Tuberc Respir Dis.
2014 Dec;77(6):243-250. 10.4046/trd.2014.77.6.243.
Prognostic Value of Serum Growth Differentiation Factor-15 in Patients with Chronic Obstructive Pulmonary Disease Exacerbation
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. sicha@knu.ac.kr
- 2Department of Radiology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 1842991
- DOI: http://doi.org/10.4046/trd.2014.77.6.243
Abstract
- BACKGROUND
Information regarding prognostic value of growth differentiation factor 15 (GDF-15) and heart-type fatty acid-binding protein (H-FABP) in patients with chronic obstructive pulmonary disease (COPD) exacerbation is limited. The aim of this study was to investigate whether serum levels of GDF-15 and H-FABP predict an adverse outcome for COPD exacerbation.
METHODS
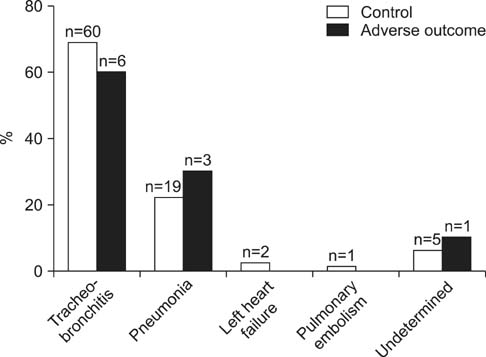
Clinical variables, including serum GDF-15 and H-FABP levels were compared in prospectively enrolled patients with COPD exacerbation that did or did not experience an adverse outcome. An adverse outcome included 30-day mortality and need for endotracheal intubation or inotropic support.
RESULTS
Ninety-seven patients were included and allocated into an adverse outcome (n=10) or a control (n=87) group. Frequencies of mental change and PaCO2>37 mm Hg were significantly higher in the adverse outcome group (mental change: 30% vs. 6%, p=0.034 and PaCO2>37 mm Hg: 80% vs. 22%, p<0.001, respectively). Serum GDF-15 elevation (>1,600 pg/mL) was more common in the adverse outcome group (80% vs. 43%, p=0.041). However, serum H-FABP level and frequency of serum H-FABP elevation (>755 pg/mL) did not differ between the two groups. Multivariate analysis showed that an elevated serum GDF-15 and PaCO2>37 mm Hg were significant predictors of an adverse outcome (odds ratio [OR], 25.8; 95% confidence interval [CI], 2.7-243.8; p=0.005 and OR, 11.8; 95% CI, 1.2-115.3; p=0.034, respectively).
CONCLUSION
Elevated serum GDF-15 level and PaCO2>37 mm Hg were found to predict an adverse outcome independently in patients with COPD exacerbation, suggesting the possibility that serum GDF-15 could be used as a prognostic biomarker of COPD exacerbation.
Keyword
MeSH Terms
Figure
Reference
-
1. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997; 349:1498–1504.2. Anzueto A. Impact of exacerbations on COPD. Eur Respir Rev. 2010; 19:113–118.3. Connors AF Jr, Dawson NV, Thomas C, Harrell FE Jr, Desbiens N, Fulkerson WJ, et al. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Outcomes following acute exacerbation of severe chronic obstructive lung disease. Am J Respir Crit Care Med. 1996; 154(4 Pt 1):959–967.4. Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003; 124:459–467.5. Singanayagam A, Schembri S, Chalmers JD. Predictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013; 10:81–89.6. Stolz D, Breidthardt T, Christ-Crain M, Bingisser R, Miedinger D, Leuppi J, et al. Use of B-type natriuretic peptide in the risk stratification of acute exacerbations of COPD. Chest. 2008; 133:1088–1094.7. Chang CL, Robinson SC, Mills GD, Sullivan GD, Karalus NC, McLachlan JD, et al. Biochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPD. Thorax. 2011; 66:764–768.8. Baillard C, Boussarsar M, Fosse JP, Girou E, Le Toumelin P, Cracco C, et al. Cardiac troponin I in patients with severe exacerbation of chronic obstructive pulmonary disease. Intensive Care Med. 2003; 29:584–589.9. Rammaert B, Verdier N, Cavestri B, Nseir S. Procalcitonin as a prognostic factor in severe acute exacerbation of chronic obstructive pulmonary disease. Respirology. 2009; 14:969–974.10. Meadows CA, Risbano MG, Zhang L, Geraci MW, Tuder RM, Collier DH, et al. Increased expression of growth differentiation factor-15 in systemic sclerosis-associated pulmonary arterial hypertension. Chest. 2011; 139:994–1002.11. Su AI, Wiltshire T, Batalov S, Lapp H, Ching KA, Block D, et al. A gene atlas of the mouse and human protein-encoding transcriptomes. Proc Natl Acad Sci U S A. 2004; 101:6062–6067.12. Wollert KC, Kempf T, Peter T, Olofsson S, James S, Johnston N, et al. Prognostic value of growth-differentiation factor-15 in patients with non-ST-elevation acute coronary syndrome. Circulation. 2007; 115:962–971.13. Kempf T, Bjorklund E, Olofsson S, Lindahl B, Allhoff T, Peter T, et al. Growth-differentiation factor-15 improves risk stratification in ST-segment elevation myocardial infarction. Eur Heart J. 2007; 28:2858–2865.14. Kempf T, von Haehling S, Peter T, Allhoff T, Cicoira M, Doehner W, et al. Prognostic utility of growth differentiation factor-15 in patients with chronic heart failure. J Am Coll Cardiol. 2007; 50:1054–1060.15. Lankeit M, Kempf T, Dellas C, Cuny M, Tapken H, Peter T, et al. Growth differentiation factor-15 for prognostic assessment of patients with acute pulmonary embolism. Am J Respir Crit Care Med. 2008; 177:1018–1025.16. Nickel N, Kempf T, Tapken H, Tongers J, Laenger F, Lehmann U, et al. Growth differentiation factor-15 in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med. 2008; 178:534–541.17. Alhadi HA, Fox KA. Do we need additional markers of myocyte necrosis: the potential value of heart fatty-acid-binding protein. QJM. 2004; 97:187–198.18. Storch J, Thumser AE. The fatty acid transport function of fatty acid-binding proteins. Biochim Biophys Acta. 2000; 1486:28–44.19. O'Donoghue M, de Lemos JA, Morrow DA, Murphy SA, Buros JL, Cannon CP, et al. Prognostic utility of heart-type fatty acid binding protein in patients with acute coronary syndromes. Circulation. 2006; 114:550–557.20. Dellas C, Puls M, Lankeit M, Schafer K, Cuny M, Berner M, et al. Elevated heart-type fatty acid-binding protein levels on admission predict an adverse outcome in normotensive patients with acute pulmonary embolism. J Am Coll Cardiol. 2010; 55:2150–2157.21. Puls M, Dellas C, Lankeit M, Olschewski M, Binder L, Geibel A, et al. Heart-type fatty acid-binding protein permits early risk stratification of pulmonary embolism. Eur Heart J. 2007; 28:224–229.22. Boscheri A, Wunderlich C, Langer M, Schoen S, Wiedemann B, Stolte D, et al. Correlation of heart-type fatty acid-binding protein with mortality and echocardiographic data in patients with pulmonary embolism at intermediate risk. Am Heart J. 2010; 160:294–300.23. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176:532–555.24. Tillie-Leblond I, Marquette CH, Perez T, Scherpereel A, Zanetti C, Tonnel AB, et al. Pulmonary embolism in patients with unexplained exacerbation of chronic obstructive pulmonary disease: prevalence and risk factors. Ann Intern Med. 2006; 144:390–396.25. Choi KJ, Cha SI, Shin KM, Lee J, Hwangbo Y, Yoo SS, et al. Prevalence and predictors of pulmonary embolism in Korean patients with exacerbation of chronic obstructive pulmonary disease. Respiration. 2013; 85:203–209.26. Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988; 93:580–586.27. Shorr AF, Sun X, Johannes RS, Yaitanes A, Tabak YP. Validation of a novel risk score for severity of illness in acute exacerbations of COPD. Chest. 2011; 140:1177–1183.28. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.29. McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001; 104:2797–2802.30. Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989; 2:358–367.31. Wells JM, Washko GR, Han MK, Abbas N, Nath H, Mamary AJ, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012; 367:913–921.32. Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM. Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology. 2010; 254:609–616.33. Edwards PD, Bull RK, Coulden R. CT measurement of main pulmonary artery diameter. Br J Radiol. 1998; 71:1018–1020.34. Shimano M, Ouchi N, Walsh K. Cardiokines: recent progress in elucidating the cardiac secretome. Circulation. 2012; 126:e327–e332.35. Matkovic Z, Huerta A, Soler N, Domingo R, Gabarrus A, Torres A, et al. Predictors of adverse outcome in patients hospitalised for exacerbation of chronic obstructive pulmonary disease. Respiration. 2012; 84:17–26.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Study of Clarithromycin for the Treatment of Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Apoptosis of T Lymphocytes Isolated from Peripheral Blood of Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Chronic Obstructive Pulmonary Disease: Respiratory Review of 2014
- Pulmonary Strongyloidiasis Masquerading as Exacerbation of Chronic Obstructive Pulmonary Disease
- The Relationship between Airway Inflammation and Exacerbation in Chronic Obstructive Pulmonary Disease