J Korean Soc Radiol.
2014 Jul;71(1):6-13. 10.3348/jksr.2014.71.1.6.
Comparative Analysis of Tuberculous Lymphadenitis and Kikuchi Disease of the Neck
- Affiliations
-
- 1Department of Radiology, Cheonan Hospital, College of Medicine, Soonchunhyang University, Cheonan, Korea. mdhjk@schmc.ac.kr
- 2Department of Hemato-Oncology, Cheonan Hospital, College of Medicine, Soonchunhyang University, Cheonan, Korea.
- KMID: 1709014
- DOI: http://doi.org/10.3348/jksr.2014.71.1.6
Abstract
- PURPOSE
To compare the clinical and CT manifestations of Kikuchi disease (KD) and tuberculous lymphadenitis (TL).
MATERIALS AND METHODS
111 patients with TL (55 men, 56 women, mean age 38.6 years, range 13-80 years) and 73 patients with KD (24 men, 49 women, mean age 26.8 years, range 8-61 years) were included in the study. Two observers independently compared sex, age, peripheral white blood cells, erythrocyte sedimentation rate (ESR), nodal distribution, nodal bilaterality, perinodal fat infiltration, muscle abscess, nodal conglomeration, necrotic and non-necrotic lymph nodes in the patients with TL and KD.
RESULTS
KD patients showed a female predominance (67.1%). Patients with TL were older. Leukocytopenia and increased ESR were more frequent in patients with KD. KD more commonly affected lymph nodes in level II, III, and V, while TL more commonly involved lymph nodes in the upper paratracheal area. Perinodal fat infiltration was more frequent in KD. Muscle abscess was seen in patients with TL only (14%). Necrotic lymph nodes were more frequent in TL. A thin type was more frequent in TL.
CONCLUSION
KD showed female predominance, leukocytopenia, increased ESR, involvement of levels II, III, and V and frequent perinodal fat infiltration. TL patients were older than KD patients, were commonly affected in the upper paratracheal area, abscesses were shown only in this group and thin type necrotic lymph nodes were more frequent.
MeSH Terms
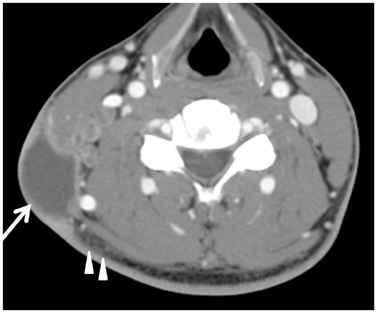
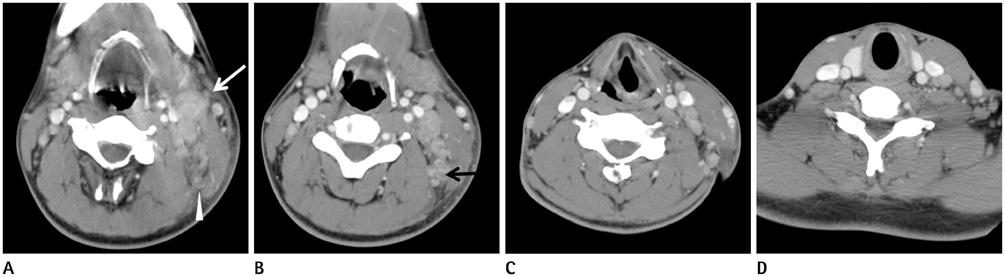
Figure
Reference
-
1. Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes: a clinicopathological study. Acta Hematol Jpn. 1972; 35:379–380.2. Primrose WJ, Napier SS, Primrose AJ. Kikuchi-Fugimoto disease (Cervical Subacute Necrotising Lymphadenitis): an important benign disease often masquerading as lymphoma. Ulster Med J. 2009; 78:134–136.3. Schwetschenau E, Kelley DJ. The adult neck mass. Am Fam Physician. 2002; 66:831–838.4. Bennie MJ, Bowles KM, Rankin SC. Necrotizing cervical lymphadenopathy caused by Kikuchi-Fujimoto disease. Br J Radiol. 2003; 76:656–658.5. Ahuja A, Ying M, Yuen YH, Metreweli C. Power Doppler sonography to differentiate tuberculous cervical lymphadenopathy from nasopharyngeal carcinoma. AJNR Am J Neuroradiol. 2001; 22:735–740.6. Altuntas F, Sari I, Canoz O, Yildiz O, Eser B, Cetin M, et al. Kikuchi-Fujimoto disease: a rare but important cause of fever and lymphadenopathy in pregnant women. Am J Hematol. 2006; 81:118–120.7. Campbell IA, Ormerod LP, Friend JA, Jenkins PA, Prescott RJ. Six months versus nine months chemotherapy for tuberculosis of lymph nodes: final results. Respir Med. 1993; 87:621–623.8. Na DG, Chung TS, Byun HS, Kim HD, Ko YH, Yoon JH. Kikuchi disease: CT and MR findings. AJNR Am J Neuroradiol. 1997; 18:1729–1732.9. Song JY, Cheong HJ, Kee SY, Lee J, Sohn JW, Kim MJ, et al. Disease spectrum of cervical lymphadenitis: analysis based on ultrasound-guided core-needle gun biopsy. J Infect. 2007; 55:310–316.10. Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY. CT findings in Kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol. 2004; 25:1099–1102.11. Shah JP, Strong E, Spiro RH, Vikram B. Surgical grand rounds. Neck dissection: current status and future possibilities. Clin Bull. 1981; 11:25–23.12. Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol. 2004; 122:141–152.13. Kucukardali Y, Solmazgul E, Kunter E, Oncul O, Yildirim S, Kaplan M. Kikuchi-Fujimoto Disease: analysis of 244 cases. Clin Rheumatol. 2007; 26:50–54.14. Choi EC, Moon WJ, Lim YC. Case report. Tuberculous cervical lymphadenitis mimicking metastatic lymph nodes from papillary thyroid carcinoma. Br J Radiol. 2009; 82:e208–e211.15. Jha BC, Dass A, Nagarkar NM, Gupta R, Singhal S. Cervical tuberculous lymphadenopathy: changing clinical pattern and concepts in management. Postgrad Med J. 2001; 77:185–187.16. Castro DJ, Hoover L, Castro DJ, Zuckerbraun L. Cervical mycobacterial lymphadenitis. Medical vs surgical management. Arch Otolaryngol. 1985; 111:816–810.17. Kuo TT. Kikuchi's disease (histiocytic necrotizing lymphadenitis). A clinicopathologic study of 79 cases with an analysis of histologic subtypes, immunohistology, and DNA ploidy. Am J Surg Pathol. 1995; 19:798–809.18. Fontanilla JM, Barnes A, von Reyn CF. Current diagnosis and management of peripheral tuberculous lymphadenitis. Clin Infect Dis. 2011; 53:555–562. World Health Organization. Global tuberculosis control annual reports from 1997 to 2008. Geneva, Switzerland: WHO, 2008. Available at: http://www.who.int/tb/publications/en/. Accessed on: April 20, 2008.19. Schofer JM, Tong TC, Tanen DA. Kikuchi's disease: a rare cause of cervical lymphadenitis and fever. J Emerg Med. 2005; 29:151–153.20. Jayaraj SM, Lloyd J, Frosh AC, Patel KS. Kikuchi-Fujimoto's syndrome masquerading as tuberculosis. J Laryngol Otol. 1999; 113:82–84.21. Chen YM, Lee PY, Su WJ, Perng RP. Lymph node tuberculosis: 7-year experience in Veterans General Hospital, Taipei, Taiwan. Tuber Lung Dis. 1992; 73:368–371.22. Parappil A, Rifaath AA, Doi SA, Pathan E, Surrun SK. Pyrexia of unknown origin: Kikuchi-Fujimoto disease. Clin Infect Dis. 2004; 39:138–143.23. Lin HC, Su CY, Huang CC, Hwang CF, Chien CY. Kikuchi's disease: a review and analysis of 61 cases. Otolaryngol Head Neck Surg. 2003; 128:650–653.24. Felgar RE, Furth EE, Wasik MA, Gluckman SJ, Salhany KE. Histiocytic necrotizing lymphadenitis (Kikuchi's disease): in situ end-labeling, immunohistochemical, and serologic evidence supporting cytotoxic lymphocyte-mediated apoptotic cell death. Mod Pathol. 1997; 10:231–241.25. Hassan M, Anees A, Zaheer S. Kikuchi-fujimoto disease: diagnostic dilemma and the role of immunohistochemistry. J Clin Med Res. 2009; 1:244–246.26. Som PM, Curtin HD, Mancuso AA. Imaging-based nodal classification for evaluation of neck metastatic adenopathy. AJR Am J Roentgenol. 2000; 174:837–844.27. Han HJ, Lim GY, Yeo DM, Chung NG. Kikuchi's disease in children: clinical manifestations and imaging features. J Korean Med Sci. 2009; 24:1105–1109.28. Kato H, Kanematsu M, Kato Z, Teramoto T, Kondo N, Hirose Y, et al. MR imaging findings of cervical lymphadenopathy in patients with Kikuchi disease. Eur J Radiol. 2011; 80:e576–e581.29. Iqbal M, Subhan A, Aslam A. Papillary thyroid carcinoma with tuberculous cervical lymphadenopathy mimicking metastasis. J Coll Physicians Surg Pak. 2011; 21:207–209.30. Solak O, Sayar A, Metin M, Erdoğu V, Cuhadaroğlu S, Turna A, et al. The coincidence of mediastinal tuberculosis lymphadenitis in lung cancer patients. Acta Chir Belg. 2005; 105:180–182.31. Kang SJ, Kim YH, Jung CY, Lee HJ, Hyun MC. Clinical characteristics and radiologic patterns of adelescents with pulmonary tuberculosis: relevance to the reactive tuberculosis. Pediatr Allergy Respir Dis. 2012; 22:163–170.32. Leung AN. Pulmonary tuberculosis: the essentials. Radiology. 1999; 210:307–322.33. Sarwar A, Haque AU, Aftab S, Mustafa M, Moatasim A, Siddique S, et al. Spectrum of Morphological Changes in Tuberculous Lymphadenitis. Int J Pathol. 2004; 2:85–89.34. Teo SY, Ong CL. Clinics in diagnostic imaging (108). Tuberculous dactylitis of the thumb, mediastinal and left hilar lymphadenopathy, and probable left cervical lymphadenopathy. Singapore Med J. 2006; 47:243–249. quiz 250.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Histiocytic Necrotizing Lymphadenitis(Kikuchi's Disease) A clinicopathologic study of 1 cases
- Comparison of Ultrasonographic Findings of Biopsy-Proven Tuberculous Lymphadenitis and Kikuchi Disease
- Clinical and Radiologic Characteristics of Kikuchi's Disease
- A Case of Kikuchi's Disease Associated with Hemophagocytic Syndrome
- Two Cases of Hemophagocytic Lymphohistiocytosis Following Kikuchi's Disease