Korean J Crit Care Med.
2015 Nov;30(4):258-264. 10.4266/kjccm.2015.30.4.258.
The Prognostic Factors of Pneumonia with Septic Shock in Patients Presenting to the Emergency Department
- Affiliations
-
- 1Department of Emergency Medicine, Gachon University, Gil Medical Center, Incheon, Korea. empearl@gilhospital.com
- 2Department of Family Medicine, Gachon University, Gil Medical Center, Incheon, Korea.
- 3Department of Neurology, Gachon University, Gil Medical Center, Incheon, Korea.
- KMID: 2156178
- DOI: http://doi.org/10.4266/kjccm.2015.30.4.258
Abstract
- BACKGROUND
Pneumonia is the most common cause of death among patients with infectious disease in Korea. However, studies of pneumonia with septic shock in patients presenting to the emergency department are limited. The aim of this study was to investigate the prognostic factors associated with pneumonia with septic shock in patients presenting to the emergency department.
METHODS
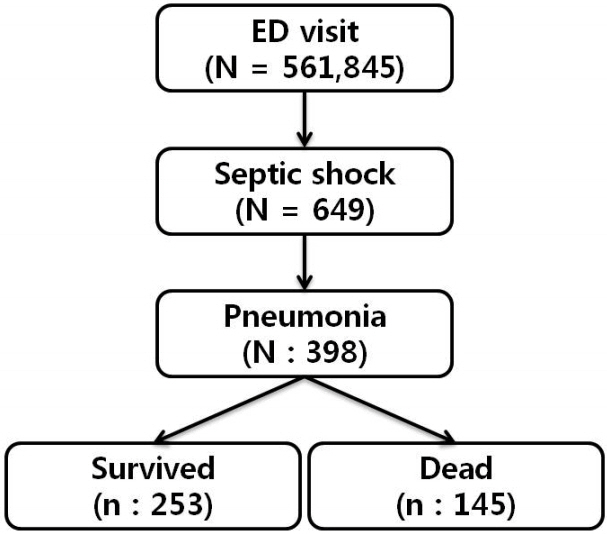
From January 2008 to September 2014, patients with pneumonia with septic shock admitted through the emergency department were retrospectively examined.
RESULTS
Of the 561,845 patients who visited the emergency department, 398 were admitted for pneumonia with septic shock. The 28-day mortality rate in these patients was 36.4%. The independent prognostic factors were old age (>70 yrs) (odds ratio [OR], 2.42; 95%, confidence interval [CI], 1.35-4.32), Acute Physiology and Chronic Health Evaluation (APACHE) II score (OR, 1.04; 95% CI, 1.01-1.08), leukopenia (OR, 3.63; 95% CI, 1.48-8.94), prolonged PT-INR (OR, 2.53; 95% CI, 1.41-4.54), and hypoxemia (OR, 2.88; 95% CI, 1.30-6.38).
CONCLUSIONS
A poor prognosis of patients with pneumonia is associated with old age (>70 yrs), increased APACHE II score, leukopenia, prolonged PT-INR, and hypoxemia.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013; 39:165–228.
Article2. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001; 29:1303–10.
Article3. Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005; 365:63–78.
Article4. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348:1546–54.
Article5. Wang HE, Shapiro N, Angus DC, Yealy DM. National estimates of severe sepsis in United States emergency departments. Crit Care Med. 2007; 35:1928–36.
Article6. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome and associated costs of care. Crit Care Med. 2001; 29:1303–10.
Article7. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004; 32:858–73.
Article8. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008; 34:17–60.
Article9. National Emergency Medical Center. Emergency Medical 2013. 2015 Nov [2015 N0v. 25].Available from: http://www.nemc.or.kr/egen/filedown.do?fileName=2013_nemc.pdf .10. Honselmann KC, Buthut F, Heuwer B, Karadag S, Sayk F, Kurowski V, et al. Long-term mortality and quality of life in intensive care patients treatedfor pneumonia and/or sepsis, predictors of mortality and quality of life in patients with sepsis/pneumonia. J Crit care. 2015; 30:721–6.11. Halm EA, Teirstein AS. Clinical practice. Management of community-acquired pneumonia. N Engl J Med. 2002; 347:2039–45.12. Harrison DA, Welch CA, Eddleston JM. The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit Care. 2006; 10:R42.13. Brun-Buisson C, Meshaka P, Pinton P, Vallet B; EPISEPSIS Study Group. EPISEPSIS : a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Med. 2004; 30:580–8.14. Capp R, Horton CL, Takhar SS, Ginde AA, Peak DA, Zane R, et al. Predictors of patients who present to the emergency department with sepsis and progress to septic shock between 4 and 48 hours of emergency department arrival. Crit Care Med. 2015; 43:983–8.
Article15. Laterre PF, Garber G, Levy H, Wunderink R, Kinasewitz GT, Sollet JP, et al. Severe community-acquired pneumonia as a cause of severe sepsis: data from the PROWESS study. Crit Care Med. 2005; 33:952–61.
Article16. Lee YW, Jung JW, Song JH, Jeon EJ, Choi JC, Shin JW, et al. Risk factors for mortality in community-acquired pneumonia patients admitted to a Referral Hospital. Tuberc Respir Dis. 2006; 61:347–55.
Article17. Park HP, Seo YW, Lee JE, Kim YH, Jang YY, Park SH, et al. Factors associated with early death in patients with community-acquired pneumonia. Tuberc Respir Dis. 2005; 58:607–13.
Article18. Richards G, Levy H, Laterre PF, Feldman C, Woodward B, Bates BM, et al. CURB-65, PSI, and APACHE II to assess mortality risk in patients with severe sepsis and community acquired pneumonia in PROWESS. J Intensive Care Med. 2011; 26:34–40.
Article19. Bohnen JMA, Mustard RA, Oxholm SE, Schouten D. APACHI II Score and Abdominal Sepsis: a prospective study. Arch Surg. 1988; 123:225–29.20. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHI II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.21. Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med. 2006; 34:15–21.
Article22. Kale SS, Yende S. Effects of aging on inflammation and hemostasis through the continuum of critical illness. Aging Dis. 2011; 2:501–11.23. Opal SM, Girard TD, Ely EW. The immunopathogenesis of sepsis in elderly patients. Clin Infect Dis. 2005; 41 Suppl 7:S504–12.
Article24. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/AmericanThoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. CID. 2007; 44(Suppl 2):S27–72.25. ProCESS Investigators, Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014; 370:1683–93.
Article26. Gu WJ, Wang F, Bakker J, Tang L, Liu JC. The effect of goal-directed therapy on mortality in patients with sepsis - earlier is better: a meta-analysis of randomized controlled trials. Crit Care. 2014; 18:570.
Article27. Shin HJ, Lee KH, Hwang SO, Kim H, Shin TY, Kim SC. The efficacy of early goal-directed therapy in septic shock patients in the emergency department: severe sepsis campaign. Korean J Crit Care Med. 2010; 25:61–70.
Article28. Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med. 2015; 43:1907–15.29. Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically Ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014; 311:1308–16.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors in Septic Shock Patients on Arrival at Emergency Department
- Usefulness of Delta Neutrophil Index in Prediction of Septic Shock in Patients with Community-acquired Pneumonia
- Early Prognostic Factors of Patients with Septic Shock
- The Prevalence and Significance of Overt Disseminated Intravascular Coagulation in Patients with Septic Shock in the Emergency Department According to the Third International Consensus Definition
- Incidence and risk factors associated with early death in patients with emergency department septic shock