Korean J Radiol.
2015 Aug;16(4):767-775. 10.3348/kjr.2015.16.4.767.
Comparison of Ultrasonographic Findings of Biopsy-Proven Tuberculous Lymphadenitis and Kikuchi Disease
- Affiliations
-
- 1Department of Radiology, Guro Hospital, Korea University College of Medicine, Seoul 152-703, Korea. sangil.suh@gmail.com
- 2Department of Radiology, Ansan Hospital, Korea University College of Medicine, Ansan 425-707, Korea.
- KMID: 2155549
- DOI: http://doi.org/10.3348/kjr.2015.16.4.767
Abstract
OBJECTIVE
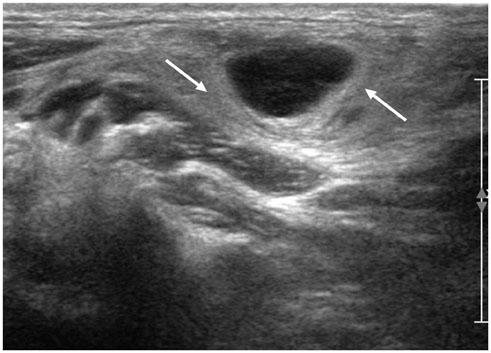
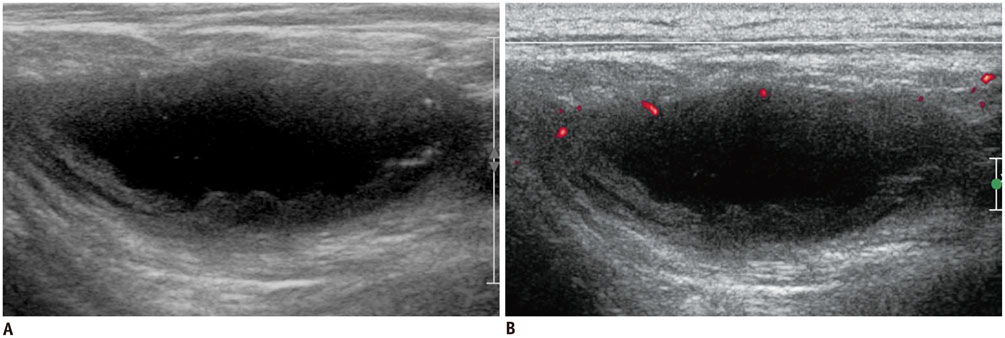
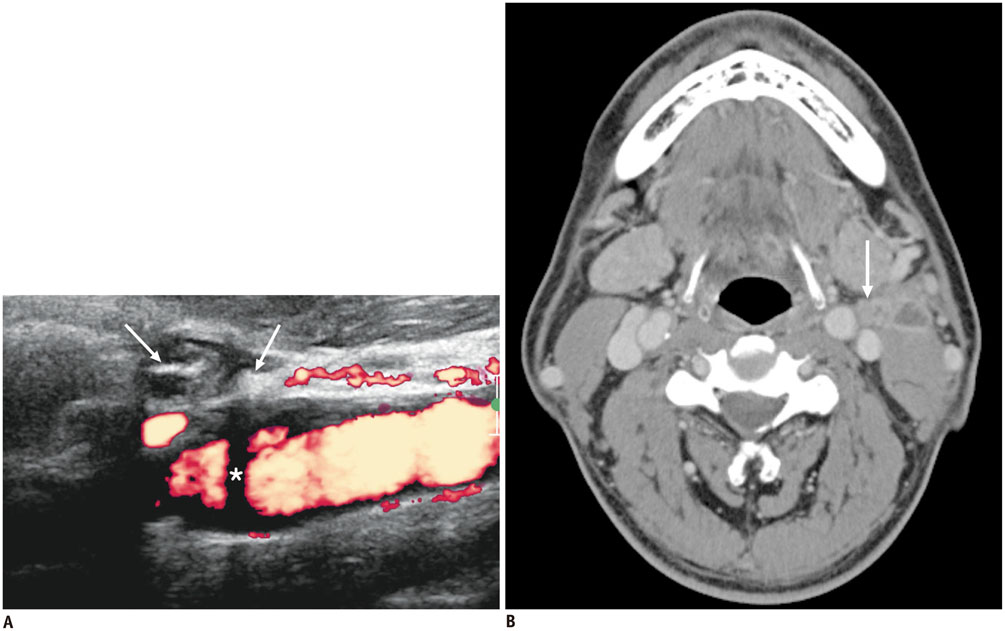
Although tuberculous lymphadenitis and Kikuchi disease are common causes of cervical lymphadenopathy in Asians and exhibit similar clinical manifestations, their treatment strategies are totally different. The purpose of this study was to identify ultrasonographic features that distinguish these two diseases.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board. The study included 77 patients with tuberculous lymphadenitis and 135 patients with Kikuchi disease. The sex and age distributions of the patients were analyzed. The size and shape of lymph nodes (LNs), presence of conglomeration, increased perinodal echogenicity, echogenic hilum, posterior neck involvement, internal calcification, patterns of internal necrosis, laterality of involved LNs, and hilar vascular patterns on ultrasonography were compared between the two groups. Multiple logistic regression analysis was conducted to identify independent findings to discriminate tuberculous lymphadenitis from Kikuchi disease. Finally, diagnostic accuracies were calculated using the independent findings.
RESULTS
The presence of an echogenic hilum, internal calcification, patterns of internal necrosis, and LN hilar vascular structures on power Doppler ultrasonography were independent findings that discriminated tuberculous lymphadenitis from Kikuchi disease. The diagnostic accuracy of each of these four factors was 84.9% (181/212), 76.9% (163/212), 84% (178/212), and 89.2% (189/212), respectively. A combination of internal calcification and hilar vascular structures showed the best accuracy of 89.6% (190/212) (sensitivity, 86.7% [117/135]; specificity, 94.8% [73/77]) for diagnosing Kikuchi disease.
CONCLUSION
The presence of an echogenic hilum, internal calcification, pattern of internal necrosis, and LN hilar vascular structures are useful ultrasonographic findings to differentiate tuberculous lymphadenitis from Kikuchi disease.
MeSH Terms
-
Adolescent
Adult
Aged
Aged, 80 and over
Asian Continental Ancestry Group
Biopsy
Calcinosis/pathology
Child
Child, Preschool
Female
Histiocytic Necrotizing Lymphadenitis/pathology/*ultrasonography
Humans
Lymph Nodes/pathology/*ultrasonography
Male
Middle Aged
Neck/ultrasonography
Necrosis/pathology
Sensitivity and Specificity
Tuberculosis, Lymph Node/pathology/*ultrasonography
Ultrasonography, Doppler
Young Adult
Figure
Reference
-
1. Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY. CT findings in Kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol. 2004; 25:1099–1102.2. Na DG, Chung TS, Byun HS, Kim HD, Ko YH, Yoon JH. Kikuchi disease: CT and MR findings. AJNR Am J Neuroradiol. 1997; 18:1729–1732.3. Onciu M, Medeiros LJ. Kikuchi-Fujimoto lymphadenitis. Adv Anat Pathol. 2003; 10:204–211.4. Song JY, Lee J, Park DW, Sohn JW, Suh SI, Kim IS, et al. Clinical outcome and predictive factors of recurrence among patients with Kikuchi's disease. Int J Infect Dis. 2009; 13:322–326.5. Youk JH, Kim EK, Ko KH, Kim MJ. Sonographic features of axillary lymphadenopathy caused by Kikuchi disease. J Ultrasound Med. 2008; 27:847–853.6. Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol. 2004; 122:141–152.7. Han HJ, Lim GY, Yeo DM, Chung NG. Kikuchi's disease in children: clinical manifestations and imaging features. J Korean Med Sci. 2009; 24:1105–1109.8. Fontanilla JM, Barnes A, von Reyn CF. Current diagnosis and management of peripheral tuberculous lymphadenitis. Clin Infect Dis. 2011; 53:555–562.9. Artenstein AW, Kim JH, Williams WJ, Chung RC. Isolated peripheral tuberculous lymphadenitis in adults: current clinical and diagnostic issues. Clin Infect Dis. 1995; 20:876–882.10. Khan FY. Clinical pattern of tuberculous adenitis in Qatar: experience with 35 patients. Scand J Infect Dis. 2009; 41:128–134.11. Wei YF, Liaw YS, Ku SC, Chang YL, Yang PC. Clinical features and predictors of a complicated treatment course in peripheral tuberculous lymphadenitis. J Formos Med Assoc. 2008; 107:225–231.12. Khanna R, Sharma AD, Khanna S, Kumar M, Shukla RC. Usefulness of ultrasonography for the evaluation of cervical lymphadenopathy. World J Surg Oncol. 2011; 9:29.13. Tong TR, Chan OW, Lee KC. Diagnosing Kikuchi disease on fine needle aspiration biopsy: a retrospective study of 44 cases diagnosed by cytology and 8 by histopathology. Acta Cytol. 2001; 45:953–957.14. Lin HC, Su CY, Huang CC, Hwang CF, Chien CY. Kikuchi's disease: a review and analysis of 61 cases. Otolaryngol Head Neck Surg. 2003; 128:650–653.15. Poulose V, Chiam P, Poh WT. Kikuchi's disease: a Singapore case series. Singapore Med J. 2005; 46:229–232.16. Lee S, Yoo JH, Lee SW. Kikuchi disease: differentiation from tuberculous lymphadenitis based on patterns of nodal necrosis on CT. AJNR Am J Neuroradiol. 2012; 33:135–140.17. Lo WC, Chang WC, Lin YC, Hsu YP, Liao LJ. Ultrasonographic differentiation between Kikuchi's disease and lymphoma in patients with cervical lymphadenopathy. Eur J Radiol. 2012; 81:1817–1820.18. Ying M, Ahuja AT, Yuen HY. Grey-scale and power Doppler sonography of unusual cervical lymphadenopathy. Ultrasound Med Biol. 2004; 30:449–454.19. Yoo JL, Suh SI, Lee YH, Seo HS, Kim KM, Shin BK, et al. Gray scale and power Doppler study of biopsy-proven Kikuchi disease. J Ultrasound Med. 2011; 30:957–963.20. Ahuja A, Ying M, King A, Yuen HY. Lymph node hilus: gray scale and power Doppler sonography of cervical nodes. J Ultrasound Med. 2001; 20:987–992. quiz 99421. Ahuja AT, Ying M. Sonographic evaluation of cervical lymph nodes. AJR Am J Roentgenol. 2005; 184:1691–1699.22. Harnsberger HR, Glastonbury CM, Michel MA, Koch BL, Branstetter BF, Davidson HC, et al. Diagnostic Imaging: Head and Neck. 2nd ed. Frisens, Altona, Manitoba, Canada: Amirsys;2011.23. Asai S, Miyachi H, Suzuki K, Shimamura K, Ando Y. Ultrasonographic differentiation between tuberculous lymphadenitis and malignant lymph nodes. J Ultrasound Med. 2001; 20:533–538.24. Ying M, Ahuja A, Brook F. Accuracy of sonographic vascular features in differentiating different causes of cervical lymphadenopathy. Ultrasound Med Biol. 2004; 30:441–447.25. Miller WT Jr, Perez-Jaffe LA. Cross-sectional imaging of Kikuchi disease. J Comput Assist Tomogr. 1999; 23:548–551.26. Pombo F, Rodríguez E, Mato J, Pérez-Fontán J, Rivera E, Valvuena L. Patterns of contrast enhancement of tuberculous lymph nodes demonstrated by computed tomography. Clin Radiol. 1992; 46:13–17.27. Fulcher AS. Cervical lymphadenopathy due to Kikuchi disease: US and CT appearance. J Comput Assist Tomogr. 1993; 17:131–133.28. Ogawa M, Ueda S, Ohto M, Fujita M, Kubosawa T. Ultrasonography of cervical lymphadenopathy in a patient with Kikuchi's disease. Acta Radiol. 1991; 32:260–261.29. De Backer AI, Mortelé KJ, Van Den Heuvel E, Vanschoubroeck IJ, Kockx MM, Van de Vyvere M. Tuberculous adenitis: comparison of CT and MRI findings with histopathological features. Eur Radiol. 2007; 17:1111–1117.30. Lee Y, Park KS, Chung SY. Cervical tuberculous lymphadenitis: CT findings. J Comput Assist Tomogr. 1994; 18:370–375.31. Moon WK, Han MH, Chang KH, Im JG, Kim HJ, Sung KJ, et al. CT and MR imaging of head and neck tuberculosis. Radiographics. 1997; 17:391–402.32. Kuo TT, Lo SK. Significance of histological subtypes of Kikuchi's disease: comparative immunohistochemical and apoptotic studies. Pathol Int. 2004; 54:237–240.33. Hutchinson CB, Wang E. Kikuchi-Fujimoto disease. Arch Pathol Lab Med. 2010; 134:289–293.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Histiocytic Necrotizing Lymphadenitis(Kikuchi's Disease) A clinicopathologic study of 1 cases
- Kikuchi-Fujimoto Disease Coexistent with Papillary Thyroid Carcinoma in a Single Lymph Node
- Clinical and Radiologic Characteristics of Kikuchi's Disease
- A Case of Subacute Necrotizing Lymphadenitis Associated with Yersinia Infection in a 12 Years Old Child
- A Case of Kikuchi's Disease (Histiocytic Necrotizing Lymphadenopathy) Showing Typical Histopathologic Findings in Cutaneous Lesion