Korean J Crit Care Med.
2016 Nov;31(4):334-341. 10.4266/kjccm.2016.00339.
The Prevalence and Significance of Overt Disseminated Intravascular Coagulation in Patients with Septic Shock in the Emergency Department According to the Third International Consensus Definition
- Affiliations
-
- 1Department of Emergency Medicine, College of Medicine, Kyung Hee University, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 2Department of Emergency Medicine, College of Medicine, Dankook University, Cheonan, Korea.
- 3Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2371189
- DOI: http://doi.org/10.4266/kjccm.2016.00339
Abstract
- BACKGROUND
The prevalence and prognostic value of overt disseminated intravascular coagulation (DIC) in patients with septic shock presenting to emergency departments (EDs) is poorly understood, particularly following the release of a new definition of septic shock. The purpose of this study was to investigate the prevalence and prognostic value of DIC in septic shock.
METHODS
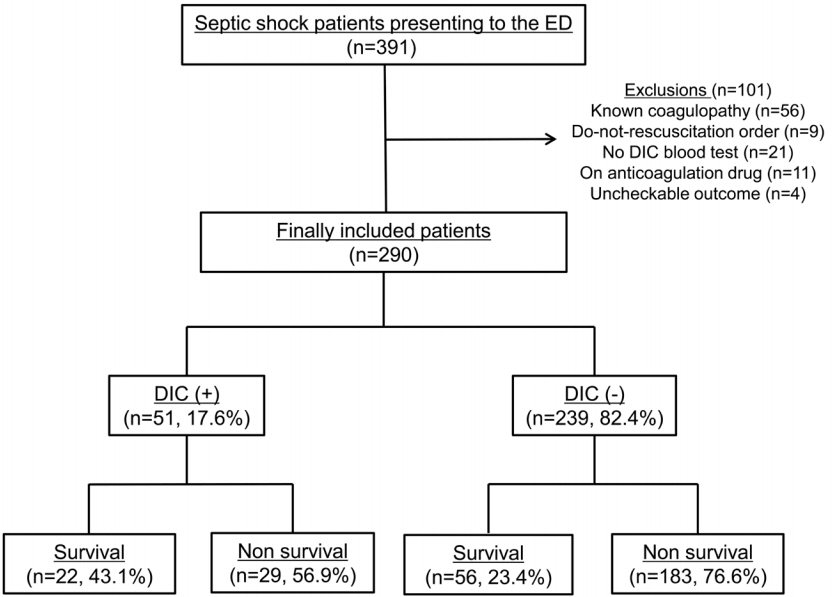
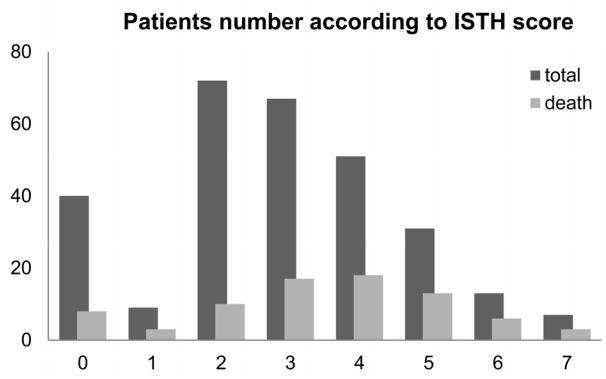
We performed retrospective review of 391 consecutive patients with septic shock admitting to the ED of tertiary care, university-affiliated hospital during a 16-month. Septic shock was defined as fluid-unresponsive hypotension requiring vasopressor to maintain a mean arterial pressure of 65 mmHg or greater, and serum lactate level ≥ 2 mmol/L. Overt DIC was defined as an International Society on Thrombosis and Hemostasis (ISTH) score ≥ 5 points. The primary endpoint was 28-day mortality.
RESULTS
Of 391 patients with septic shock, 290 were included in the present study. The mean age was 65.6 years, the 28-day mortality rate was 26.9%, and the prevalence of overt DIC was 17.6% (n = 51) according to the ISTH score. The median DIC score was higher in non-survivors than in survivors (5.0 vs. 2.0, p = 0.001). Significant higher risk of mortality was observed in overt DIC patients compared to those without (28.2% vs. 13.7%, p = 0.005). Multivariable logistic regression analysis identified DIC to be independently associated with 28-day mortality (odds ratio, 2.689 [95% confidence interval, 1.390-5.201]).
CONCLUSIONS
Using the ISTH criteria of DIC, overt DIC in septic shock was found to be common among patients admitting to the ED and to be associated with higher mortality when it is accompanied with septic shock. Efforts are required to identify presence of overt DIC during the initial treatment of septic shock in patients presenting the the ED.
MeSH Terms
Figure
Cited by 1 articles
-
Relationship between low hemoglobin levels and mortality in patients with septic shock
Sung Min Jung, Youn-Jung Kim, Seung Mok Ryoo, Won Young Kim
Acute Crit Care. 2019;34(2):141-147. doi: 10.4266/acc.2019.00465.
Reference
-
References
1. Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007; 35:1244–50.
Article2. Kim WY, Huh JW, Lim CM, Koh Y, Hong SB. Analysis of progression in risk, injury, failure, loss, and end-stage renal disease classification on outcome in patients with severe sepsis and septic shock. J Crit Care. 2012; 27:104. e1-7.
Article3. Ryoo SM, Kim WY, Huh JW, Hong SB, Lim CM, Koh Y, et al. Prognostic value of B-type natriuretic peptide with the sequential organ failure assessment score in septic shock. Am J Med Sci. 2015; 349:287–91.
Article4. Ryoo SM, Kim WY, Sohn CH, Seo DW, Koh JW, Oh BJ, et al. Prognostic value of timing of antibiotic administration in patients with septic shock treated with early quantitative resuscitation. Am J Med Sci. 2015; 349:328–33.
Article5. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016; 315:801–10.
Article6. Yin Q, Liu B, Chen Y, Zhao Y, Li C. Prognostic value of the International Society on Thrombosis and Haemostasis scoring system for overt disseminated intravascular coagulation in emergency department sepsis. Infection. 2014; 42:629–37.
Article7. Levi M. Disseminated intravascular coagulation. Crit Care Med. 2007; 35:2191–5.
Article8. Dhainaut JF, Shorr AF, Macias WL, Kollef MJ, Levi M, Reinhart K, et al. Dynamic evolution of coagulopathy in the first day of severe sepsis: relationship with mortality and organ failure. Crit Care Med. 2005; 33:341–8.
Article9. Voves C, Wuillemin WA, Zeerleder S. International Society on Thrombosis and Haemostasis score for overt disseminated intravascular coagulation predicts organ dysfunction and fatality in sepsis patients. Blood Coagul Fibrinolysis. 2006; 17:445–51.
Article10. Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016; 315:762–74.11. Gando S, Saitoh D, Ogura H, Fujishima S, Mayumi T, Araki T, et al. A multicenter, prospective validation study of the Japanese Association for Acute Medicine disseminated intravascular coagulation scoring system in patients with severe sepsis. Crit Care. 2013; 17:R111.
Article12. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637.
Article13. Ogawa Y, Yamakawa K, Ogura H, Kiguchi T, Mohri T, Nakamori Y, et al. Recombinant human soluble thrombomodulin improves mortality and respiratory dysfunction in patients with severe sepsis. J Trauma Acute Care Surg. 2012; 72:1150–7.
Article14. Kienast J, Juers M, Wiedermann CJ, Hoffmann JN, Ostermann H, Strauss R, et al. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006; 4:90–7.
Article15. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001; 344:699–709.
Article16. Dhainaut JF, Yan SB, Joyce DE, Pettilä V, Basson B, Brandt JT, et al. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J Thromb Haemost. 2004; 2:1924–33.17. Levi M. Another step in improving the diagnosis of disseminated intravascular coagulation in sepsis. Crit Care. 2013; 17:448.
Article18. Bakhtiari K, Meijers JC, de Jonge E, Levi M. Prospective validation of the International Society of Thrombosis and Haemostasis scoring system for disseminated intravascular coagulation. Crit Care Med. 2004; 32:2416–21.
Article19. Angstwurm MW, Dempfle CE, Spannagl M. New disseminated intravascular coagulation score: a useful tool to predict mortality in comparison with Acute Physiology and Chronic Health Evaluation II and Logistic Organ Dysfunction scores. Crit Care Med. 2006; 34:314–20. quiz 328.
Article20. Takemitsu T, Wada H, Hatada T, Ohmori Y, Ishikura K, Takeda T, et al. Prospective evaluation of three different diagnostic criteria for disseminated intravascular coagulation. Thromb Haemost. 2011; 105:40–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence and prognosis of disseminated intravascular coagulation in patients with severe sepsis or septic shock
- A Fulminant Case of Clostridium perfringens Septic Shock caused by a Liver Abscess with Massive Hemolytic Anemia
- Disseminated Intravascular Coagulation Following Septic Shock in Multiple Open Fractures : a Case Report
- A Case of Septic Shock and Disseminated Intravascular Coagulation Complicated by Acute Myocardial Infarction Following Amniocentesis
- A Case of Pseudomonas Gangrene