Ann Dermatol.
2009 Nov;21(4):345-351. 10.5021/ad.2009.21.4.345.
Clinical and Immunohistochemical Characteristics of Mucoceles
- Affiliations
-
- 1Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea. cjpark777@yahoo.co.kr
- KMID: 2156495
- DOI: http://doi.org/10.5021/ad.2009.21.4.345
Abstract
- BACKGROUND
Mucoceles have diverse clinical and histological features. Their pathogenesis remains to be elucidated.
OBJECTIVE
To determine the structural and/or pathogenic differences between two clinically different types of mucoceles.
METHODS
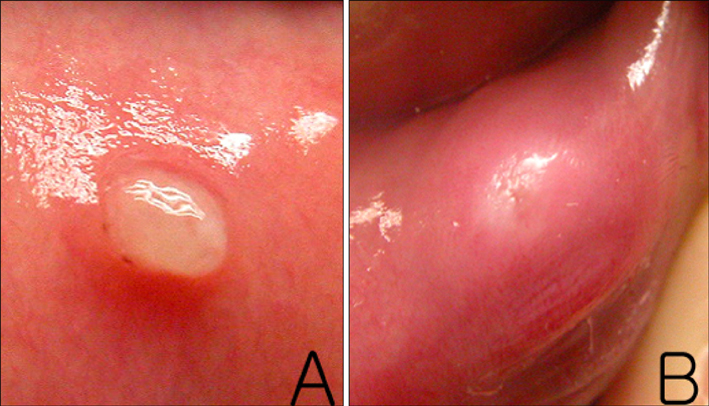
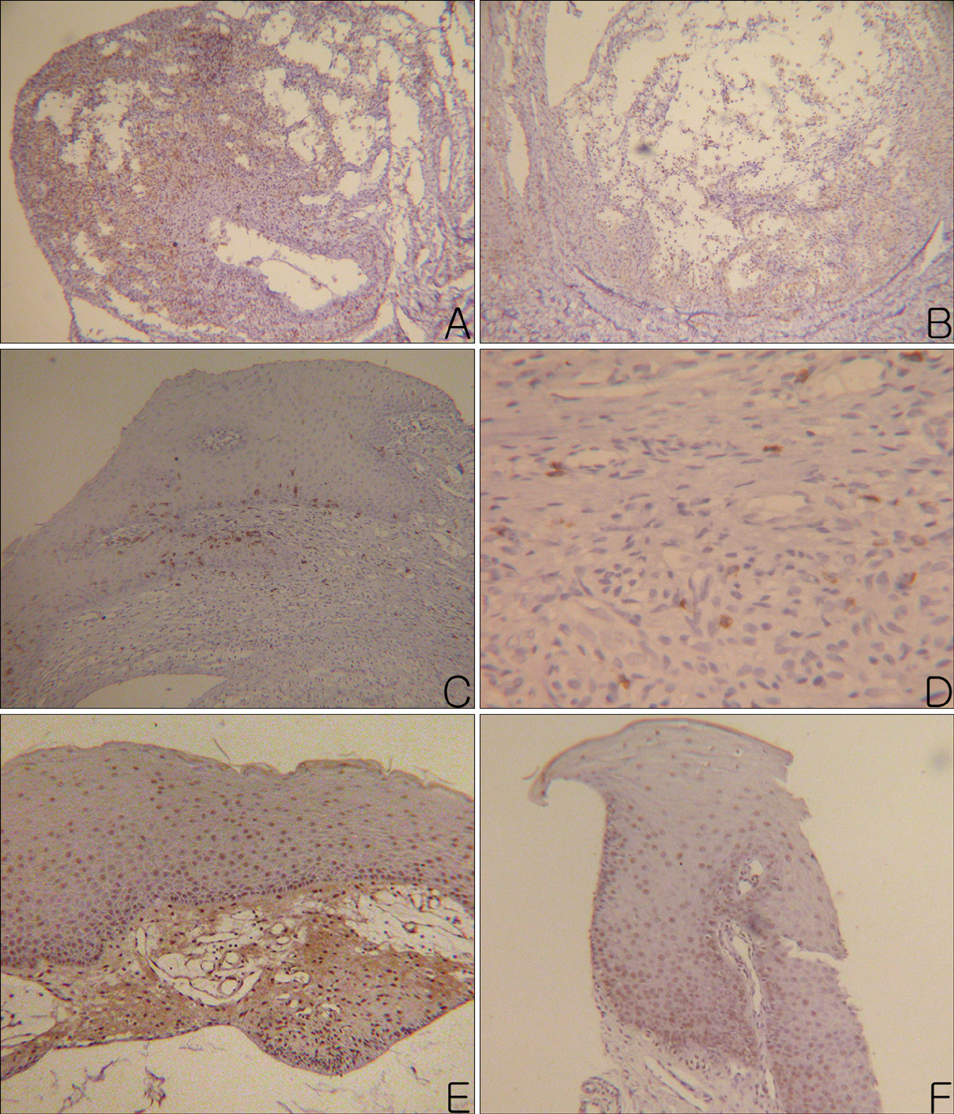
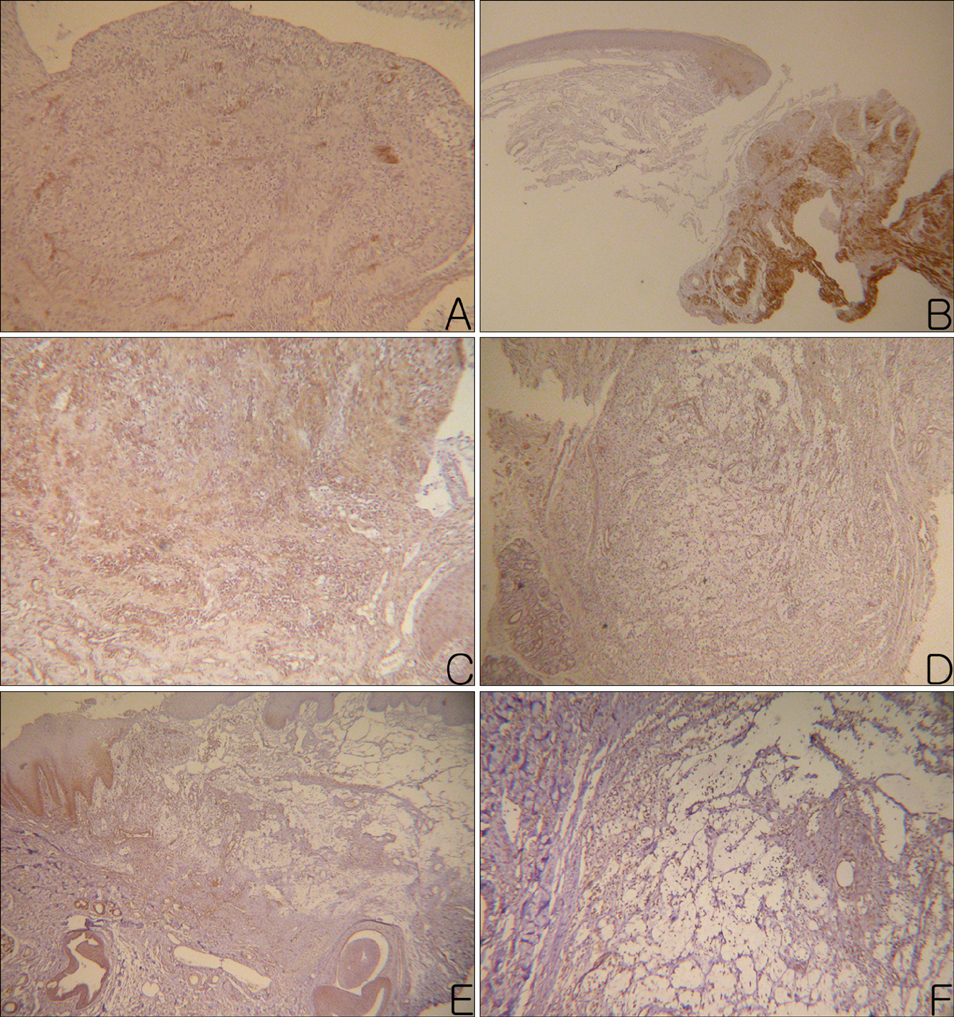
Seventeen oral mucoceles were examined clinically and immunohistologically. The mucoceles were divided into two groups by their clinical manifestations: papular group (PG) and nodular group (NG).
RESULTS
Histologically, granulation tissue formed more frequently in the NG group, while CD4 and CD8 positive cells were more abundant in the PG group. There were no significant differences in the tumor necrosis factor-alpha or the matrix metalloproteinases (MMP)-2 and 9, between the two groups.
CONCLUSION
There were significant differences in the depth of the lesions, granulation tissue formation and infiltrating T lymphocytes between the PG and NP type of mucoceles. These findings suggest that the clinical manifestations may be influenced by the type of inflammatory response and extracellular matrix remodeling.
Keyword
MeSH Terms
Figure
Reference
-
1. Ship JA, Phelan J, Kerr AR. Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Biology and pathology of the oral mucosa. Fitzpatrick's dermatology in general medicine. 2003. 6th ed. New York: McGraw-Hill;1087–1088.2. Lattanand A, Johnson WC, Graham JH. Mucous cyst (mucocele). A clinicopathologic and histochemical study. Arch Dermatol. 1970. 101:673–678.
Article3. Stetler-Stevenson WG. Dynamics of matrix turnover during pathologic remodeling of the extracellular matrix. Am J Pathol. 1996. 148:1345–1350.4. Chaudhry AP, Reynolds DH, Lachapelle CF, Vickers RA. A clinical and experimental study of mucocele (retention cyst). J Dent Res. 1960. 39:1253–1262.
Article5. Woo SB. McKee PH, Calonje E, Granter SR, editors. Diseases of the oral mucosa. Pathology of the skin: with clinical correlations. 2005. 3rd ed. Philadelphia: Elsevier Mosby;447.6. Hoque MO, Azuma M, Sato M. Significant correlation between matrix metalloproteinase activity and tumor necrosis factor-alpha in salivary extravasation mucoceles. J Oral Pathol Med. 1998. 27:30–33.
Article7. Eversole LR, Sabes WR. Minor salivary gland duct changes due to obstruction. Arch Otolaryngol. 1971. 94:19–24.
Article8. Dallos A, Kiss M, Polyanka H, Dobozy A, Kemeny L, Husz S. Effects of the neuropeptides substance P, calcitonin gene-related peptide, vasoactive intestinal polypeptide and galanin on the production of nerve growth factor and inflammatory cytokines in cultured human keratinocytes. Neuropeptides. 2006. 40:251–263.
Article9. Clark JD, Shi X, Li X, Qiao Y, Liang D, Angst MS, et al. Morphine reduces local cytokine expression and neutrophil infiltration after incision. Mol Pain. 2007. 3:28.
Article10. Harrison JD, Garrett JR. Experimental salivary mucoceles in cat. A histochemical study. J Oral Pathol. 1975. 4:297–306.
Article11. Perez C, Albert I, DeFay K, Zachariades N, Gooding L, Kriegler M. A nonsecretable cell surface mutant of tumor necrosis factor (TNF) kills by cell-to-cell contact. Cell. 1990. 63:251–258.
Article12. Mauviel A. Cytokine regulation of metalloproteinase gene expression. J Cell Biochem. 1993. 53:288–295.
Article13. Muller K, Meineke V. Radiation-induced alterations in cytokine production by skin cells. Exp Hematol. 2007. 35:96–104.
Article14. Han YP, Tuan TL, Hughes M, Wu H, Garner WL. Transforming growth factor-beta- and tumor necrosis factor-alpha-mediated induction and proteolytic activation of MMP-9 in human skin. J Biol Chem. 2001. 276:22341–22350.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Characteristics between Primary and Secondary Paranasal Mucoceles
- Postoperative Mucoceles of Frontal, Ethmoid, or Sphenoid Sinus
- A Case of Primary Septated Mucocele of Maxillary Sinus
- Clinical Characteristics of Paranasal Sinus Mucoceles Which Invade the Orbit
- Endoscopic Surgery for Paranasal Sinus Mucocele