Yonsei Med J.
2015 Mar;56(2):582-585. 10.3349/ymj.2015.56.2.582.
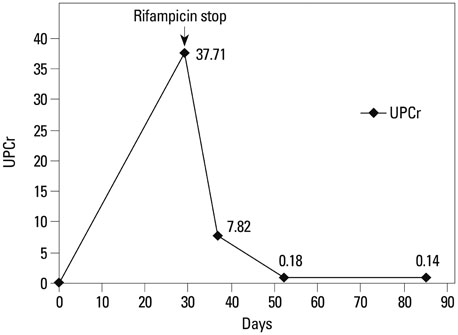
Rifampicin-Induced Minimal Change Disease Is Improved after Cessation of Rifampicin without Steroid Therapy
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. ohjmd@yuhs.ac
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2070042
- DOI: http://doi.org/10.3349/ymj.2015.56.2.582
Abstract
- There are several reports to demonstrate that rifampicin, a major anti-tuberculosis agent, is associated with some adverse renal effects, with a few cases of rifampicin-induced minimal change disease (MCD). In the present case, a 68-year-old female presented with nausea, vomiting, foamy urine, general weakness and edema. She had been taking rifampicin for 4 weeks due to pleural tuberculosis. The patient had no proteinuria before the anti-tuberculosis agents were started, but urine tests upon admission showed heavy proteinuria with a 24-h urinary protein of 9.2 g/day, and serum creatinine, albumin, and total cholesterol levels were 1.36 mg/dL, 2.40 g/dL, and 283 mg/dL, respectively. MCD was diagnosed, and the patient achieved complete remission after cessation of rifampicin without undergoing steroid therapy.
Keyword
MeSH Terms
-
Aged
Antibiotics, Antitubercular/*adverse effects/therapeutic use
Edema/etiology
Female
Humans
Kidney Function Tests
Kidney Glomerulus/pathology
Nausea/etiology
Nephrosis, Lipoid/*chemically induced/pathology
Proteinuria
Remission Induction
Rifampin/*adverse effects/therapeutic use
Treatment Outcome
Tuberculosis, Pleural/*drug therapy
Antibiotics, Antitubercular
Rifampin
Figure
Reference
-
1. Covic A, Goldsmith DJ, Segall L, Stoicescu C, Lungu S, Volovat C, et al. Rifampicin-induced acute renal failure: a series of 60 patients. Nephrol Dial Transplant. 1998; 13:924–929.
Article2. De Vriese AS, Robbrecht DL, Vanholder RC, Vogelaers DP, Lameire NH. Rifampicin-associated acute renal failure: pathophysiologic, immunologic, and clinical features. Am J Kidney Dis. 1998; 31:108–115.
Article3. Gabow PA, Lacher JW, Neff TA. Tubulointerstitial and glomerular nephritis associated with rifampin. Report of a case. JAMA. 1976; 235:2517–2518.
Article4. Kohno K, Mizuta Y, Yoshida T, Watanabe H, Nishida H, Fukami K, et al. Minimal change nephrotic syndrome associated with rifampicin treatment. Nephrol Dial Transplant. 2000; 15:1056–1059.
Article5. Murray AN, Cassidy MJ, Templecamp C. Rapidly progressive glomerulonephritis associated with rifampicin therapy for pulmonary tuberculosis. Nephron. 1987; 46:373–376.
Article6. Muthukumar T, Jayakumar M, Fernando EM, Muthusethupathi MA. Acute renal failure due to rifampicin: a study of 25 patients. Am J Kidney Dis. 2002; 40:690–696.
Article7. Neugarten J, Gallo GR, Baldwin DS. Rifampin-induced nephrotic syndrome and acute interstitial nephritis. Am J Nephrol. 1983; 3:38–42.
Article8. Rekha VV, Santha T, Jawahar MS. Rifampicin-induced renal toxicity during retreatment of patients with pulmonary tuberculosis. J Assoc Physicians India. 2005; 53:811–813.9. Tada T, Ohara A, Nagai Y, Otani M, Ger YC, Kawamura S. A case report of nephrotic syndrome associated with rifampicin therapy. Nihon Jinzo Gakkai Shi. 1995; 37:145–150.10. Yoshioka K, Satake N, Kasamatsu Y, Nakamura Y, Shikata N. Rapidly progressive glomerulonephritis due to rifampicin therapy. Nephron. 2002; 90:116–118.
Article11. Black DA, Rose G, Brewer DB. Controlled trial of prednisone in adult patients with the nephrotic syndrome. Br Med J. 1970; 3:421–426.
Article12. Waldman M, Crew RJ, Valeri A, Busch J, Stokes B, Markowitz G, et al. Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol. 2007; 2:445–453.
Article13. Glassock RJ. Secondary minimal change disease. Nephrol Dial Transplant. 2003; 18:Suppl 6. vi52–vi58.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rifampicin-Induced Severe Hyperkalemia Requiring Hemodialysis in a Patient with Addison's Disease
- A Case of Rifampicin-induced Thrombocytopenic Purpura
- Tracing the Variation in Physiological Response to Rifampicin Across the Microbial Spectrum
- Rifampicin Inhibits the LPS-induced Expression of Toll-like Receptor 2 via the Suppression of NF-kappaB DNA-binding Activity in RAW 264.7 Cells
- Rifampicin-induced Tubulo-interstitial Nephritis - A case report -