Korean J Urogenit Tract Infect Inflamm.
2013 Oct;8(2):102-108. 10.14777/kjutii.2013.8.2.102.
Prevalence of Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, Ureaplasma urealyticum in Chronic Prostatitis Category IIIa and IIIb Patients Using Polymerase Chain Reaction
- Affiliations
-
- 1Department of Urology, National Police Hospital, Seoul, Korea. msk0701@hanmail.net
- 2Department of Laboratory Medicine, National Police Hospital, Seoul, Korea.
- KMID: 1502115
- DOI: http://doi.org/10.14777/kjutii.2013.8.2.102
Abstract
- PURPOSE
The aim of this study was to report on the prevalence of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), Mycoplasma genitalium (MG), and Ureaplasma urealyticum (UU) in patients with chronic prostatitis (CP) IIIa and CP IIIb using PCR and correlations between four microorganisms and other clinical parameters.
MATERIALS AND METHODS
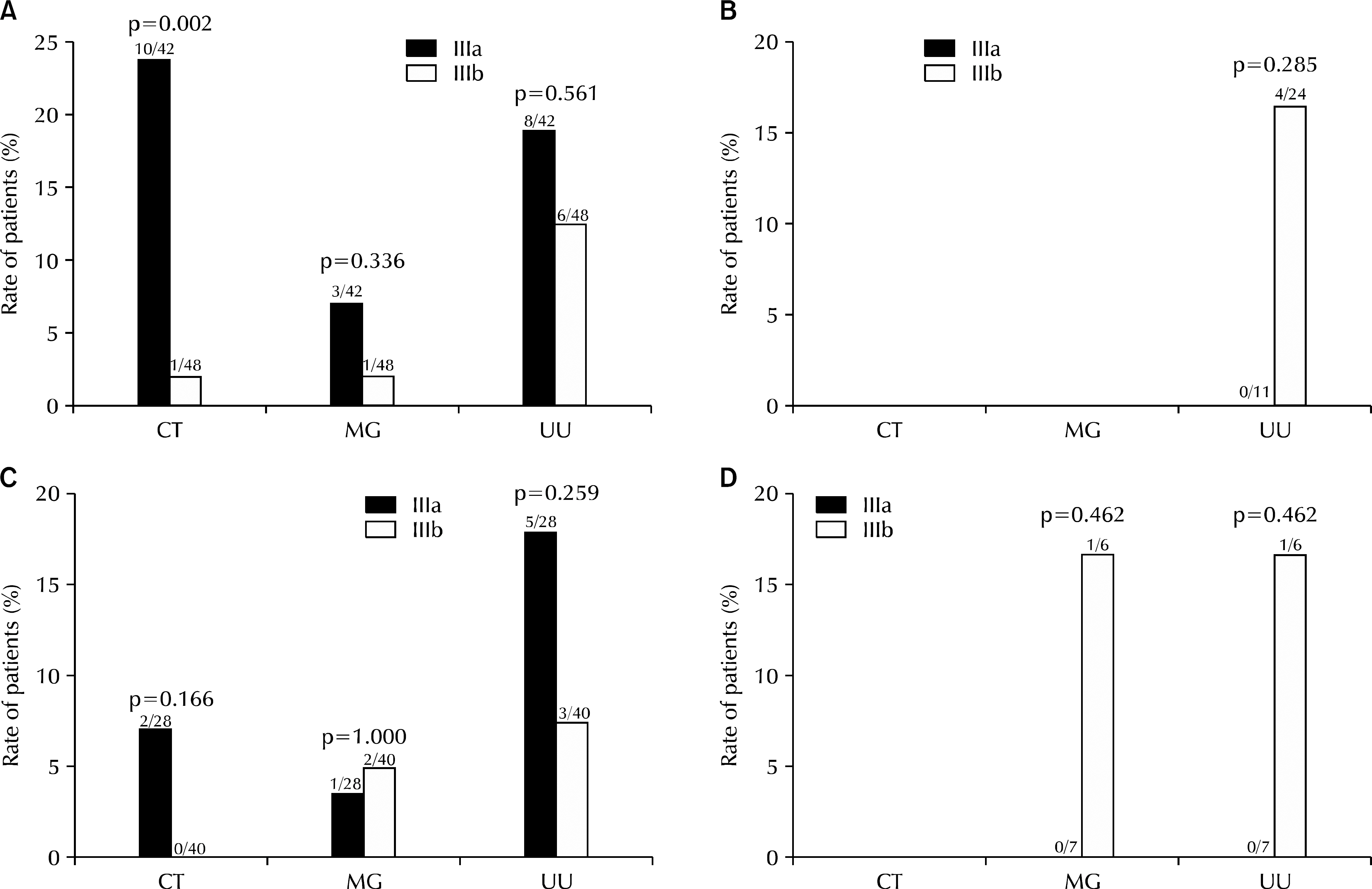
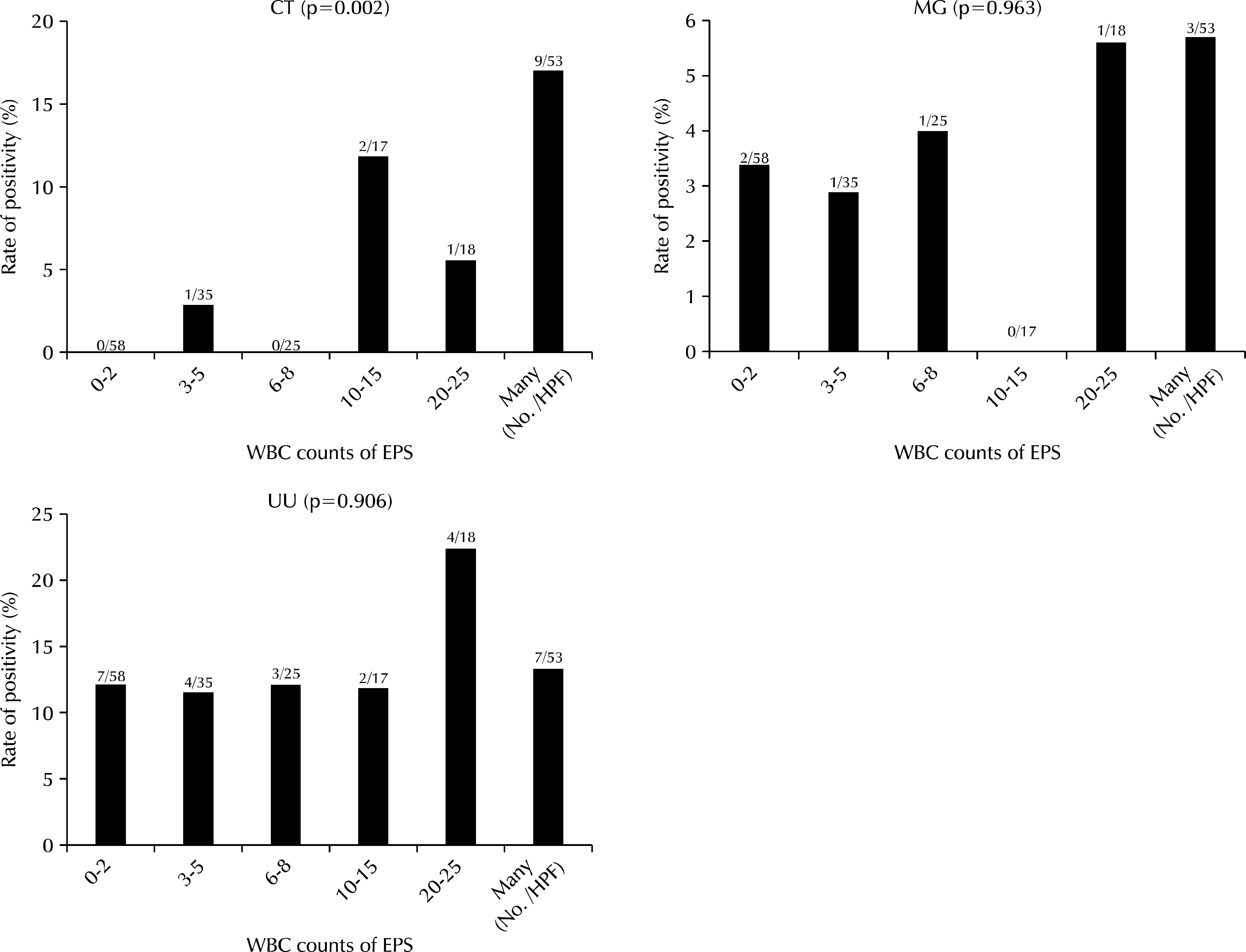
The medical charts of 206 Patients who visited National Police Hospital and were diagnosed with CP IIIa and CP IIIb between January 2011 and December 2012 were reviewed. We investigated white blood cell (WBC) counts on expressed prostatic secretion (EPS) samples and the frequency of four possible causative microorganisms of prostatitis, CT, NG, MG, and UU, using PCR techniques on first voided urine samples (VB1).
RESULTS
Of 206 patients, 88 patients were CP IIIa and 118 were CP IIIb, with a mean age of 33.8+/-12.9 and 34.6+/-11.3, respectively. CT, NG, MG, and UU were detected in 13.6%, 0%, 4.5%, and 14.8% of CP IIIa patients and in 0.8%, 0%, 3.4%, and 11.9% of CP IIIb patients, respectively. Among men aged 19-30, detection of CT was significantly greater in the CP IIIa group than in the CP IIIb group (p=0.002). CT showed a positive association with EPS or the third voided urine (VB3) WBC count grade (p<0.01), however, MG and UU did not. The relationship between numbers of detected microorganisms and WBC counts was statistically insignificant.
CONCLUSIONS
In subgroup analyses, microorganisms were detected in by PCR in 29 CP IIIa patients (32.9%) and 19 CP IIIb patients (16.1%). Young aged men in the CP IIIa group showed high prevalence of CT, and patients in whom CT was detected in urine PCR had high EPS WBC counts.
Keyword
MeSH Terms
Figure
Reference
-
1. Ku JH, Lee SH, Jeon YS, Kim ME, Lee NK, Park YH. Epidemiologic study of chronic prostatitis-like symptoms surveyed among young men in the area of Taejeon and Chungnam: prevalence and influence of weather. Korean J Urol. 2002; 43:318–21.2. Shoskes DA, Landis JR, Wang Y, Nickel JC, Zeitlin SI, Nadler R. Chronic Prostatitis Collaborative Research Network Study Group. Impact of post-ejaculatory pain in men with category III chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2004; 172:542–7.
Article3. Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominent urogenital symptoms of “chronic prostatitis”. Urology. 1996; 48:715–21.
Article4. Pontari MA. Chronic prostatitis/chronic pelvic pain syndrome. Urol Clin North Am. 2008; 35:81–9.
Article5. Schaeffer AJ. Epidemiology and evaluation of chronic pelvic pain syndrome in men. Int J Antimicrob Agents. 2008; 31(Suppl 1):S108–11.
Article6. Cho IC, Min SK. Asymptomatic prostatitis: clinical significances and management. Korean J Urogenit Tract Infect Inflamm. 2013; 8:13–9.
Article7. Nickel JC, Nyberg LM, Hennenfent M. Research guidelines for chronic prostatitis: consensus report from the first National Institutes of Health International Prostatitis Collaborative Network. Urology. 1999; 54:229–33.
Article8. Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001; 165:842–5.
Article9. Nadler RB, Schaeffer AJ. Lower urinary tract cultures. Nickel JC, editor. Textbook of prostatitis. 1st ed.Oxford, England: Isis Medical Media;1999. p. 201–6.10. Schaeffer AJ, Landis JR, Knauss JS, Propert KJ, Alexander RB, Litwin MS, et al. Chronic Prostatitis Collaborative Research Network Group. Demographic and clinical characteristics of men with chronic prostatitis: the national institutes of health chronic prostatitis cohort study. J Urol. 2002; 168:593–8.
Article11. Krieger JN, Riley DE. Chronic prostatitis: charlottesville to Seattle. J Urol. 2004; 172:2557–60.
Article12. de la Rosette JJ, Hubregtse MR, Karthaus HF, Debruyne FM. Results of a questionnaire among Dutch urologists and general practitioners concerning diagnostics and treatment of patients with prostatitis syndromes. Eur Urol. 1992; 22:14–9.
Article13. Moon TD. Questionnaire survey of urologists and primary care physicians' diagnostic and treatment practices for prostatitis. Urology. 1997; 50:543–7.
Article14. Lee KS, Choi JD. Chronic prostatitis: approaches for best management. Korean J Urol. 2012; 53:69–77.
Article15. Johnson RE, Green TA, Schachter J, Jones RB, Hook EW 3rd, Black CM, et al. Evaluation of nucleic acid amplification tests as reference tests for Chlamydia trachomatis infections in asymptomatic men. J Clin Microbiol. 2000; 38:4382–6.16. Kim TH, Kim TH, Kim HR, Lee MK, Myung SC, Kim YS. Detection of cryptic microorganisms in patients with chronic prostatitis by multiplex polymerase chain reaction. Korean J Urol. 2007; 48:304–9.
Article17. Seo KI, Hwang JC, Kim TW, Lee SH, Park SY, Roh SH. Results of microorganism detection by multiplex polymerase chain reaction in patients with chronic pelvic pain syndrome. Korean J Urol. 2009; 50:1120–4.
Article18. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999; 282:236–7.
Article19. Kim SW, Lee JY, Park WJ, Cho YH, Yoon MS. The diagnostic values of the polymerase chain reaction in prostatitis. Korean J Infect Dis. 2000; 32:265–73.20. Ha JS, Kim SW, Cho YH. Detection of cryptic microorganisms by polymerase chain reaction assay in chronic pelvic pain syndrome. Korean J Urol. 2002; 43:396–401.21. Krieger JN, Riley DE, Roberts MC, Berger RE. Prokaryotic DNA sequences in patients with chronic idiopathic prostatitis. J Clin Microbiol. 1996; 34:3120–8.
Article22. Brookings C, Goldmeier D, Sadeghi-Nejad H. Sexually transmitted infections and sexual function in relation to male fertility. Korean J Urol. 2013; 54:149–56.
Article23. Mouton JW, Verkooyen R, van der Meijden WI, van Rijsoort-Vos TH, Goessens WH, Kluytmans JA, et al. Detection of Chlamydia trachomatis in male and female urine specimens by using the amplified Chlamydia trachomatis test. J Clin Microbiol. 1997; 35:1369–72.
Article24. Lee YS, Lee KS. Chlamydia and male lower urinary tract diseases. Korean J Urol. 2013; 54:73–7.25. Kim SJ, Lee DS, Lee SJ. The prevalence and clinical significance of urethritis and cervicitis in asymptomatic people by use of multiplex polymerase chain reaction. Korean J Urol. 2011; 52:703–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of Cryptic Microorganisms by Polymerase Chain Reaction Assay in Chronic Pelvic Pain Syndrome
- The Prevalence and Clinical Significance of Urethritis and Cervicitis in Asymptomatic People by Use of Multiplex Polymerase Chain Reaction
- PCR-based Investigation of Infection Patterns in Patients with Pelvic Inflammatory Diseases in Jeju
- Comparison of the Anyplex II STI-7 and Seeplex STD6 ACE Detection Kits for the Detection of Sexually Transmitted Infections
- Detection of Cryptic Microorganisms in Patients with Chronic Prostatitis by Multiplex Polymerase Chain Reaction