J Gynecol Oncol.
2014 Apr;25(2):118-123. 10.3802/jgo.2014.25.2.118.
Clinicopathologic features of epithelial ovarian carcinoma in younger vs. older patients: analysis in Japanese women
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Nagoya University Graduate School of Medicine, Nagoya, Japan. kajiyama@med.nagoya-u.ac.jp
- 2Department of Obstetrics and Gynecology, Toyohashi Municipal Hospital, Toyohashi, Japan.
- 3Department of Medical Technology, Nagoya University School of Health Science, Nagoya, Japan.
- KMID: 1708334
- DOI: http://doi.org/10.3802/jgo.2014.25.2.118
Abstract
OBJECTIVE
The purpose of this study was to clarify the clinical features of epithelial ovarian carcinoma (EOC) in younger vs. older patients in Japan.
METHODS
We collected data on 1,562 patients with EOC treated at multiple institutions in the Tokai Ovarian Tumor Study Group, and analyzed them retrospectively. All patients were divided into 2 groups: group A (< or =40 years old) and group B (>40 years old). The data were analyzed to evaluate prognostic factors and the distribution of features in each group. Patients were subjected to univariate and multivariate analyses to evaluate overall survival (OS).
RESULTS
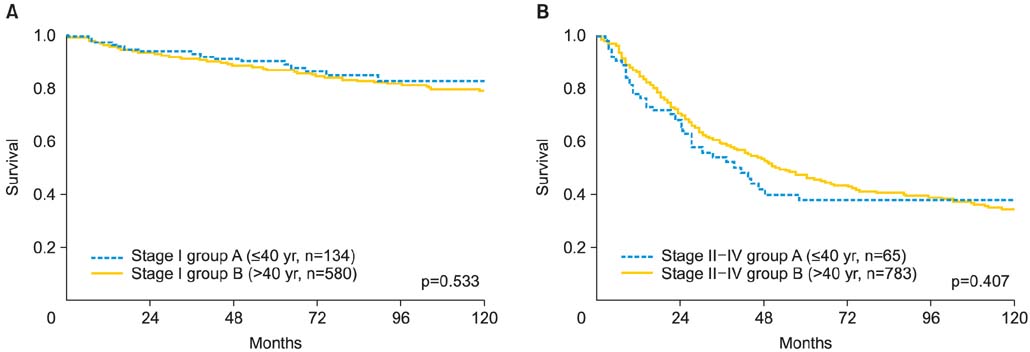
The median follow-up time was 45.1 months (range, 1 to 257 months). Patients in group A had a significantly higher rate of stage I disease (67.3% vs. 42.6%, respectively; p<0.001) and the mucinous type (36.7% vs. 13.5%, respectively; p<0.001) than those in group B. There was a significant difference of OS between the 2 groups (p=0.013). However, upon stratification according to the stage, there were no significant differences in the OS between the 2 groups (group A vs. B: stage I, p=0.533; stage II-IV, p=0.407). Multivariate analysis revealed that younger age was not an independent prognostic factor for OS.
CONCLUSION
On the basis of our data, younger patients had a different clinical profile than older patients, particularly regarding the stage of the disease and pathological distribution; however, they showed a similar long-term prognosis, even upon stratification according to the stage.
MeSH Terms
Figure
Reference
-
1. Japan Society of Gynecologic Oncology. Ovarian treatment guidelines 2010. Tokyo: Kanehara;2010.2. Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics, 2001. CA Cancer J Clin. 2001; 51:15–36.3. Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004; 54:8–29.4. Lindemann K, Christensen RD, Vergote I, Stuart G, Izquierdo MA, Kaern J, et al. First-line treatment of advanced ovarian cancer with paclitaxel/carboplatin with or without epirubicin (TEC versus TC): a gynecologic cancer intergroup study of the NSGO, EORTC GCG and NCIC CTG. Ann Oncol. 2012; 23:2613–2619.5. Katsumata N, Yasuda M, Isonishi S, Takahashi F, Michimae H, Kimura E, et al. Long-term results of dose-dense paclitaxel and carboplatin versus conventional paclitaxel and carboplatin for treatment of advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer (JGOG 3016): a randomised, controlled, open-label trial. Lancet Oncol. 2013; 14:1020–1026.6. Bozas G, Dimopoulos MA, Kastritis E, Efstathiou E, Koutsoukou V, Rodolakis A, et al. Young age is associated with favorable characteristics but is not an independent prognostic factor in patients with epithelial ovarian cancer: a single institution experience. Oncology. 2006; 70:265–272.7. Duska LR, Chang YC, Flynn CE, Chen AH, Goodman A, Fuller AF, et al. Epithelial ovarian carcinoma in the reproductive age group. Cancer. 1999; 85:2623–2629.8. Rodriguez M, Nguyen HN, Averette HE, Steren AJ, Penalver MA, Harrison T, et al. National survey of ovarian carcinoma XII: epithelial ovarian malignancies in women less than or equal to 25 years of age. Cancer. 1994; 73:1245–1250.9. Smedley H, Sikora K. Age as a prognostic factor in epithelial ovarian carcinoma. Br J Obstet Gynaecol. 1985; 92:839–842.10. Fruscio R, Corso S, Ceppi L, Garavaglia D, Garbi A, Floriani I, et al. Conservative management of early-stage epithelial ovarian cancer: results of a large retrospective series. Ann Oncol. 2013; 24:138–144.11. Kajiyama H, Shibata K, Mizuno M, Hosono S, Kawai M, Nagasaka T, et al. Fertility-sparing surgery in patients with clear-cell carcinoma of the ovary: is it possible? Hum Reprod. 2011; 26:3297–3302.12. Satoh T, Hatae M, Watanabe Y, Yaegashi N, Ishiko O, Kodama S, et al. Outcomes of fertility-sparing surgery for stage I epithelial ovarian cancer: a proposal for patient selection. J Clin Oncol. 2010; 28:1727–1732.13. Schilder JM, Thompson AM, DePriest PD, Ueland FR, Cibull ML, Kryscio RJ, et al. Outcome of reproductive age women with stage IA or IC invasive epithelial ovarian cancer treated with fertility-sparing therapy. Gynecol Oncol. 2002; 87:1–7.14. Zanetta G, Chiari S, Rota S, Bratina G, Maneo A, Torri V, et al. Conservative surgery for stage I ovarian carcinoma in women of childbearing age. Br J Obstet Gynaecol. 1997; 104:1030–1035.15. Chan JK, Urban R, Cheung MK, Osann K, Shin JY, Husain A, et al. Ovarian cancer in younger vs older women: a population-based analysis. Br J Cancer. 2006; 95:1314–1320.16. Rusell P. Surgical pathology of the ovaries. New York: Churchill Livingstone;1989.17. Kennedy AW, Biscotti CV, Hart WR, Webster KD. Ovarian clear cell adenocarcinoma. Gynecol Oncol. 1989; 32:342–349.18. Kajiyama H, Shibata K, Suzuki S, Ino K, Nawa A, Kawai M, et al. Fertility-sparing surgery in young women with invasive epithelial ovarian cancer. Eur J Surg Oncol. 2010; 36:404–408.19. Kajiyama H, Shibata K, Mizuno M, Umezu T, Suzuki S, Nawa A, et al. Long-term survival of young women receiving fertility-sparing surgery for ovarian cancer in comparison with those undergoing radical surgery. Br J Cancer. 2011; 105:1288–1294.20. Kajiyama H, Shibata K, Suzuki S, Ino K, Yamamoto E, Mizuno K, et al. Is there any possibility of fertility-sparing surgery in patients with clear-cell carcinoma of the ovary? Gynecol Oncol. 2008; 111:523–526.21. Morice P, Leblanc E, Rey A, Baron M, Querleu D, Blanchot J, et al. Conservative treatment in epithelial ovarian cancer: results of a multicentre study of the GCCLCC (Groupe des Chirurgiens de Centre de Lutte Contre le Cancer) and SFOG (Société Francaise d'Oncologie Gynécologique). Hum Reprod. 2005; 20:1379–1385.22. Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT, et al. Outcomes of fertility-sparing surgery for invasive epithelial ovarian cancer: oncologic safety and reproductive outcomes. Gynecol Oncol. 2008; 110:345–353.23. Massi D, Susini T, Savino L, Boddi V, Amunni G, Colafranceschi M. Epithelial ovarian tumors in the reproductive age group: age is not an independent prognostic factor. Cancer. 1996; 77:1131–1136.24. Kajiyama H, Shibata K, Mizuno M, Nawa A, Mizuno K, Matsuzawa K, et al. Fertility-sparing surgery in young women with mucinous adenocarcinoma of the ovary. Gynecol Oncol. 2011; 122:334–338.25. Chan JK, Loizzi V, Lin YG, Osann K, Brewster WR, DiSaia PJ. Stages III and IV invasive epithelial ovarian carcinoma in younger versus older women: what prognostic factors are important? Obstet Gynecol. 2003; 102:156–161.26. Herrinton LJ, Stanford JL, Schwartz SM, Weiss NS. Ovarian cancer incidence among Asian migrants to the United States and their descendants. J Natl Cancer Inst. 1994; 86:1336–1339.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expression of c-Met in ovarian epithelial tumor
- Current status of gynecologic cancer in Japan
- Analysis of Clinicopathologic Features in Papillary Thyroid Carcinoma Patients Younger than Thirty
- A rare case of pure-type embryonal carcinoma in a 75-year-old woman mimicking epithelial ovarian carcinoma
- Incidence and treatment outcomes of ovarian carcinosarcoma from the national cancer registry of Korea