J Korean Med Sci.
2015 Aug;30(8):1042-1047. 10.3346/jkms.2015.30.8.1042.
Predictors of Asthma Control by Stepwise Treatment in Elderly Asthmatic Patients
- Affiliations
-
- 1Department of Allergy and Clinical Immunology, Ajou University School of Medicine, Suwon, Korea. hspark@ajou.ac.kr
- 2Department of Preventive Medicine & Public Health, Ajou University School of Medicine, Suwon, Korea.
- 3Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 4Department of Internal Medicine, Dong-A University School of Medicine, Busan, Korea.
- 5Department of Internal Medicine, Hallym University School of Medicine, Anyang, Korea.
- 6Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2164497
- DOI: http://doi.org/10.3346/jkms.2015.30.8.1042
Abstract
- The geriatric population is increasing, and asthma severity increases with age. We determined the predictors of asthma control, exacerbation, and the factors that affect asthma-specific quality of life (A-QOL) in elderly asthmatic patients. This was a prospective, multicenter, real-life study for 6 months with stepwise pharmacologic treatment based on the Global Initiative for Asthma (GINA) guideline. A total of 296 asthmatic patients aged > or = 60 yr were recruited from 5 university centers in Korea. The improved-asthma control group was defined as the group of patients who maintained well-controlled or improved disease and the not-improved asthma control group was defined as the remaining patients. Fewer number of medications for comorbidities (2.8 +/- 3.3 in the improved vs. 4.5 +/- 4.4 in the control) and higher physical functioning (PF) scale (89.8 +/- 14.2 in the improved vs. 82.0 +/- 16.4 in the control) were significant predictors in the improved-asthma control group (OR = 0.863, P = 0.004 and OR = 1.028, P = 0.018, respectively). An asthma control test (ACT) score of < or = 19 at baseline was a significant predictor of asthma exacerbation (OR = 3.938, P = 0.048). Asthma duration (F = 5.656, P = 0.018), ACT score (F = 12.237, P = 0.001) at baseline, and the presence of asthma exacerbation (F = 5.565, P = 0.019) were significant determinants of changes in A-QOL. The number of medications for comorbidities and performance status determined by the PF scale may be important parameters for assessing asthma control in elderly asthmatic patients.
Keyword
MeSH Terms
-
Aged
Aged, 80 and over
Anti-Asthmatic Agents/*administration & dosage
Asthma/*diagnosis/epidemiology/*therapy
Critical Pathways/statistics & numerical data
Dose-Response Relationship, Drug
Female
Geriatric Assessment/*methods/statistics & numerical data
Humans
Male
Middle Aged
Outcome Assessment (Health Care)/*methods
*Quality of Life
Reproducibility of Results
Republic of Korea/epidemiology
Sensitivity and Specificity
Treatment Outcome
Anti-Asthmatic Agents
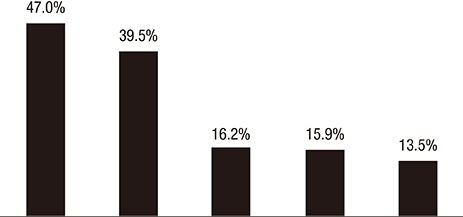
Figure
Cited by 2 articles
-
Impact of cognitive impairment on asthma control in older asthmatics
Gyu-Young Hur, Young-Min Ye, So Young Moon, Joo-Hee Kim, Ki-Suck Jung, Hae-Sim Park
Allergy Asthma Respir Dis. 2017;5(1):34-40. doi: 10.4168/aard.2017.5.1.34.Multifaceted interventions to reduce acute exacerbations in elderly asthmatics
So-Hee Lee, Woo-Jung Song, Heung-Woo Park, Min-Gyu Kang, Sae-Hoon Kim, Hye-Kyung Park, Sang-Heon Kim, Yong-Eun Kwon, Tae-Bum Kim, Byung-Jae Lee, Young-Koo Jee, Byung-Whui Choi, Sang-Heon Cho, Sun-Sin Kim
Asia Pac Allergy. 2018;8(1):. doi: 10.5415/apallergy.2018.8.e1.
Reference
-
1. Hanania NA, King MJ, Braman SS, Saltoun C, Wise RA, Enright P, Falsey AR, Mathur SK, Ramsdell JW, Rogers L, et al. Asthma in Elderly workshop participants. Asthma in Elderly workshop participants. Asthma in the elderly: Current understanding and future research needs--a report of a National Institute on Aging (NIA) workshop. J Allergy Clin Immunol. 2011; 128:S4–S24.2. Statistics Korea. Population projections. 2014. Available at https://www.index.go.kr/egams/stts/jsp/potal/stts/PO_STTS_IdxMain.jsp?idx_cd=1010&bbs=INDX_001.3. Reed CE. Asthma in the elderly: diagnosis and management. J Allergy Clin Immunol. 2010; 126:681–687. quiz 688-94. Tsai CL, Delclos GL, Huang JS, Hanania NA, Camargo CA Jr. Age-related differences in asthma outcomes in the United States, 1988-2006. Ann Allergy Asthma Immunol. 2013; 110:240–246. 246.e15. Yáñez A, Cho SH, Soriano JB, Rosenwasser LJ, Rodrigo GJ, Rabe KF, Peters S, Niimi A, Ledford DK, Katial R, et al. Asthma in the elderly: what we know and what we have yet to know. World Allergy Organ J. 2014; 7:8.6. Jones SC, Iverson D, Burns P, Evers U, Caputi P, Morgan S. Asthma and ageing: an end user's perspective--the perception and problems with the management of asthma in the elderly. Clin Exp Allergy. 2011; 41:471–481.7. Mäkelä MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013; 107:1481–1490.8. Goeman DP, Douglass JA. Optimal management of asthma in elderly patients: strategies to improve adherence to recommended interventions. Drugs Aging. 2007; 24:381–394.9. Schatz M. Predictors of asthma control: what can we modify? Curr Opin Allergy Clin Immunol. 2012; 12:263–268.10. Global Initiative for Asthma. Global strategy for asthma management and prevention 2014 (revision). 2014. accessed on May 14 2014. Available at http://www.ginasthma.org/documents/4.11. Braido F, Bousquet PJ, Brzoza Z, Canonica GW, Compalati E, Fiocchi A, Fokkens W, Gerth van Wijk R, La Grutta S, Lombardi C, et al. Specific recommendations for PROs and HRQoL assessment in allergic rhinitis and/or asthma: a GA(2)LEN taskforce position paper. Allergy. 2010; 65:959–968.12. Lee EH, Kim SH, Choi JH, Jee YK, Nahm DH, Park HS. Development and evaluation of an Asthma-Specific Quality of Life (A-QOL) questionnaire. J Asthma. 2009; 46:716–721.13. WHO Collaborating Center for Drug Statistics Methodology. Updates included in the ATC/DDD Index. accessed on May 14 2014. Available at http://www.whocc.no/atc_ddd_index/?code=A&showdescription=yes.14. Hwang EK, Jin HJ, Nam YH, Shin YS, Ye YM, Nahm DH, Park HS. The predictors of poorly controlled asthma in elderly. Allergy Asthma Immunol Res. 2012; 4:270–276.15. Lee YH, Lee KJ, Han GS, Yoon SJ, Lee YK, Kim CH, Kim JL. The development of physical functioning scale for community-dwelling older persons. Korean J Prev Med. 2002; 35:359–374.16. Lee H, Kahng S, Lee J. The effects of socioeconomic position and health behavior on geriatric depressive symptom. J Korean Gerontol Soc. 2008; 28:1129–1145.17. Krauskopf KA, Sofianou A, Goel MS, Wolf MS, Wilson EA, Martynenko ME, Halm EA, Leventhal H, Feldman JM, Federman AD, et al. Depressive symptoms, low adherence, and poor asthma outcomes in the elderly. J Asthma. 2013; 50:260–266.18. Park J, Kim TB, Joo H, Lee JS, Lee SD, Oh YM. Diseases concomitant with asthma in middle-aged and elderly subjects in Korea: a population-based study. Allergy Asthma Immunol Res. 2013; 5:16–25.19. Ross JA, Yang Y, Song PX, Clark NM, Baptist AP. Quality of life, health care utilization, and control in older adults with asthma. J Allergy Clin Immunol Pract. 2013; 1:157–162.20. Jee YK. Comorbid diseases in adult asthma. Allergy Asthma Immunol Res. 2013; 5:1–2.21. Kim YH, Lee MK, Lee SJ, Cho MS, Hwang MS. Medication status and adherence of the elderly under home care nursing. J Korean Acad Community Health Nurs. 2011; 22:290–301.22. Morales DR, Jackson C, Lipworth BJ, Donnan PT, Guthrie B. Adverse respiratory effect of acute beta-blocker exposure in asthma: a systematic review and meta-analysis of randomized controlled trials. Chest. 2014; 145:779–786.23. Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007; 5:345–351.24. Enright PL. The diagnosis and management of asthma is much tougher in older patients. Curr Opin Allergy Clin Immunol. 2002; 2:175–181.25. Guilbert TW, Garris C, Jhingran P, Bonafede M, Tomaszewski KJ, Bonus T, Hahn RM, Schatz M. Asthma that is not well-controlled is associated with increased healthcare utilization and decreased quality of life. J Asthma. 2011; 48:126–132.26. Wilson SR, Rand CS, Cabana MD, Foggs MB, Halterman JS, Olson L, Vollmer WM, Wright RJ, Taggart V. Asthma outcomes: quality of life. J Allergy Clin Immunol. 2012; 129:S88–S123.27. Choi JY, Hwang SY. Factors associated with health-related quality of life among low-compliant asthmatic adults in Korea. Res Nurs Health. 2009; 32:140–147.28. Gold DA. An examination of instrumental activities of daily living assessment in older adults and mild cognitive impairment. J Clin Exp Neuropsychol. 2012; 34:11–34.29. Guilbert TW, Garris C, Jhingran P, Bonafede M, Tomaszewski KJ, Bonus T, Hahn RM, Schatz M. Asthma that is not well-controlled is associated with increased healthcare utilization and decreased quality of life. J Asthma. 2011; 48:126–132.30. Lowery EP, Henneberger PK, Rosiello R, Sama SR, Preusse P, Milton DK. Quality of life of adults with workplace exacerbation of asthma. Qual Life Res. 2007; 16:1605–1613.