Yonsei Med J.
2006 Dec;47(6):826-832. 10.3349/ymj.2006.47.6.826.
Management Strategy for Congenital Choledochal Cyst with Co-existing Intrahepatic Dilation and Aberrant Bile Duct As Well As Other Complicated Biliary Anomalies
- Affiliations
-
- 1Department of Pediatric Surgery, The Affiliated Hospital of Medical College, Qing Dao University, Qing Dao 266003, China. dong.qian@qdumh.qd.sd.cn
- KMID: 1777172
- DOI: http://doi.org/10.3349/ymj.2006.47.6.826
Abstract
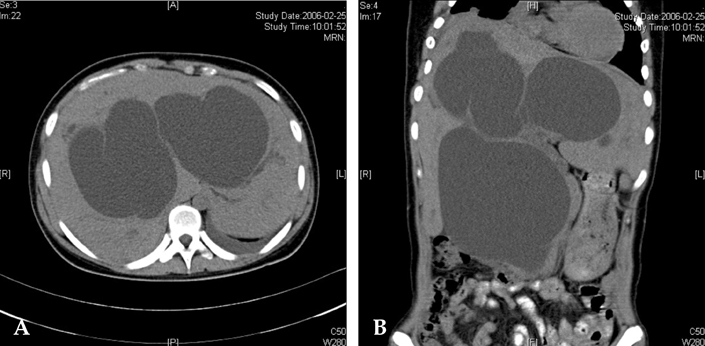
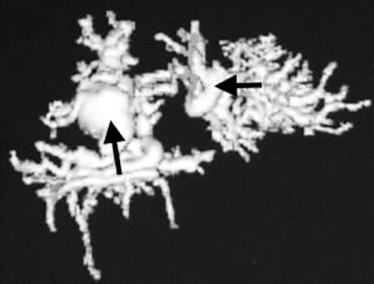
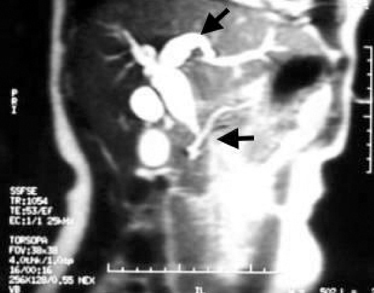
- The purpose of this study was to investigate and discuss imaging methods and management strategies for congenital choledochal cyst with co-existing intrahepatic dilation and aberrant bile duct as well as other complicated biliary anomalies. In this study we reviewed and analyzed 72 patients with congenital choledochal cyst, ranging in age from 15 days to 12 years old and who were seen at our hospital during the past 12 years, from January 1993 to October 2005. The image manifestation and clinical significance of patients with co- xisting intrahepatic biliary dilation and aberrant bile duct were carefully examined during operation via MRCP, cholangiography and choledochoscope. Twenty-two cases (30.1%) presented with intrahepatic bile duct dilation and 12 of these were of the cystic type. That is, the orifice of the dilated intrahepatic tract that converged into the common hepatic duct showed membrane or septum-like stenosis. In 10 cases the dilation tapered off from the porta hepatis to the initiating terminals of the intra-hepatic bile ducts and was not accompanied by stenosis. An aberrant bile duct was observed in 2 of the cases. In 3 cases, the right and left hepatic ducts converged at the choledochal cyst. In conclusion, the imaging methods for intrahepatic bile duct dilation possess important clinical significance. Further, for hepatojejunostomy with radical excision of a choledochal cyst, additional operative procedures for intrahepatic stenosis, possible bile duct malformation and pancreaticobiliary common duct calculi can potentially reduce postoperative complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Jordan PH Jr, Goss JA Jr, Rosenberg WR, Woods KL. Some considerations for management of choledochal cysts. Am J Surg. 2004. 187:790–795.2. Tsuchida A, Kasuya K, Endo M, Saito H, Inoue K, Nagae I, et al. High risk of bile duct carcinogenesis after primary resection of a congenital biliary dilatation. Oncol Rep. 2003. 10:1183–1187.3. Okada A, Hasegawa T, Oguchi Y, Nakamura T. Recent advances in pathophysiology and surgical treatment of congenital dilatation of the bile duct. J Hepatobiliary Pancreat Surg. 2002. 9:342–351.4. Qian D, Kinouchi T, Komi N, Baixiang J. Studies on the mechanism of biliary carcinogenesis in congenital choledochal cyst. Chin J Pediatr Surg. 1994. 15:97. (In Chinese).5. Qian D, Akimoto R. Qian D, editor. Pancreaticobiliary maljunction. Pediatric Hepatobiliary Surgery. 2005. 1st ed. Beijing: The People's Health Publishing House;409–425.6. Qian D, Yang B. The expression of PCNA and P53 protein in congenital bile duct dilation and its significance. Shandong Med J. 2003. 43:3.7. Qian D, Kinouchi T, Kunitomo K, Kataoka K, Matin MA, Akimoto S, et al. Mutagenicity of the bile of dogs with an experimental model of an anomalous arrangement of the pancreaticobiliary duct. Carcinogenesis. 1993. 14:743–747.8. Shimotakahara A, Yamataka A, Kobayashi H, Okada Y, Yanai T, Lane GT, et al. Forme fruste choledochal cyst: long-term follow-up with special reference to surgical technique. J Pediatr Surg. 2003. 38:1833–1836.9. Ando H, Kaneko K, Ito F, Seo T, Ito T. Operative treatment of congenital stenoses of the intrahepatic bile ducts in patients with choledochal cysts. Am J Surg. 1997. 173:491–494.10. Turner MA, Fulcher AS. The cystic duct: normal anatomy and disease processes. Radiographics. 2001. 21:3–22.11. Suzuki M, Shimizu T, Kudo T, Suzuki R, Ohtsuka Y, Yamashiro Y, et al. Usefulness of nonbreath-hold 1-shot magnetic resonance cholangiopancreatography for the evaluation of choledochal cyst in children. J Pediatr Gastroenterol Nutr. 2006. 42:539–544.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Type IV-A Choledochal Cyst with Intrahepatic Bile Duct Stricture
- A Case Report of an Unusual Type of Choledochal Cyst with Choledocholithiasis: Saccular Dilatation of the Confluent Portion of Both Intrahepatic Ducts
- Multiple stone formation in a remnant choledochal cyst
- A Case of Intrahepatic Cholangiocarcinoma Associated with Type IV Choledochal Cyst
- Type IVB Choledochal Cyst : A case report