Tuberc Respir Dis.
2006 Nov;61(5):473-478. 10.4046/trd.2006.61.5.473.
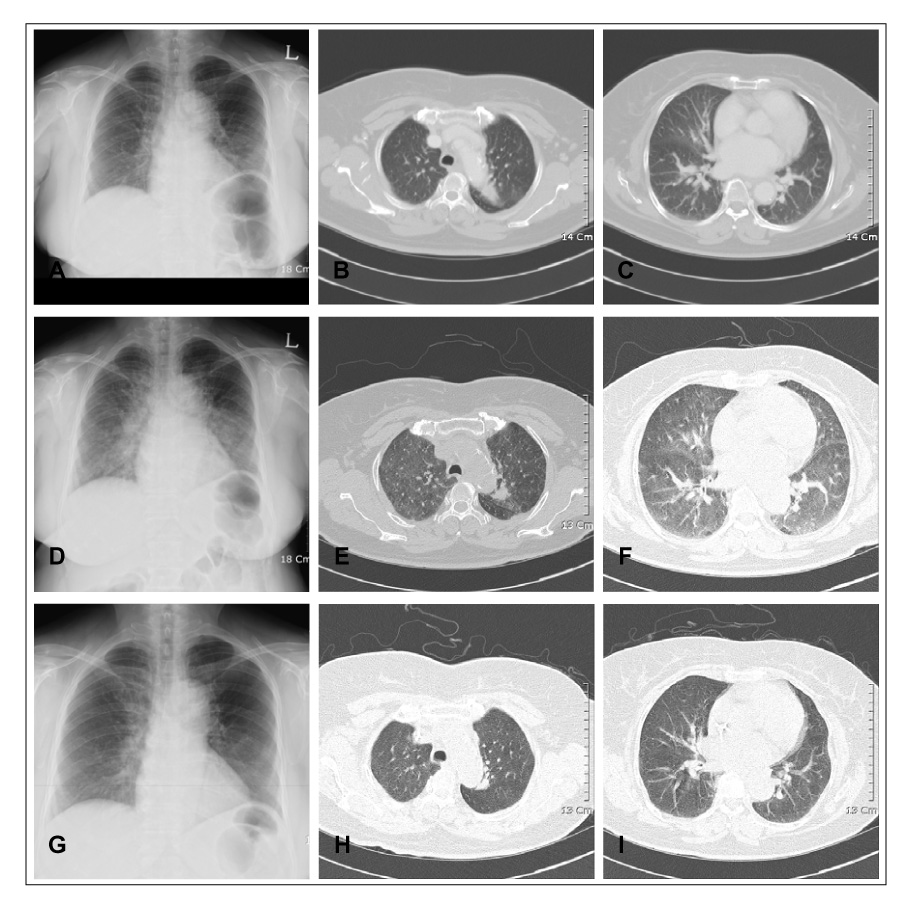
Two Cases of Transfusion Related Acute Lung Injury
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Korea University, Seoul, Korea. dreamnet@dreamwiz.com
- KMID: 1970253
- DOI: http://doi.org/10.4046/trd.2006.61.5.473
Abstract
- Transfusion related acute lung injury (TRALI) is a serious, potentially life-threatening complication of transfusion therapy that is sometimes under diagnosed and under reported. Patients with TRALI present with dyspnea/respiratory distress and fever. The symptoms, signs and chest radiological findings in TRALI are similar to transfusion associated circulatory overload, which makes it is difficult to distinguish it from circulatory overload. Although the mortality rate in cases of TRALI is relatively low, TRALI is the third most common cause of fatal transfusion reactions next to ABO blood type incompatibility and hepatitis. Mild-to-moderate cases of TRALI may be misdiagnosed as volume overload. Recently, we encountered two cases where the patients suffered from dyspnea and fever after a transfusion. and review of the relevant literature.
MeSH Terms
Figure
Cited by 1 articles
-
A case of transfusion-related acute lung injury induced by anti-human leukocyte antigen antibodies in acute leukemia
Sun Mi Jin, Moon Ju Jang, Ji Young Huh, Myoung Hee Park, Eun Young Song, Doyeun Oh
Korean J Hematol. 2012;47(4):302-306. doi: 10.5045/kjh.2012.47.4.302.
Reference
-
1. Barnard RD. Indiscriminate transfusion: a critique of case reports illustrating hypersensitivity reactions. N Y State J Med. 1951. 51:2399–2402.2. Popovsky MA, Abel MD, Moore SB. Transfusion-related acute lung injury associated with passive transfer of antileukocyte antibodies. Am Rev Respir Dis. 1983. 128:185–189.3. Bux J. Transfusion-related acute lung injury (TRALI): a serious adverse event of blood transfusion. Vox Sang. 2005. 89:1–10.4. Kleinman S, Caulfield T, Chan P, Davenport R, McFarland J, McPhedran S, et al. Toward an understanding of transfusion-related acute lung injury: statement of a consensus panel. Transfusion. 2004. 44:1774–1789.5. Toy P, Popovsky MA, Abraham E, Ambruso DR, Holness LG, Kopko PM, et al. Transfusion-related acute lung injury: definition and review. Crit Care Med. 2005. 33:721–726.6. Sazama K. Reports of 355 transfusion-associated deaths: 1976 through 1985. Transfusion. 1990. 30:583–590.7. Suassuna JH, da Costa MA, Faria RA, Melichar AC. Noncardiogenic pulmonary edematriggered by intravenous immunoglobulin in cancer-associated thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Nephron. 1997. 77:368–370.8. Wolf CF, Canale VC. Fatal pulmonary hypersensitivity reaction to HL-A incompatible blood transfusion: report of a case and review of the literature. Transfusion. 1976. 16:135–140.9. Silliman CC, Dickey WO, Paterson AJ, Thurman GW, Clay KL, Johnson CA, et al. Analysis of the priming activity of lipids generated during routine storage of platelet concentrates. Transfusion. 1996. 36:133–139.10. Gong MN, Wei Z, Xu LL, Miller DP, Thompson BT, Christiani DC. Polymorphism in the surfactant protein-B gene, gender, and the risk of direct pulmonary injury and ARDS. Chest. 2004. 125:203–211.11. Hudson LD, Milberg JA, Anardi D, Maunder RJ. Clinical risks for development of the acute respiratory distress syndrome. Am J Respir Crit Care Med. 1995. 151:293–301.12. Pepe PE, Potkin RT, Reus DH, Hudson LD, Carrico CJ. Clinical predictors of the adult respiratory distress syndrome. Am J Surg. 1982. 144:124–130.13. Fein A, Grossman RF, Jones JG, Overland E, Pitts L, Murray JF, et al. The value of edema fluid protein measurement in patients with pulmonary edema. Am J Med. 1979. 67:32–38.14. Ausley MB Jr. Fatal transfusion reactions caused by donor antibodies to recipient leukocytes. Am J Forensic Med Pathol. 1987. 8:287–290.15. Brittingham TE. Immunologic studies on leukocytes. Vox Sang. 1957. 2:242–248.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transfusion-related Acute Lung Injury
- A Case of Acute Lung Injury after Transfusion during Cesarean Section: A Case Report
- A Case of Transfusion-related Acute Lung Injury
- Transfusion-related acute lung injury; clinical perspectives
- Transfusion-Related Acute Lung Injury after Stored Packed Red Blood Cell Transfusion: A Case Report