J Korean Foot Ankle Soc.
2016 Mar;20(1):1-5. 10.14193/jkfas.2016.20.1.1.
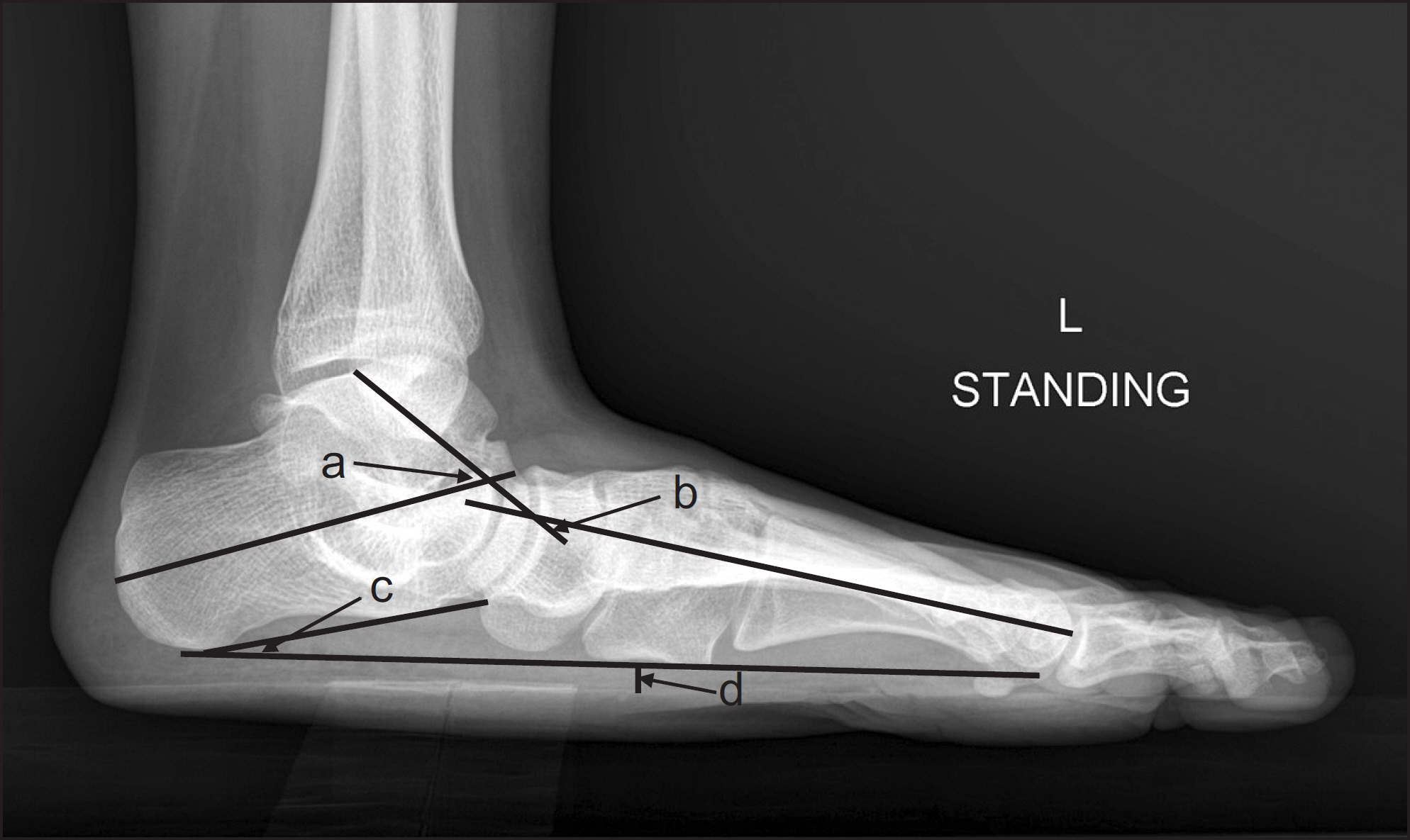
Diagnosis of Flatfoot Deformity
- Affiliations
-
- 1Department of Orthopedic Surgery, Guro Hospital, Korea University College of Medicine, Seoul, Korea. dakjul@hanmail.net
- KMID: 2158420
- DOI: http://doi.org/10.14193/jkfas.2016.20.1.1
Abstract
- Flatfoot is defined as loss of medial arch with hindfoot valgus, but normal condition is obscure due to wide individual variance. Loss or decreasing of medial longitudinal arch with radiographic image is clinically diagnosed as flatfoot. Flatfoot without symptoms is not an indication for treatment. The etiologies of flatfoot are congenital cause, hypermobility, tarsal coalition, neuromuscular disease, posttraumatic deformity, Charcot arthropathy, and posterior tibial tendon dysfuction. The flatfoot is classified as congenital and acquired, flexible, and rigid. The diagnosis is made by physical examination and radiographic findings. In particular, the posterior tibial tendon dysfunction is known as adult acquired flatfoot.
MeSH Terms
Figure
Cited by 1 articles
-
Relationships Between Self-awareness and Clinical Diagnostic Findings of Abnormal Foot Arch Height in Koreans
Youngsuk Son, Hyo Jeong Kang, Yun-Mi Song, Ji Hye Hwang
Ann Rehabil Med. 2017;41(6):1013-1018. doi: 10.5535/arm.2017.41.6.1013.
Reference
-
References
1. Rose GK, Welton EA, Marshall T. The diagnosis of flat foot in the child. J Bone Joint Surg Br. 1985; 67:71–8.
Article2. Harris EJ, Vanore JV, Thomas JL, Kravitz SR, Mendelson SA, Mendicino RW, et al. Clinical Practice Guideline Pediatric Flatfoot Panel of the American College of Foot and Ankle Surgeons. Diagnosis and treatment of pediatric flatfoot. J Foot Ankle Surg. 2004; 43:341–73.
Article3. Staheli LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am. 1987; 69:426–8.4. Anderson M, Blais MM, Green WT. Lengths of the growing foot. J Bone Joint Surg Am. 1956; 38:998–1000.5. Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 1989; 239:196–206.
Article6. Dyal CM, Feder J, Deland JT, Thompson FM. Pes planus in patients with posterior tibial tendon insufficiency: asymptomatic versus symptomatic foot. Foot Ankle Int. 1997; 18:85–8.
Article7. Ferciot CF. The etiology of developmental flatfoot. Clin Orthop Relat Res. 1972; 85:7–10.
Article8. Miller M, Dobbs MB. Congenital vertical talus: etiology and management. J Am Acad Orthop Surg. 2015; 23:604–11.9. Lee MS, Vanore JV, Thomas JL, Catanzariti AR, Kogler G, Kravitz SR, et al. Clinical Practice Guideline Adult Flatfoot Panel. Diagnosis and treatment of adult flatfoot. J Foot Ankle Surg. 2005; 44:78–113.
Article10. Kim SJ, Lee BG, Sung IH. Adult flatfoot. J Korean Med Assoc. 2014; 57:243–52.
Article11. Sung KS, Yu IS. Acquired adult flatfoot: pathophysiology, diagnosis, and nonoperative treatment. J Korean Foot Ankle Soc. 2014; 18:87–92.
Article12. Ahn CY, Ahn JH, Kim MS. Operative treatment of acquired adult flatfoot. J Korean Foot Ankle Soc. 2014; 18:93–9.
Article13. Durrant B, Chockalingam N, Morriss-Roberts C. Assessment and diagnosis of posterior tibial tendon dysfunction: do we share the same opinions and beliefs? J Am Podiatr Med Assoc. Published online July 22. 2015. doi: 10.7547/14–12211.
Article14. Sullivan JA, Miller WA. The relationship of the accessory navicular to the development of the flat foot. Clin Orthop Relat Res. 1979; 144:233–7.
Article15. Kiter E, Günal I, Karatosun V, Korman E. The relationship between the tibialis posterior tendon and the accessory navicular. Ann Anat. 2000; 182:65–8.
Article16. Arnoldner MA, Gruber M, Syré S, Kristen KH, Trnka HJ, Kain-berger F, Bodner G. Imaging of posterior tibial tendon dysfunction: comparison of high-resolution ultrasound and 3T MRI. Eur J Radiol. 2015; 84:1777–81.17. Chadha H, Pomeroy G, Manoli A 2nd. Radiologic signs of unilateral pes planus. Foot Ankle Int. 1997; 18:603–4.
Article18. Hsu TC, Wang CL, Wang TG, Chiang IP, Hsieh FJ. Ultrasonographic examination of the posterior tibial tendon. Foot Ankle Int1. 1997; 18:34–8.
Article19. Niki H, Ching RP, Kiser P, Sangeorzan BJ. The effect of posterior tibial tendon dysfunction on hindfoot kinematics. Foot Ankle Int. 2001; 22:292–300.
Article20. Park H, Hwang JH, Seo JO, Kim HW. The relationship between accessory navicular and flat foot: a radiologic study. J Pediatr Orthop. 2015; 35:739–45.