Infect Chemother.
2009 Aug;41(4):233-235. 10.3947/ic.2009.41.4.233.
A Case of Syphilitic Uveitis in an Immunocompetent Patient
- Affiliations
-
- 1Department of Internal Medicine, Gachon University of Medicine and Science, Gil Hospital, Incheon, Korea. yspark@gilhospital.com
- 2Department of Ophthalmology, Gachon University of Medicine and Science, Gil Hospital, Incheon, Korea.
- 3Department of Laboratory Medicine, Gachon University of Medicine and Science, Gil Hospital, Incheon, Korea.
- KMID: 1473669
- DOI: http://doi.org/10.3947/ic.2009.41.4.233
Abstract
- Syphilis is re-emerging worldwide due to the HIV epidemic. Prior to the introduction of penicillin, syphilis was the second most common primary cause of all cases of uveitis. Today, ocular syphilis is a rare disease, especially in an immunocompetent patient. Variable manifestation without pathognomonic signs of ocular syphilis often lead to delayed diagnosis, resulted in irreversibile loss of vision. In Korea, syphilitic uveitis has not been reported in an immunocompetent patient since 1984. We experienced a case of syphilitic uveitis in an immunocompetent man with visual deterioration. As the incidence of syphilis is increasing in these days, a high degree of clinical suspicion should be considered in patients with unexplained ocular inflammation and visual disturbances.
MeSH Terms
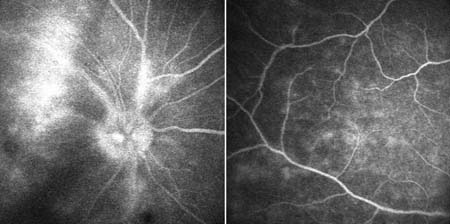
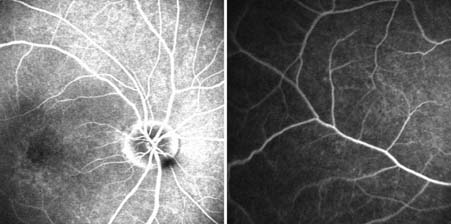
Figure
Reference
-
1. Gaudio PA. Update on ocular syphilis. Curr Opin Ophthalmol. 2006. 17:562–566.
Article2. Park HJ. Clinical Observation and Statistical Consideration of Syphilis (2000-2007). Korean J Dermatol. 2008. 46:1344–1352.3. Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. 2005. 20:161–167.
Article4. Parc CE, Chahed S, Patel SV, Salmon-Ceron D. Manifestations and treatment of ocular syphilis during an epidemic in France. Sex Transm Dis. 2007. 34:553–556.
Article5. Maves RC, Cachay ER, Young MA, Fierer J. Secondary syphilis with ocular manifestations in older adults. Clin Infect Dis. 2008. 46:e142–e145.
Article6. Jaun SI, Kim CG, Hong SH. A Case of Late Seronegative Ocular Syphilis. J Korean Ophthalmol Soc. 1984. 25:533–536.7. Yoo KS, Kim YH. 3 Cases of Interstitial Keratitis Occurred in Congenital Syphilitic Patients. J Korean Ophthalmol Soc. 1981. 22:427–431.8. Jeong HW, Jung SJ, Kim MG, Kee SY, Suh SY, Song JS, Kim MJ. A case of the human immunodeficiency virus type 1-infected patient presented as a syphilitic papillitis. Korean J Med. 2005. 68:238–242.9. Kim EH, Lee JE. A Case of Vitritis as the Primary Manifestation without Retinitis in Ocular Syphilis with AIDS. J Korean Ophthalmol Soc. 2006. 47:1177–1182.10. Oh HG, Yang KI. A Case of Optic Perineuritis Associated with Seronegative Neurosyphilis. J Korean Geriatr Soc. 2007. 11:98–100.11. Song JH, Hong YT, Kwon OW. Acute syphilitic posterior placoid chorioretinitis following intravitreal triamcinolone acetonide injection. Graefes Arch Clin Exp Ophthalmol. 2008. 246:1775–1778.
Article12. Yoon KC, Im SK, Seo MS, Park YG. Neurosyphilitic episcleritis. Acta Ophthalmol Scand. 2005. 83:265–266.
Article13. Hong MC, Sheu SJ, Wu TT, Chuang CT. Ocular uveitis as the initial presentation of syphilis. J Chin Med Assoc. 2007. 70:274–280.
Article14. Thami GP, Kaur S, Gupta R, Kanwar AJ, Sood S. Syphilitic panuveitis and asymptomatic neurosyphilis: a marker of HIV infection. Int J STD AIDS. 2001. 12:754–756.
Article15. Centers for Disease Control and Prevention. Workowski KA, Berman SM. Sexually transmitted diseases treatment guidelines, 2006. MMWR Recomm Rep. 2006. 55:1–94.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Syphilitic Keratoderma Concurrent with Syphilitic Uveitis
- A Case of Cytomegalovirus Retinitis Following Intravitreal Dexamethasone Implant in an Immunocompetent Patient with Uveitis
- Clinical Manifestations of Syphilitic Uveitis in the Korean Population
- A case of the human immunodeficiency virus type 1-infected patient presented as a syphilitic papillitis
- Syphilitic gastritis: a case report