Korean J Pediatr Gastroenterol Nutr.
2010 Mar;13(1):36-43. 10.5223/kjpgn.2010.13.1.36.
Factors Contributing to Treatment Outcome of Functional Constipation in Children
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Pusan National University, Busan, Korea. jhongpark@pusan.ac.kr
- 2Department of Pediatrics, School of Medicine, Kosin University, Busan, Korea.
- KMID: 1459442
- DOI: http://doi.org/10.5223/kjpgn.2010.13.1.36
Abstract
- PURPOSE
The aim of this study was to evaluate the clinical features and factors contributing to treatment outcome for chronic functional constipation in children.
METHODS
We analyzed the medical records of patients with constipation, who visited the inpatient or outpatient clinic of the Department of Pediatrics of Pusan National University Hospital, between January 1998 and December 2007. The clinical features, outcomes, and factors affecting the treatment response according to the main drug (lactulose vs. PEG 4000) were analyzed retrospectively.
RESULTS
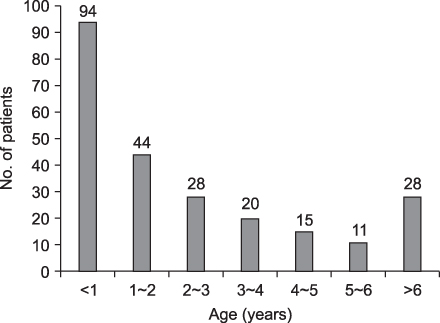
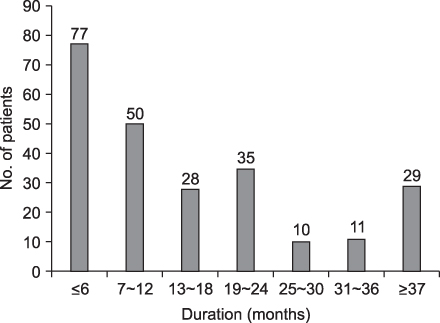
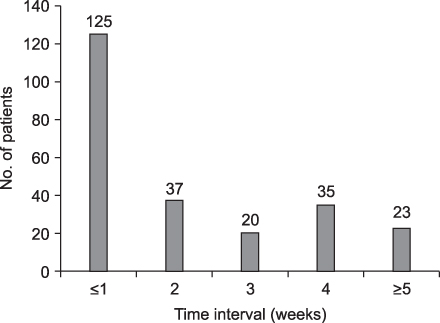
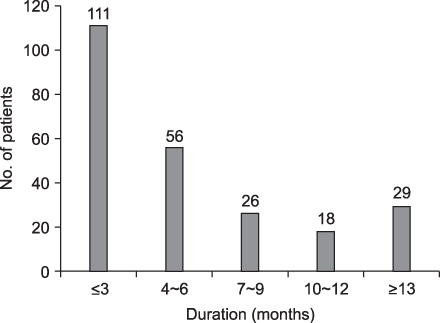
Two hundred forty children (142 males and 98 females) were enrolled in this study. The mean age was 51.2+/-37.9 months. The duration of symptoms was 32.6+/-33.7 months. The accompanying symptoms were as follows: encopresis, 91 (30.4%); abdominal pain, 76 (31.6%); and blood-tinged stool, 37 (15.4%). The treatment response was achieved earlier in females (p<0.001), patients with accompanying symptoms (p<0.05), and patients treated with PEG 4000 (p=0.001). The duration of symptoms (p<0.05) and stool frequency before treatment (p<0.05) were related to a delayed treatment response. Relapse occurred in 7 children, all of whom were treated successfully later.
CONCLUSION
Factors contributing to treatment response are female gender, accompanying symptoms, duration of symptoms, and stool frequency before treatment. PEG 4000 is superior to lactulose in response time and taken into consideration as a primary drug for the treatment of functional constipation of children. Early treatment and sufficient treatment time may also be important factors to achieve an early response and prevent relapse.
Keyword
MeSH Terms
Figure
Reference
-
1. Loening-Baucke V. Prevalence, symptoms and outcome of constipation in infants and toddlers. J Pediatr. 2005. 146:359–363.
Article2. Loening-Baucke V. Prevalence rates for constipation and faecal and urinary incontinence. Arch Dis Child. 2007. 92:486–489.
Article3. Baker SS, Liptak GS, Colletti RB, Croffie JM, Di Lorenzo C, Ector W, et al. Constipation in infants and children: evaluation and treatment. A medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 1999. 29:612–626.4. Borowitz SM, Cox DJ, Tam A, Ritterband LM, Sutphen JL, Penberthy JK. Precipitants of constipation during early childhood. J Am Board Fam Pract. 2003. 16:213–218.
Article5. Dupont C, Leluyer B, Maamri N, Morali A, Joye JP, Fiorini JM, et al. Double-blind randomized evaluation of clinical and biological tolerance of polyethylene glycol 4000 versus lactulose in constipated children. J Pediatr Gastroenterol Nutr. 2005. 41:625–633.
Article6. Loening-Baucke V. Polyethylene glycol without electrolytes for children with constipation and encopresis. J Pediatr Gastroenterol Nutr. 2002. 34:372–377.
Article7. Lee JH, Lee R, Bae SH. Efficacy and safety of electrolytes-free polyethylene glycol (PEG) 4000 for disimpaction in children with chronic functional constipation. Korean J Pediatr. 2008. 51:391–395.
Article8. Uhm JH. Comparison of polyethylene glycol 4000 and lactulose for treatment of chronic functional constipation in children. Korean J Pediatr. 2007. 50:752–756.
Article9. Ahn YJ, Park JO. Clinical outcome and long term follow-up of chronic functional constipation in children. Korean J Pediatr Gastroenterol Nutr. 2006. 9:200–209.
Article10. Loening-Baucke V. Factors responsible for persistence of childhood constipation. J Pediatr Gastroenterol Nutr. 1987. 6:915–922.
Article11. Kot TV, Pettit-Young NA. Lactulose in the management of constipation: a current review. Ann Pharmacother. 1992. 26:1277–1282.
Article12. Wang BX, Wang MG, Jiang MZ, Xu CD, Shao CH, Jia LY, et al. Forlax in the treatment of childhood constipation: a randomized, controlled, multicenter clinical study. Zhongguo Dang Dai Er Ke Za Zhi. 2007. 9:429–432.13. Thomson MA, Jenkins HR, Bisset WM, Heuschkel R, Kalra DS, Green MR, et al. Polyethylene glycol 3350 plus electrolytes for chronic constipation in children: a double blind, placebo controlled, crossover study. Arch Dis Child. 2007. 92:996–1000.
Article14. Candy DC, Edwards D, Geraint M. Treatment of faecal impaction with polyethylene glycol plus electrolytes (PGE +E) followed by a double-blind comparison of PEG+E versus lactulose as maintenance therapy. J Pediatr Gastroenterol Nutr. 2006. 43:65–70.
Article15. Voskuijl W, de Lorijn F, Verwijs W, Hogeman P, Heijmans J, Mäkel W, et al. PEG 3350 (Transipeg) versus lactulose in the treatment of childhood functional constipation: a double blind, randomized, controlled, multicenter trial. Gut. 2004. 53:1590–1594.
Article16. Gremse DA, Hixon J, Crutchfield A. Comparison of polyethylene glycol 3350 and lactulose for treatment of chronic constipation in children. Clin Pediatr (Phila). 2002. 41:225–229.
Article17. Loening-Baucke V, Pashankar DS. A randomized, prospective, comparison study of polyethylene glycol 3350 without electrolytes and milk of magnesia for children with constipation and fecal incontinence. Pediatrics. 2006. 118:528–535.
Article18. Abi-Hanna A, Lake AM. Constipation and encopresis in childhood. Pediatr Rev. 1998. 19:23–30.
Article19. Seo JW. Constipation and encopresis in children. J Korean Med Assoc. 2001. 44:59–68.
Article20. Kim JY. Constipation in children. Korean J Pediatr. 2005. 48:355–362.21. van Ginkel R, Reitsma JB, Büller HA, van Wijk MP, Taminiau JA, Benninga MA. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology. 2003. 125:357–363.
Article22. Sutphen JL, Borowitz SM, Hutchison RL, Cox DJ. Long-term follow-up of medically treated childhood constipation. Clin Pediatr (Phila). 1995. 34:576–580.
Article23. Staiano A, Andreotti MR, Greco L, Basile P, Auricchio S. Long-term follow-up of children with chronic idiopathic constipation. Dig Dis Sci. 1994. 39:561–564.
Article