Clin Orthop Surg.
2014 Mar;6(1):87-95. 10.4055/cios.2014.6.1.87.
Negative Effect of Rapidly Resorbing Properties of Bioactive Glass-Ceramics as Bone Graft Substitute in a Rabbit Lumbar Fusion Model
- Affiliations
-
- 1Department of Orthopedic Surgery, SMG-SNU Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- 2Institute of Medical and Biological Engineering, Medical Research Center, Seoul National University, Seoul, Korea.
- 3The Research and Development Institute, Daewoong Pharmaceutical Co., Yongin, Korea.
- 4Department of Orthopedic Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. choonki@snu.ac.kr
- KMID: 1737636
- DOI: http://doi.org/10.4055/cios.2014.6.1.87
Abstract
- BACKGROUND
Bioactive glass-ceramics have the ability to directly bind to bones and have been widely used as bone graft substitutes due to their high osteoconductivity and biocompatibility. CaO-SiO2-P2O5-B2O3 glass-ceramics are known to have good osteoconductivity and are used as bone graft extenders.
METHODS
This study aimed to evaluate the effects of the resorbing properties of glass-ceramics in bone fusion after producing and analyzing three types of CaO-SiO2-P2O5-B2O3 glass-ceramics with high osteoconductivity that had enhanced resorption by having an increased B2O3 content. The three types of CaO-SiO2-P2O5-B2O3 glass-ceramics with B2O3 contents of 8.0, 9.0, and 9.5 weight % were designated and grouped as P20B80, P10B90, and P5B95, respectively. Glass-ceramic types were tested for fusion rates and bone formation by employing the lumbar 5-6 intertransverse process fusion model in 51 New Zealand male rabbits. Bioactivity was assessed by soaking in simulated body fluid (SBF).
RESULTS
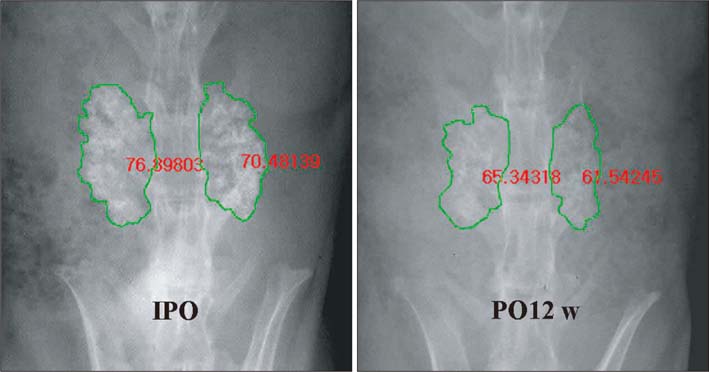
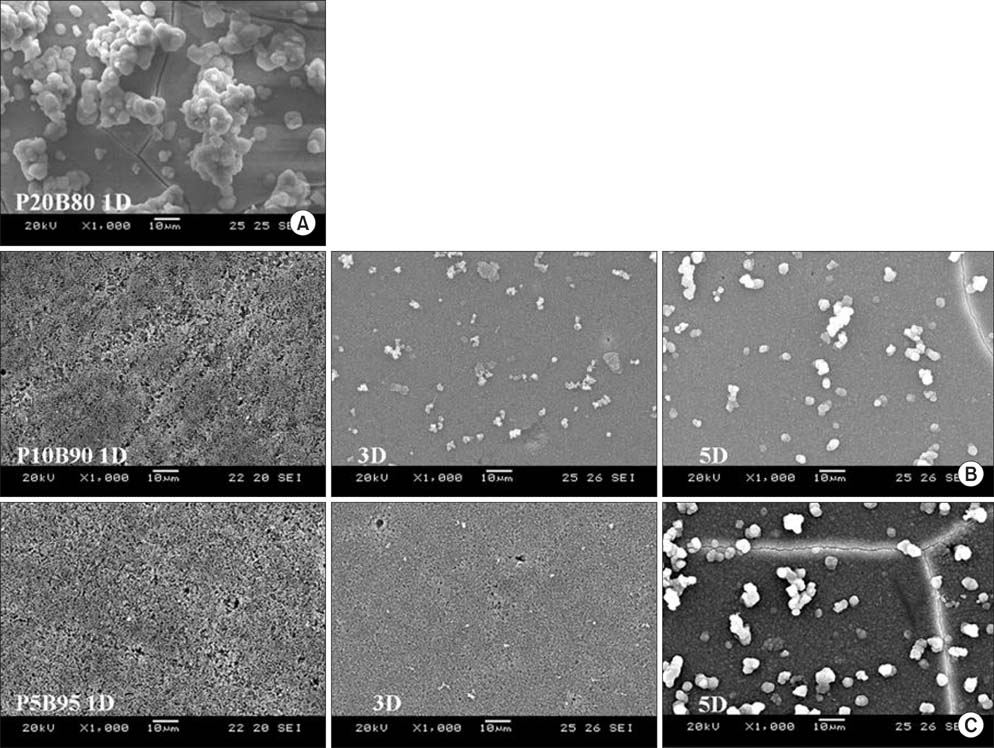
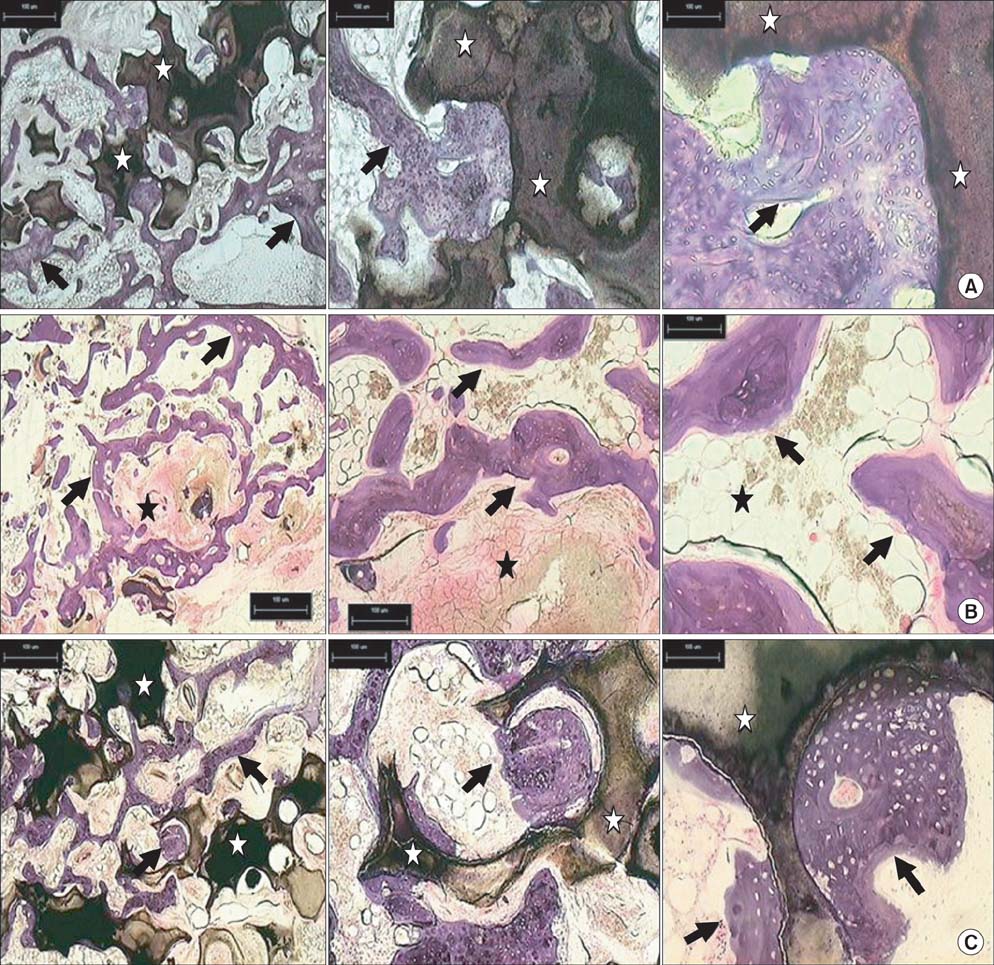
In vitro study results showed sufficient hydroxycarbonate apatite layer formation occurred for P20B80 in1 day, for P10B90 in 3 days, and for P5B95 in 5 days after soaking in SBF. For the rabbit lumbar spine posterolateral fusion model, the autograft group recorded a 100% fusion rate with levels significantly higher than those of P20B80 (29.4%), P10B90 (0%), and P5B95 (14.3%), with high resorbing properties. Resorbing property differences among the three glass-ceramic groups were not significant. Histological results showed new bone formation confirming osteoconductivity in all three types of glass-ceramics. Radiomorphometric results also confirmed the resorbing properties of the three glass-ceramic types.
CONCLUSIONS
The high resorbing properties and osteoconductivity of porous glass-ceramics can be advantageous as no glass-ceramics remain in the body. However, their relatively fast rate of resorption in the body negatively affects their role as an osteoconductive scaffold as glass-ceramics are resorbed before bony fusion.
MeSH Terms
Figure
Reference
-
1. Schnee CL, Freese A, Weil RJ, Marcotte PJ. Analysis of harvest morbidity and radiographic outcome using autograft for anterior cervical fusion. Spine. 1997; 22(19):2222–2227.2. Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003; 28(2):134–139.3. Lee JH, Chang BS, Ryu HS, Lee CK. A 90-day subchronic toxicity study of beta-calcium pyrophosphate in rat. Drug Chem Toxicol. 2009; 32(3):277–282.4. Lee JH, Lee KM, Jang SJ, Lee HS, Baek HR. Effects of bisphosphonate-treated bioactive ceramic grafts for the proliferation and osteoblastic differentiation of human bone marrow mesenchymal stem cells. Tissue Eng Regen Med. 2011; 8(1):69–77.5. Ono K, Yamamuro T, Nakamura T, et al. Apatite-wollastonite containing glass ceramic-fibrin mixture as a bone defect filler. J Biomed Mater Res. 1988; 22(10):869–885.6. Schepers E, de Clercq M, Ducheyne P, Kempeneers R. Bioactive glass particulate material as a filler for bone lesions. J Oral Rehabil. 1991; 18(5):439–452.7. Kitsugi T, Yamamuro T, Nakamura T, et al. Bone bonding behavior of three kinds of apatite containing glass ceramics. J Biomed Mater Res. 1986; 20(9):1295–1307.8. Kokubo T, Ito S, Huang ZT, et al. Ca,P-rich layer formed on high-strength bioactive glass-ceramic A-W. J Biomed Mater Res. 1990; 24(3):331–343.9. Lee JH, Ryu HS, Lee DS, Hong KS, Chang BS, Lee CK. Biomechanical and histomorphometric study on the bone-screw interface of bioactive ceramic-coated titanium screws. Biomaterials. 2005; 26(16):3249–3257.10. Lee JH, Nam H, Ryu HS, Seo JH, Chang BS, Lee CK. Bioactive ceramic coating of cancellous screws improves the osseointegration in the cancellous bone. J Orthop Sci. 2011; 16(3):291–297.11. Lee JH, Park KW, Song KS, et al. Evaluation of osteosynthesis in CaO-SiO2-P2O5-B2O3 glass-ceramics by posterolateral fusion of rabbit lumbar vertebrae. J Korean Soc Spine Surg. 2005; 12(1):1–11.12. Lee JH, Lee CK, Chang BS, et al. In vivo study of novel biodegradable and osteoconductive CaO-SiO2-B2O3 glass-ceramics. J Biomed Mater Res A. 2006; 77(2):362–369.13. Boden SD, Schimandle JH, Hutton WC. An experimental lumbar intertransverse process spinal fusion model: radiographic, histologic, and biomechanical healing characteristics. Spine. 1995; 20(4):412–420.14. Lee JH, Hwang CJ, Song BW, Koo KH, Chang BS, Lee CK. A prospective consecutive study of instrumented posterolateral lumbar fusion using synthetic hydroxyapatite (Bongros-HA) as a bone graft extender. J Biomed Mater Res A. 2009; 90(3):804–810.15. Boden SD, Martin GJ Jr, Morone M, Ugbo JL, Titus L, Hutton WC. The use of coralline hydroxyapatite with bone marrow, autogenous bone graft, or osteoinductive bone protein extract for posterolateral lumbar spine fusion. Spine. 1999; 24(4):320–327.16. Kraal T, Mullender M, de Bruine JH, et al. Resorbability of rigid beta-tricalcium phosphate wedges in open-wedge high tibial osteotomy: a retrospective radiological study. Knee. 2008; 15(3):201–205.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In Vivo reaction of the Highly Porous Glass Ceramics in the Rabbit Tibia: Radiological and Histological Analysis
- Evaluation of Osteosynthesis in CaO-SiO2-P2O5-B2O3 Glass-ceramics by Posterolateral Fusion of Rabbit Lumbar vertebrae
- A Retrospective Comparative Study to Evaluate the Clinical Efficacy Using a Bioactive Glass Ceramic Spacer in Posterior Lumbar Interbody Fusion
- Comparison of the Bone Union Rates Using a Local Autobone and Bone Graft Substitute Mixed Graft in Lumbar Posterolateral Fusion
- THE EFFECT OF BIOACTIVE GLASS AND A RESORBABLE MEMBRANE ON BONE REGENERATION OF THE MANDIBULAR BONE DEFECTS IN RABBIT