Hanyang Med Rev.
2012 Nov;32(4):179-186. 10.7599/hmr.2012.32.4.179.
Calcium Metabolism and Hyper and Hypoparathyroidism
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. csshin@snu.ac.kr
- KMID: 2168207
- DOI: http://doi.org/10.7599/hmr.2012.32.4.179
Abstract
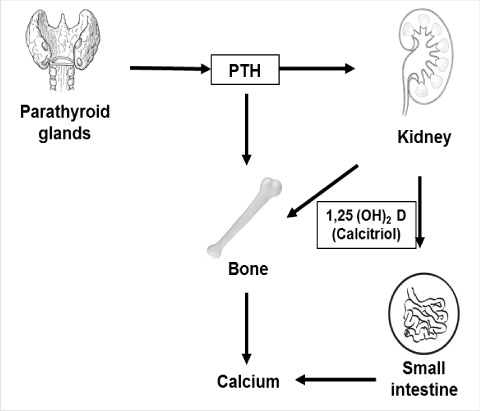
- Calcium balance refers to the state of calcium body stores which are primarily in bone, determined largely as a function of dietary intake, intestinal absorption, renal excretion, and bone remodeling. Calcium homeostasis refers to the hormonal regulation of serum ionized calcium concentrations by parathyroid hormone (PTH), the release and effect of which is dependent on the availability of 1,25-dihydroxyvitamin D, and levels of serum ionized calcium, which together regulate calcium absorption and transport in the tissues of the gut, kidney, and bone. Primary hyperparathyroidism is diagnosed on the basis of a raised PTH level in the presence of hypercalcemia. Hypoparathyroidism refers to the failure of the body to produce levels of PTH sufficient to maintain a normal level of serum calcium. Pseudo-parathyroidismis characterized by end-organ resistance to PTH which presents as hypocalcemia and hyperphosphatemias under high PTH levels.
Keyword
MeSH Terms
Figure
Reference
-
1. Peacock M. Calcium metabolism in health and disease. Clin J Am Soc Nephrol. 2010. 5 Suppl 1:S23–S30.
Article2. O'Toole JF. Disorders of calcium metabolism. Nephron Physiol. 2011. 118:p22–p27.3. Shoback D, Sellmeyer D, Bikle DD. Gardner DG, Shoback D, editors. Metabolic bone disease. Greenspan's basic & clinical endocrinology. 2011. 9th ed. New York: McGraw-Hill;227–241.4. Bringhurst FR, Demay MB, Kronenberg HM. Melmed S PK, Larsen PR, Kronengerg HM, editors. Hormones and disorders of mineral metabolism. Williams textbook of endocrinology. 2011. 12th ed. Elsevier;1257–1260.
Article5. Allgrove J. Physiology of calcium, phosphate and magnesium. Endocr Dev. 2009. 16:8–31.
Article6. Silverberg SJ, Lewiecki EM, Mosekilde L, Peacock M, Rubin MR. Presentation of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009. 94:351–365.
Article7. Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med. 2011. 365:2389–2397.8. Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, et al. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993-2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006. 21:171–177.
Article9. Cohen J, Gierlowski TC, Schneider AB. A prospective study of hyperparathyroidism in individuals exposed to radiation in childhood. JAMA. 1990. 264:581–584.
Article10. Szalat A, Mazeh H, Freund HR. Lithium-associated hyperparathyroidism: report of four cases and review of the literature. Eur J Endocrinol. 2009. 160:317–323.
Article11. Marx SJ. Hyperparathyroid genes: sequences reveal answers and questions. Endocr Pract. 2011. 17:Suppl 3. 18–27.
Article12. Rejnmark L, Vestergaard P, Mosekilde L. Nephrolithiasis and renal calcifications in primary hyperparathyroidism. J Clin Endocrinol Metab. 2011. 96:2377–2385.
Article13. Ayturk S, Gursoy A, Bascil Tutuncu N, Ertugrul DT, Guvener Demirag N. Changes in insulin sensitivity and glucose and bone metabolism over time in patients with asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab. 2006. 91:4260–4263.
Article14. Hagstrom E, Lundgren E, Lithell H, Berglund L, Ljunghall S, Hellman P, et al. Normalized dyslipidaemia after parathyroidectomy in mild primary hyperparathyroidism: population-based study over five years. Clin Endocrinol (Oxf). 2002. 56:253–260.
Article15. Walker MD, Silverberg SJ. Cardiovascular aspects of primary hyperparathyroidism. J Endocrinol Invest. 2008. 31:925–931.
Article16. Vestergaard P, Mollerup CL, Frokjaer VG, Christiansen P, Blichert-Toft M, Mosekilde L. Cohort study of risk of fracture before and after surgery for primary hyperparathyroidism. BMJ. 2000. 321:598–602.
Article17. Bilezikian JP, Khan AA, Potts JT Jr. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab. 2009. 94:335–339.
Article18. Rubin MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E, Siris E, et al. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab. 2008. 93:3462–3470.
Article19. Bollerslev J, Jansson S, Mollerup CL, Nordenstrom J, Lundgren E, Torring O, et al. Medical observation, compared with parathyroidectomy, for asymptomatic primary hyperparathyroidism: a prospective, randomized trial. J Clin Endocrinol Metab. 2007. 92:1687–1692.
Article20. Ambrogini E, Cetani F, Cianferotti L, Vignali E, Banti C, Viccica G, et al. Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial. J Clin Endocrinol Metab. 2007. 92:3114–3121.
Article21. Rao DS, Phillips ER, Divine GW, Talpos GB. Randomized controlled clinical trial of surgery versus no surgery in patients with mild asymptomatic primary hyperparathyroidism. J Clin Endocrinol Metab. 2004. 89:5415–5422.
Article22. Lowe H, McMahon DJ, Rubin MR, Bilezikian JP, Silverberg SJ. Normocalcemic primary hyperparathyroidism: further characterization of a new clinical phenotype. J Clin Endocrinol Metab. 2007. 92:3001–3005.
Article23. Soreide JA, van Heerden JA, Grant CS, Yau Lo C, Schleck C, Ilstrup DM. Survival after surgical treatment for primary hyperparathyroidism. Surgery. 1997. 122:1117–1123.
Article24. Yu N, Donnan PT, Flynn RW, Murphy MJ, Smith D, Rudman A, et al. Increased mortality and morbidity in mild primary hyperparathyroid patients. The Parathyroid Epidemiology and Audit Research Study (PEARS). Clin Endocrinol (Oxf). 2010. 73:30–34.25. Jacobs TP, Bilezikian JP. Clinical review: Rare causes of hypercalcemia. J Clin Endocrinol Metab. 2005. 90:6316–6322.26. Eastell R, Arnold A, Brandi ML, Brown EM, D'Amour P, Hanley DA, et al. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009. 94:340–350.
Article27. Silverberg SJ. Vitamin D deficiency and primary hyperparathyroidism. J Bone Miner Res. 2007. 22:suppl 2. V100–V104.
Article28. Suh JM, Cronan JJ, Monchik JM. Primary hyperparathyroidism: is there an increased prevalence of renal stone disease. AJR Am J Roentgenol. 2008. 191:908–911.
Article29. Silverberg SJ, Locker FG, Bilezikian JP. Vertebral osteopenia: a new indication for surgery in primary hyperparathyroidism. J Clin Endocrinol Metab. 1996. 81:4007–4012.
Article30. Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg. 2011. 253:585–591.
Article31. Vignali E, Picone A, Materazzi G, Steffe S, Berti P, Cianferotti L, et al. A quick intraoperative parathyroid hormone assay in the surgical management of patients with primary hyperparathyroidism: a study of 206 consecutive cases. Eur J Endocrinol. 2002. 146:783–788.
Article32. Grey AB, Stapleton JP, Evans MC, Tatnell MA, Reid IR. Effect of hormone replacement therapy on bone mineral density in postmenopausal women with mild primary hyperparathyroidism. A randomized, controlled trial. Ann Intern Med. 1996. 125:360–368.
Article33. Khan AA, Bilezikian JP, Kung AW, Ahmed MM, Dubois SJ, Ho AY, et al. Alendronate in primary hyperparathyroidism: a double-blind, randomized, placebo-controlled trial. J Clin Endocrinol Metab. 2004. 89:3319–3325.
Article34. Marcocci C, Chanson P, Shoback D, Bilezikian J, Fernandez-Cruz L, Orgiazzi J, et al. Cinacalcet reduces serum calcium concentrations in patients with intractable primary hyperparathyroidism. J Clin Endocrinol Metab. 2009. 94:2766–2772.
Article35. Bilezikian JP, Khan A, Potts JT Jr, Brandi ML, Clarke BL, Shoback D, et al. Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res. 2011. 26:2317–2337.
Article36. Chan FK, Tiu SC, Choi KL, Choi CH, Kong AP, Shek CC. Increased bone mineral density in patients with chronic hypoparathyroidism. J Clin Endocrinol Metab. 2003. 88:3155–3159.
Article37. Marx SJ. Hyperparathyroid and hypoparathyroid disorders. N Engl J Med. 2000. 343:1863–1875.
Article38. Percival RC, Hargreaves AW, Kanis JA. The mechanism of hypocalcaemia following thyroidectomy. Acta Endocrinol (Copenh). 1985. 109:220–226.
Article39. Richards ML, Thompson GB, Farley DR, Grant CS. Reoperative parathyroidectomy in 228 patients during the era of minimal-access surgery and intraoperative parathyroid hormone monitoring. Am J Surg. 2008. 196:937–942.
Article40. Eisenbarth GS, Gottlieb PA. Autoimmune polyendocrine syndromes. N Engl J Med. 2004. 350:2068–2079.
Article41. Blizzard RM, Chee D, Davis W. The incidence of parathyroid and other antibodies in the sera of patients with idiopathic hypoparathyroidism. Clin Exp Immunol. 1966. 1:119–128.42. Li Y, Song YH, Rais N, Connor E, Schatz D, Muir A, et al. Autoantibodies to the extracellular domain of the calcium sensing receptor in patients with acquired hypoparathyroidism. J Clin Invest. 1996. 97:910–914.
Article43. Thakker RV. Genetic developments in hypoparathyroidism. Lancet. 2001. 357:974–976.
Article44. Toumba M, Sergis A, Kanaris C, Skordis N. Endocrine complications in patients with Thalassaemia Major. Pediatr Endocrinol Rev. 2007. 5:642–648.45. Carpenter TO, Carnes DL Jr, Anast CS. Hypoparathyroidism in Wilson's disease. N Engl J Med. 1983. 309:873–877.
Article46. Tong GM, Rude RK. Magnesium deficiency in critical illness. J Intensive Care Med. 2005. 20:3–17.
Article47. Chase LR, Melson GL, Aurbach GD. Pseudohypoparathyroidism: defective excretion of 3',5'-AMP in response to parathyroid hormone. J Clin Invest. 1969. 48:1832–1844.
Article48. Weinstein LS, Yu S, Warner DR, Liu J. Endocrine manifestations of stimulatory G protein alpha-subunit mutations and the role of genomic imprinting. Endocr Rev. 2001. 22:675–705.
Article49. Bastepe M. The GNAS locus and pseudohypoparathyroidism. Adv Exp Med Biol. 2008. 626:27–40.
Article50. Mantovani G, de Sanctis L, Barbieri AM, Elli FM, Bollati V, Vaira V, et al. Pseudohypoparathyroidism and GNAS epigenetic defects: clinical evaluation of albright hereditary osteodystrophy and molecular analysis in 40 patients. J Clin Endocrinol Metab. 2010. 95:651–658.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypoparathyroidism in children and adolescents
- Bilateral Striopallidodentate Calcinosis in Chromosome 22q11.2 Deletion Syndrome
- A Case of the Milk-alkali Syndrome During Management of Idiopathic Hypoparathyroidism
- De novo a novel variant of CaSR gene in a neonate with congenital hypoparathyroidism
- Hypoparathyroidism: Replacement Therapy with Parathyroid Hormone