Cancer Res Treat.
2007 Mar;39(1):10-15.
Laparoscopic Assisted Distal Rectal Cancer Resection with Preoperative Concurrent Chemoradiotherapy
- Affiliations
-
- 1Department of Surgery, Hallym University College of Medicine, Anyang, Korea. bshlee@hallym.or.kr, bl2262@columibia.edu
- 2Department of Radiation Therapy, Hallym University College of Medicine, Anyang, Korea.
- 3Department of Internal Medicine, Hallym University College of Medicine, Anyang, Korea.
- 4Department of Surgery, Columbia University, New York, USA.
Abstract
-
PURPOSE: Anatomy of deep pelvis, narrow distal margin and tumor invasion into neighbor organ are obstacles for curative radical resection for advanced cancer of distal rectum. Technically, laparoscopic application after downstaging the tumor with preoperative concurrent chemotherapy (CCRT) may give a solution to overcome the anatomical difficulties. We compared the results of laparoscopic surgery in the patients who received CCRT with those of patients who had conventional surgery.
MATERIALS AND METHODS
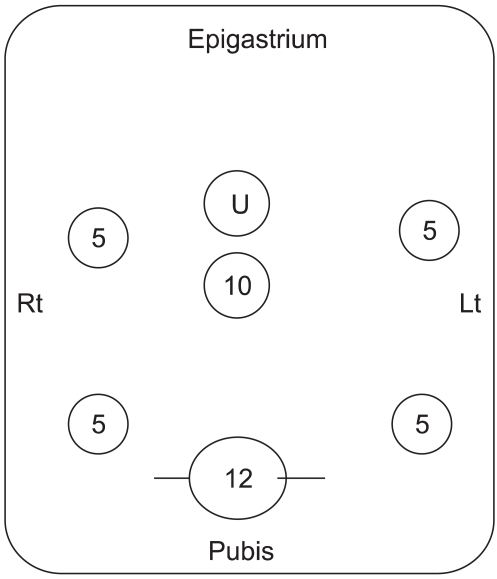
A continuous infusion of 5FU plus leucovorin and radiotherapy (50.4 Gy) in 28 fractions was given each patient as CCRT. They underwent D2 radical resection with TME and ANP for the rectal cancer in 4 weeks.
RESULTS
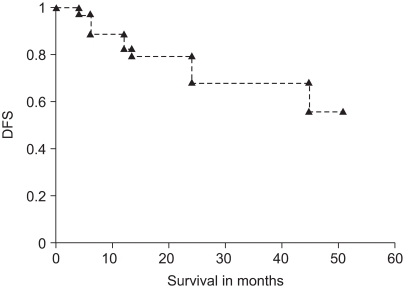
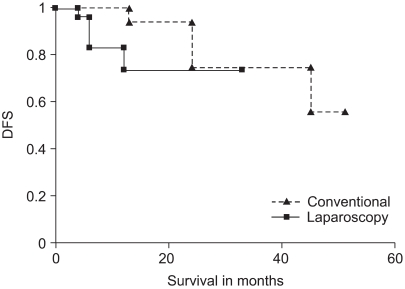
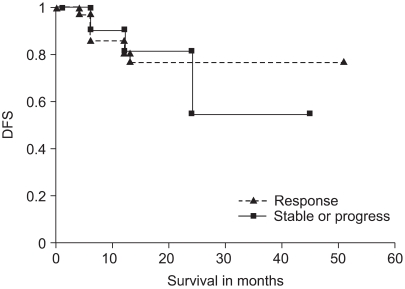
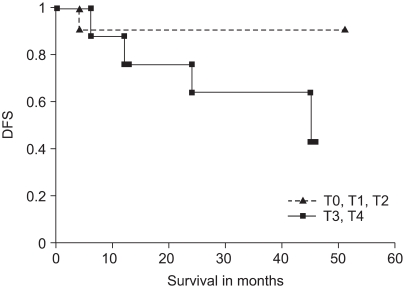
Thirty three patients had laparoscopic resection such as LAR, colo-anal anastomosis and APR. The results were compared with 12 cases of the conventional resections. As a result of preoperative CCRT, the cancer was down-staged in 71%. Two year disease free survival was 75% and 74% in the group of conventional and laparoscopic resection, respectively (p=0.427). Ileus, voiding difficulty and leakage after surgery were not different between two groups. Weakness of ejaculation was noted in 9~11% of both groups. The DFS of the preoperative CCRT followed by radical resection in the groups with a response was more favorable than that in the group with progressive or stable disease.
CONCLUSION
Radical resection of advanced distal rectal cancer could be done with performing a laparoscopic assisted operation after CCRT induced down-staging. We may suggest that laparoscopic assisted resection is a good treatment option as it doesn't increase the complications and it has a compatible survival rate to conventional surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Weiser MR, Milsom JW. Laparoscopic total mesorectal excision with autonomic nerve preservation. Semin Surg Oncol. 2000; 19:396–403. PMID: 11241922.
Article2. Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic L, et al. EORTC Radiotherapy Group Trial 22921. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006; 355:1114–1123. PMID: 16971718.
Article3. Rödel C, Sauer R. Perioperative radiotherapy and concurrent radiochemotherapy in rectal cancer. Semin Surg Oncol. 2001; 20:3–12. PMID: 11291127.
Article4. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000; 92:205–216. PMID: 10655437.
Article5. Brown CL, Ternent CA, Thorson AG, Christensen MA, Blatchford GJ, Shashidharan M, et al. Response to preoperative chemoradiation in Stage II and III rectal cancer. Dis Colon Rectum. 2003; 46:1189–1193. PMID: 12972962.
Article6. Theodoropoulos G, Wise WE, Padmanabhan A, Kerner BA, Taylor CW, Aguilar PS, et al. T-level downstaging and complete pathologic response after preoperative chemoradiation for advanced rectal cancer result in decreased recurrence and improved disease-free survival. Dis Colon Rectum. 2002; 45:895–903. PMID: 12130878.
Article7. Kim YW, Kim NK, Min BS, Pyo J, Kim H, Cha SH, et al. Accuracy of magnetic resonance imaging in predicting TNM staging and circumferential resection margin compared with pathologic assessment on whole-mount section in rectal cancer. J Korean Soc Coloproctol. 2006; 22:402–410.8. Dworak O, Keilholz L, Hoffmann A. Pathological features of rectal cancer after preoperative radiochemotherapy. Int J Colorectal Dis. 1997; 12:19–23. PMID: 9112145.
Article9. Ghadimi BM, Grade M, Difilippantoni MJ, Varma S, Simon R, Montagna C, et al. Effectiveness of gene expression profiling for response prediction of rectal adenocarcinoma to preoperative chemotherapy. J Clin Oncol. 2005; 23:1826–1836. PMID: 15774776.10. Lee HS, Kim WH. Tissue array methods for high-throughput clinicopathologic research. Cancer Res Treat. 2006; 38:1–6.
Article11. Watanabe T, Wu TT, Catalano PJ, Ueki T, Satriano R, Haller DG. Molecular predictors of survival after adjuvant chemotherapy for colon cancer. N Engl J Med. 2001; 344:1196–1206. PMID: 11309634.
Article12. Stein DE, Mahmoud NN, Anne PR, Rose DG, Isenberg GA, Goldstein SD, et al. Longer time interval between completion of neoadjuvant chemoradiation and surgical resection does not improve downstaging of rectal carcinoma. Dis Colon Rectum. 2003; 46:448–453. PMID: 12682535.
Article13. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer. Lancet Oncol. 2005; 6:477–484. PMID: 15992696.14. Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350:2050–2059. PMID: 15141043.15. Raa ST, Oosterling SJ, van der Kaaij NP, van den Tol MP, Beelen RH, Meijers S, et al. Surgery promotes implantation of disseminated tumor cells, but does not increase growth of tumor cell clusters. J Surg Oncol. 2005; 92:124–129. PMID: 16231370.
Article16. Larach SW, Gallagher JT. Complications of laparoscopic surgery for rectal cancer: avoidance and management. Semin Surg Oncol. 2000; 18:265–268. PMID: 10757893.
Article17. Holte K, Kehlet H. Postoperative ileus; preventable event. Br J Surg. 2000; 87:1480–1493. PMID: 11091234.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Preoperative Concurrent Chemoradiotherapy with Oral Fluoropyrimidine in Locally Advanced Rectal Cancer: How Good Is Good Enough?
- Simultaneous Laparoscopic Resection of Advanced Colorectal Cancer and Early Gastric Cancer
- Results of Preoperative Chemoradiotherapy in Low Rectal Cancer
- Efficacy of preoperative chemoradiotherapy in patients with cT2N0 distal rectal cancer