J Korean Med Sci.
2010 Jan;25(1):9-15. 10.3346/jkms.2010.25.1.9.
Idarubicin Plus Behenoyl Cytarabine and 6-thioguanine Compares Favorably with Idarubicin Plus Cytarabine-based Regimen for Children with Previously Untreated Acute Myeloid Leukemia: 10-Year Retrospective, Multicenter Study in Korea
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, Hallym University, Seoul, Korea.
- 2Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea. chobinkr@catholic.ac.kr
- 3Department of Pediatrics, Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Pediatrics, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 6Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Pediatric Oncology Clinic, Specific Organs Cancer Center, National Cancer Center, Goyang, Korea.
- KMID: 1713825
- DOI: http://doi.org/10.3346/jkms.2010.25.1.9
Abstract
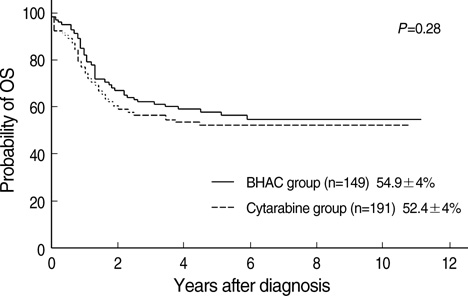
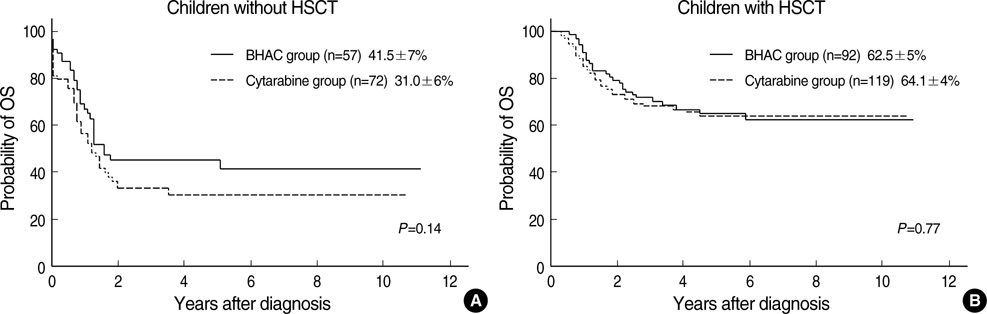
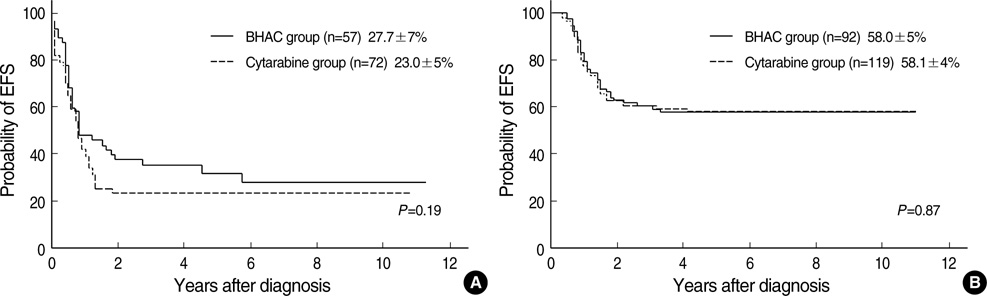
- We investigated the outcome of idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosyl cytosine (BHAC)-based chemotherapy (BHAC group, n=149) compared to idarubicin plus cytarabine-based chemotherapy (cytarabine group, n=191) for childhood acute myeloid leukemia (AML). Between January 1996 and December 2005, 340 children with AML from 5 university hospitals in Korea received the BHAC-based or cytarabine-based chemotherapy, with or without hematopoietic stem cell transplantation. After induction therapy, 264 (77.6%) of 340 children achieved a complete remission (CR) and 43 (12%) achieved a partial remission (PR). The CR rate in the BHAC group was higher than in the cytarabine group (85.2% vs. 71.7%, P=0.004). However, the overall response rate (CR+PR) was not different between the two groups (93.3% vs. 87.9%, P=0.139). The 5-yr estimates of overall survival (OS) of children in the two groups were similar (54.9% for the BHAC group vs. 52.4% for the cytarabine group, P=0.281). Although the results were analyzed according to the treatment type and cytogenetic risk, the OS showed no significant difference between the BHAC group and the cytarabine group. In the present study, the clinical outcomes of the BHAC-based chemotherapy, consisting of BHAC, idarubicin, and 6-TG, are comparable to that of the cytarabine-based chemotherapy for childhood AML.
Keyword
MeSH Terms
-
Adolescent
Antineoplastic Combined Chemotherapy Protocols/*therapeutic use
Child
Child, Preschool
Combined Modality Therapy
Cytarabine/*analogs & derivatives/*therapeutic use
Cytogenetics
Female
Hematopoietic Stem Cell Transplantation
Humans
Idarubicin/*therapeutic use
Infant
Infant, Newborn
Leukemia, Myeloid, Acute/*drug therapy/mortality
Male
Republic of Korea
Retrospective Studies
Survival Analysis
Thioguanine/*therapeutic use
Young Adult
Cytarabine
Thioguanine
Idarubicin
Figure
Cited by 1 articles
-
Improvement of treatment outcome over 2 decades in children with acute myeloid leukemia
Tae Yang Song, Sang Hoon Lee, Gun Kim, Hee Jo Baek, Tai Ju Hwang, Hoon Kook
Blood Res. 2018;53(1):25-34. doi: 10.5045/br.2018.53.1.25.
Reference
-
1. Kaspers GJ, Creutzig U. Pediatric acute myeloid leukemia: international progress and future directions. Leukemia. 2005. 19:2025–2029.2. Smith FO, Alonzo TA, Gerbing RB, Woods WG. Arceci RJ for the Children's Cancer Group. Long-term results of children with acute myeloid leukemia: a report of three consecutive Phase III trials by the Children's Cancer Group: CCG 251, CCG 213 and CCG 2891. Leukemia. 2005. 19:2054–2062.3. Gibson BE, Wheatley K, Hann IM, Stevens RF, Webb D, Hills RK, De Graaf SS, Harrison CJ. Treatment strategy and long-term results in paediatric patients treated in consecutive UK AML trials. Leukemia. 2005. 19:2130–2138.4. Lie SO, Abrahamsson J, Clausen N, Forestier E, Hasle H, Hovi L, Jonmundsson G, Mellander L, Siimes MA, Yssing M, Zeller B, Gustafsson G. Nordic Society of Pediatric Hematology and Oncology (NOPHO). AML Study Group. Long-term results in children with AML: NOPHO-AML Study Group--report of three consecutive trials. Leukemia. 2005. 19:2090–2100.5. Ravindranath Y, Chang M, Steuber CP, Becton D, Dahl G, Civin C, Camitta B, Carroll A, Raimondi SC, Weinstein HJ. Pediatric Oncology Group. Pediatric Oncology Group (POG) studies of acute myeloid leukemia (AML): a review of four consecutive childhood AML trials conducted between 1981 and 2000. Leukemia. 2005. 19:2101–2116.6. Creutzig U, Zimmermann M, Ritter J, Reinhardt D, Hermann J, Henze G, Jürgens H, Kabisch H, Reiter A, Riehm H, Gadner H, Schellong G. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia. 2005. 19:2030–2042.7. Hamada A, Kawaguchi T, Nakano M. Clinical pharmacokinetics of cytarabine formulations. Clin Pharmacokinet. 2002. 41:705–718.8. Aoshima M, Tsukagoshi S, Sakurai Y, Oh-ishi JI, Ishida T, Kobayashi H. N4-Behenoyl-1-beta-D-arabinofuranosylcytosine as a potential new antitumor agent. Cancer Res. 1977. 37:2481–2486.9. Aoshima M, Tsukagoshi S, Sakurai Y, Oh-ishi J, Ishida T, Kobayashi H. Antitumor activities of newly synthesized N4-acyl-1-beta-D-arabinofuranosylcytosine. Cancer Res. 1976. 36:2726–2732.10. Nara N, Tohda S, Suzuki T, Nagata K, Yamashita Y, Imai Y, Maruyama Y, Tomiyama J. Effects of N4-behenoyl-1-beta-D-arabinofuranosylcytosine on blast progenitors of acute myeloblastic leukemia. Cancer Res. 1990. 50:7587–7592.11. Ohno R, Kato Y, Nagura E, Murase T, Okumura M, Yamada H, Ogura M, Minami S, Suzuki H, Morishima Y, Yokomaku S, Ezaki K, Kodera Y, Kawashima K, Saito H, Yamada K. Behenoyl cytosine arabinoside, daunorubicin, 6-mercaptopurine, and prednisolone combination therapy for acute myelogenous leukemia in adults and prognostic factors related to remission duration and survival length. J Clin Oncol. 1986. 4:1740–1747.12. Nagura E, Kimura K, Yamada K, Ohta K, Maekawa T, Takaku F, Uchino H, Masaoka T, Amaki I, Kawashima K, Kariyone S, Toyama K, Ichimaru M, Nomura T, Sakai Y, Takatsuki K, Hamajima N. Nationwide randomized comparative study of daunorubicin and aclarubicin in combination with behenoyl cytosine arabinoside, 6-mercaptopurine, and prednisolone for previously untreated acute myeloid leukemia. Cancer Chemother Pharmacol. 1994. 34:23–29.13. Park HS, Kim DW, Kim CC, Kim HK, Kim JS, Hwang TJ, Kim HJ, Kim HS, Song HS, Park JW, Ahn HS, Chung TJ, Cho KS, Lee KS, Choi YM. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen--a prospective, cooperative multicenter study. Semin Hematol. 1996. 33:4 Suppl 3. 24–29.14. Kobayashi T, Miyawaki S, Tanimoto M, Kuriyama K, Murakami H, Yoshida M, Minami S, Minato K, Tsubaki K, Ohmoto E, Oh H, Jinnai I, Sakamaki H, Hiraoka A, Kanamaru A, Takahashi I, Saito K, Naoe T, Yamada O, Asou N, Kageyama S, Emi N, Matsuoka A, Tomonaga M, Ohno R. The Japan Leukemia Study Group. Randomized trials between behenoyl cytarabine and cytarabine in combination induction and consolidation therapy, and with or without ubenimex after maintenance/intensification therapy in adult acute myeloid leukemia. J Clin Oncol. 1996. 14:204–213.15. Takashima Y. Clinical use of intermediate to high dose of N4-behenoyl-1-beta-D-arabinofuranosylcytosine in children with acute leukemia. J Clin Pharmacol. 1988. 28:356–362.16. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol. 1976. 33:451–458.17. Kimura K, Ohno R, Amaki I, Hattori K, Hirota Y, Hoshino A, Ichimaru M, Ito M, Kimura I, Maekawa T, Masaoka T, Nakamura T, Ogawa M, Oguro M, Ohta K, Osamura S, Shimoyama M, Takaku F, Uzuka Y, Yamada K. Treatment of acute myelogenous leukemia in adults with N4-behenoyl-1-beta-D-arabinofuranosylcytosine. Cancer. 1985. 56:1913–1917.18. Miyawaki S, Kobayashi T, Tanimoto M, Kuriyama K, Murakami H, Yoshida M, Minami S, Minato K, Tsubaki K, Omoto E, Oh H, Jinnai I, Sakamaki H, Hiraoka A, Kanamaru A, Takahashi I, Saito K, Naoe T, Yamada O, Asou N, Kageyama S, Emi N, Ueda T, Tomonaga M, Ohno R. The Japan Adult Leukemia Study Group. Comparison of leukopenia between cytarabine and behenoyl cytarabine in JALSG AML-89 consolidation therapy. Int J Hematol. 1999. 70:56–57.19. Ueda T, Nakamura T, Ando S, Kagawa D, Sasada M, Uchino H, Johno I, Akiyama Y. Pharmacokinetics of N4-behenoyl-1-beta-D-arabinofuranosylcytosine in patients with acute leukemia. Cancer Res. 1983. 43:3412–3416.20. Ravindranath Y, Yeager AM, Chang MN, Steuber CP, Krischer J, Graham-Pole J, Carroll A, Inoue S, Camitta B, Weinstein HJ. Pediatric Oncology Group. Autologous bone marrow transplantation versus intensive consolidation chemotherapy for acute myeloid leukemia in childhood. N Engl J Med. 1996. 334:1428–1434.21. Alonzo TA, Wells RJ, Woods WG, Lange B, Gerbing RB, Buxton AB, Neudorf S, Sanders J, Smith FO, Feig SA. Postremission therapy for children with acute myeloid leukemia: the children's cancer group experience in the transplant era. Leukemia. 2005. 19:965–970.22. Oliansky DM, Rizzo JD, Aplan PD, Arceci RJ, Leone L, Ravindranath Y, Sanders JE, Smith FO 3rd, Wilmot F, McCarthy PL Jr, Hahn T. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute myeloid leukemia in children: an evidencebased review. Biol Blood Marrow Transplant. 2007. 13:1–25.23. Marcucci G, Mrózek K, Ruppert AS, Maharry K, Kolitz JE, Moore JO, Mayer RJ, Pettenati MJ, Powell BL, Edwards CG, Sterling LJ, Vardiman JW, Schiffer CA, Carroll AJ, Larson RA, Bloomfield CD. Prognostic factors and outcome of core binding factor acute myeloid leukemia patients with t(8;21) differ from those of patients with inv(16): a Cancer and Leukemia Group B study. J Clin Oncol. 2005. 23:5705–5717.24. Narimatsu H, Yokozawa T, Iida H, Tsuzuki M, Hayakawa M, Takeo T, Iino M, Ichihashi T, Kato C, Sawamoto A, Sao H, Yanada M, Emi N, Kiyoi H, Yamaguchi T, Naoe T, Suzuki R, Sugiura I. Clinical characteristics and outcomes in patients with t(8;21) acute myeloid leukemia in Japan. Leukemia. 2008. 22:428–432.25. Meshinchi S, Alonzo TA, Stirewalt DL, Zwaan M, Zimmerman M, Reinhardt D, Kaspers GJ, Heerema NA, Gerbing R, Lange BJ, Radich JP. Clinical implications of FLT3 mutations in pediatric AML. Blood. 2006. 108:3654–3661.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combination chemotherapy with cytosine arabinoside and idarubicin for acute myelogenous leukemia
- Renission induction chemotherapy with idarubicin and cytosine arabinoside for the patients with acute myelogenous leukemia
- A Case of Acute Myelogenous Leukemia during Pregnancy
- Cytarabine and Idarubicin Induction Chemotherapy in Patients with Acute Myelogenous Leukemia
- A Case of Acute Leukemia Remitted by Adding Cyclosporin-A Previously Failed with Induction Therapy