Ann Rehabil Med.
2015 Dec;39(6):1002-1010. 10.5535/arm.2015.39.6.1002.
Diagnostic Value of Elevated D-Dimer Level in Venous Thromboembolism in Patients With Acute or Subacute Brain Lesions
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. rootpmr@catholic.ac.kr
- KMID: 2165628
- DOI: http://doi.org/10.5535/arm.2015.39.6.1002
Abstract
OBJECTIVE
To define the risk factors that influence the occurrence of venous thromboembolism (VTE) in patients with acute or subacute brain lesions and to determine the usefulness of D-dimer levels for VTE screening of these patients.
METHODS
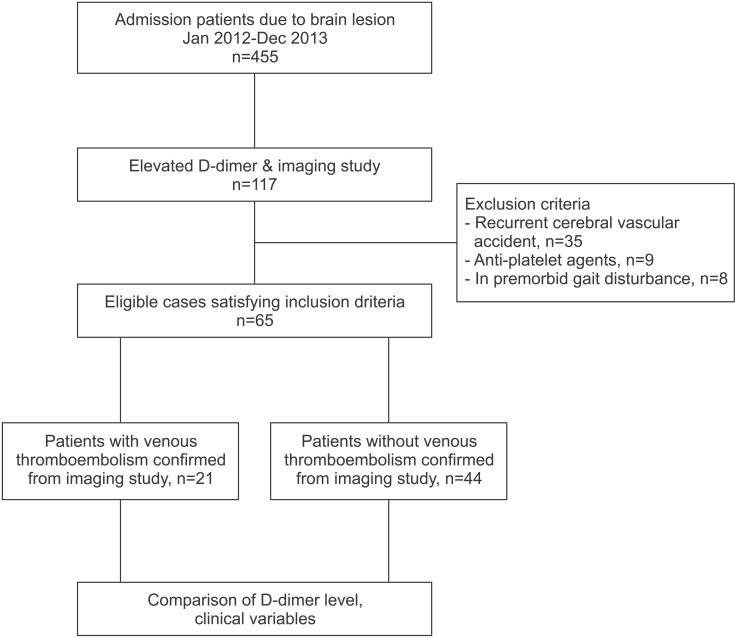
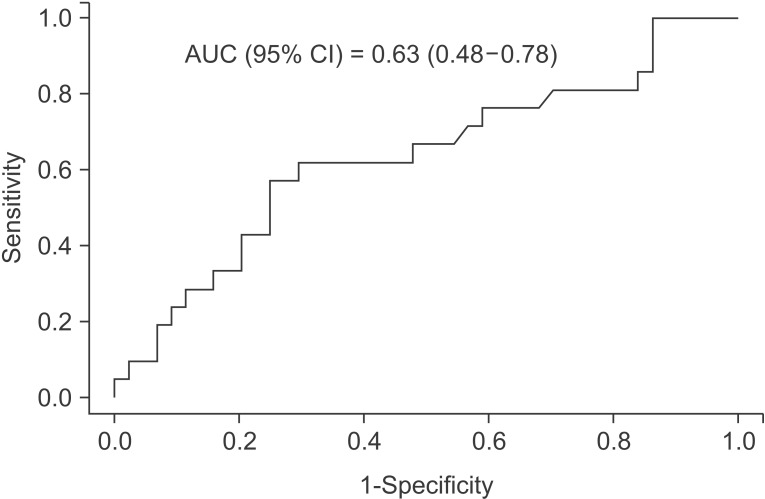
Medical data from January 2012 to December 2013 were retrospectively reviewed. Mean D-dimer levels in those with VTE versus those without VTE were compared. Factors associated with VTE were analyzed and the odds ratios (ORs) were calculated. The D-dimer cutoff value for patients with hemiplegia was defined using a receiver operating characteristic (ROC) curve.
RESULTS
Of 117 patients with acute or subacute brain lesions, 65 patients with elevated D-dimer levels (mean, 5.1+/-5.8 mg/L; positive result >0.55 mg/L) were identified. Logistic regression analysis showed that the risk of VTE was 3.9 times higher in those with urinary tract infections (UTIs) (p=0.0255). The risk of VTE was 4.5 times higher in those who had recently undergone surgery (p=0.0151). Analysis of the ROC showed 3.95 mg/L to be the appropriate D-dimer cutoff value for screening for VTE (area under the curve [AUC], 0.63; 95% confidence interval [CI], 0.5-0.8) in patients with acute or subacute brain lesions. This differs greatly from the conventional D-dimer cutoff value of 0.55 mg/L. D-dimer levels less than 3.95 mg/L in the absence of surgery showed a negative predictive value of 95.8% (95% CI, 78.8-99.8).
CONCLUSION
Elevated D-dimer levels alone have some value in VTE diagnosis. However, the concomitant presence of UTI or a history of recent surgery significantly increased the risk of VTE in patients with acute or subacute brain lesions. Therefore, a different D-dimer cutoff value should be applied in these cases.
MeSH Terms
Figure
Reference
-
1. Brandstater ME, Roth EJ, Siebens HC. Venous thromboembolism in stroke: literature review and implications for clinical practice. Arch Phys Med Rehabil. 1992; 73(5-S):S379–S391. PMID: 1301012.2. Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994; 331:1601–1606. PMID: 7969340.
Article3. Hong MY, Lee C, Yoo SY, Shin DH, Cheong SS, Kwon JH, et al. Cut-off value and factors associated with a false positive D-dimer result for venous thromboembolism in Koreans. Korean J Med. 2013; 84:372–378.
Article4. Schrecengost JE, LeGallo RD, Boyd JC, Moons KG, Gonias SL, Rose CE Jr, et al. Comparison of diagnostic accuracies in outpatients and hospitalized patients of D-dimer testing for the evaluation of suspected pulmonary embolism. Clin Chem. 2003; 49:1483–1490. PMID: 12928229.
Article5. Sadovsky R. ELISA D-dimer testing: high sensitivity but low specificity. Am Fam Physician. 2002; 66:2310.6. Darwood RJ, Smith FC. Deep vein thrombosis. Surgery (Oxford). 2013; 31:206–210.
Article7. Jiang Y, Li J, Liu Y, Li YC, Zhang WG. Risk factors for deep vein thrombosis after orthopedic surgery and the diagnostic value of D-dimer. Ann Vasc Surg. 2015; 29:675–681. PMID: 25728333.
Article8. Matsumoto M, Sakaguchi M, Okazaki S, Furukado S, Tagaya M, Etani H, et al. Relationship between plasma (D)-dimer level and cerebral infarction volume in patients with nonvalvular atrial fibrillation. Cerebrovasc Dis. 2013; 35:64–72. PMID: 23428999.
Article9. Park YW, Koh EJ, Choi HY. Correlation between serum D-dimer level and volume in acute Ischemic stroke. J Korean Neurosurg Soc. 2011; 50:89–94. PMID: 22053225.
Article10. Prell J, Rachinger J, Smaczny R, Taute BM, Rampp S, Illert J, et al. D-dimer plasma level: a reliable marker for venous thromboembolism after elective craniotomy. J Neurosurg. 2013; 119:1340–1346. PMID: 23915033.
Article11. Park JH, Kwon YC. Standardization of Korean version of the Mini-Mental State Examination (MMSE-K) for use in the elderly. Part II: diagnostic validity. J Korean Neuropsychiatr Assoc. 1989; 28:508–513.12. Lee HJ, Choi HY, Yun KW, Kim YC, Lim WJ, Kim JH, et al. Association between obesity indices and MMSE-K in elderly. J Korean Neuropsychiatr Assoc. 2013; 52:447–453.
Article13. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–297.14. Kim EJ, Kim SS, Kim WH, Lee WJ, Nam KY, Park CW, et al. The selection of exercise stress test in hemiplegic patients. J Korean Acad Rehabil Med. 2008; 32:26–31.15. Ramanan B, Gupta PK, Sundaram A, Lynch TG, Mac-Taggart JN, Baxter BT, et al. In-hospital and postdischarge venous thromboembolism after vascular surgery. J Vasc Surg. 2013; 57:1589–1596. PMID: 23395207.
Article16. Jeong HS, Miller TJ, Davis K, Matthew A, Lysikowski J, Lazcano E, et al. Application of the Caprini risk assessment model in evaluation of non-venous thromboembolism complications in plastic and reconstructive surgery patients. Aesthet Surg J. 2014; 34:87–95. PMID: 24327763.
Article17. Cho KH, Kim KP, Woo BC, Kim YJ, Park JY, Cho SY, et al. Relationship between blood stasis syndrome score and cardioankle vascular index in stroke patients. Evid Based Complement Alternat Med. 2012; 2012:696983. PMID: 22701508.
Article18. Chua K, Kong KH, Chan SP. Prevalence and risk factors of asymptomatic lower extremity deep venous thrombosis in Asian neurorehabilitation admissions in Singapore. Arch Phys Med Rehabil. 2008; 89:2316–2323. PMID: 19061744.
Article19. Sachdev U, Teodorescu VJ, Shao M, Russo T, Jacobs TS, Silverberg D, et al. Incidence and distribution of lower extremity deep vein thrombosis in rehabilitation patients: implications for screening. Vasc Endovascular Surg. 2006; 40:205–211. PMID: 16703208.
Article20. Yablon SA, Rock WA Jr, Nick TG, Sherer M, McGrath CM, Goodson KH. Deep vein thrombosis: prevalence and risk factors in rehabilitation admissions with brain injury. Neurology. 2004; 63:485–491. PMID: 15304579.
Article21. Cifu DX, Kaelin DL, Wall BE. Deep venous thrombosis: incidence on admission to a brain injury rehabilitation program. Arch Phys Med Rehabil. 1996; 77:1182–1185. PMID: 8931533.
Article22. Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet. 2006; 367:1075–1079. PMID: 16581406.
Article23. Clayton TC, Gaskin M, Meade TW. Recent respiratory infection and risk of venous thromboembolism: case-control study through a general practice database. Int J Epidemiol. 2011; 40:819–827. PMID: 21324940.
Article24. Fujita Y, Nakatsuka H, Namba Y, Mitani S, Yoshitake N, Sugimoto E, et al. The incidence of pulmonary embolism and deep vein thrombosis and their predictive risk factors after lower extremity arthroplasty: a retrospective analysis based on diagnosis using multidetector CT. J Anesth. 2015; 29:235–241. PMID: 25097087.
Article25. Kimmell KT, Jahromi BS. Clinical factors associated with venous thromboembolism risk in patients undergoing craniotomy. J Neurosurg. 2015; 122:1004–1011. PMID: 25495743.
Article26. Kim JY, Khavanin N, Rambachan A, McCarthy RJ, Mlodinow AS, De Oliveria GS Jr, et al. Surgical duration and risk of venous thromboembolism. JAMA Surg. 2015; 150:110–117. PMID: 25472485.
Article27. Legnani C, Palareti G, Cosmi B, Cini M, Tosetto A, Tripodi A, et al. Different cut-off values of quantitative D-dimer methods to predict the risk of venous thromboembolism recurrence: a post-hoc analysis of the PROLONG study. Haematologica. 2008; 93:900–907. PMID: 18443269.
Article28. Pulivarthi S, Gurram MK. Effectiveness of d-dimer as a screening test for venous thromboembolism: an update. N Am J Med Sci. 2014; 6:491–499. PMID: 25489560.29. Hu X, Fang Y, Ye F, Lin S, Li H, You C, et al. Effects of plasma D-dimer levels on early mortality and longterm functional outcome after spontaneous intracerebral hemorrhage. J Clin Neurosci. 2014; 21:1364–1367. PMID: 24631325.
Article30. Stein J, Brandstater ME. Stroke rehabilitation. In : Frontera WR, DeLisa JA, editors. DeLisa's physical medicine & rehabilitation: principles and practice. 5th ed. Philadelphia: Lippincott Williams & Wilkins;2010. p. 551–574.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT Findings of Disease with Elevated Serum D-Dimer Levels in an Emergency Room Setting
- Cutoff Values of Plasma D-Dimer Level in Patients with Diagnosis of the Venous Thromboembolism after Elective Spinal Surgery
- Serum D-dimer should not be used in the diagnosis of venous thromboembolism within 28 days of total knee replacement surgery
- D-Dimer Testing in Laboratory Practice
- Cut-Off Value and Factors Associated with a False Positive D-Dimer Result for Venous Thromboembolism in Koreans