Korean J Clin Microbiol.
2012 Jun;15(2):70-73. 10.5145/KJCM.2012.15.2.70.
Primary Cutaneous Cryptococcosis in a Patient with Iatrogenic Cushing's Syndrome: A Case Report and Review of the Literature
- Affiliations
-
- 1Department of Laboratory Medicine, Konkuk University School of Medicine and Medical Center, Seoul, Korea. hannasis@kuh.ac.kr
- KMID: 1434176
- DOI: http://doi.org/10.5145/KJCM.2012.15.2.70
Abstract
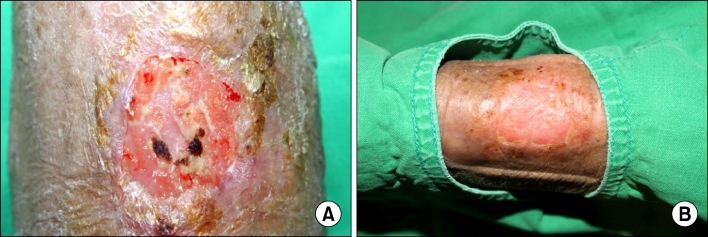
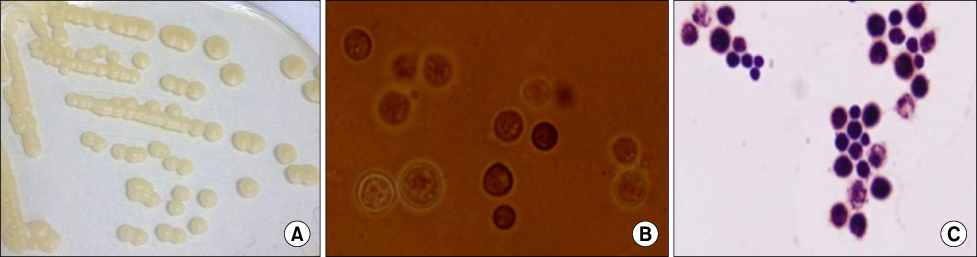
- Cryptococcus neoformans (C. neoformans) is a ubiquitous yeast-like fungus that has been a common opportunistic human pathogen, especially in immunocompromised patients. Although skin lesions due to C. neoformans are found in 10-15% of patients with systemic cryptococcosis, primary cutaneous cryptococcosis without systemic infection is rare and now considered a distinct clinical entity. We report a case of primary cutaneous cryptococcosis in a patient with iatrogenic Cushing's syndrome. A 73-year-old woman presented with pain and discharge from lesions on her left forearm. The patient had been treated with oral corticosteroids for 20 years, and as a result had developed iatrogenic Cushing's syndrome. A skin fragment of the ulcer was cultured, and the encapsulated fungus were isolated and identified as C. neoformans using a Vitek2 system (Vitek2 ID-YST, bio Merieux, France) and API 20C (bioMerieux). Concurrent blood and urine cultures were negative for growth. At first, she was treated with antibiotics due to suspicion of cellulitis. After surgical resection and treatment with systemic and oral fluconazole, her wound was improved with scar. Primary cutaneous cryptococcosis should be considered when skin lesions are not responsive to antibiotics and accurate identification is important for proper treatment.
MeSH Terms
Figure
Cited by 1 articles
-
Cutaneous Cryptococcosis Caused by Intravenous Line in Patient with Rheumatoid Arthritis
Seung Min Ryu, Doo Hyung Yoon, Kyu Jin Chung, Joon Hyuk Choi, Sam-Guk Park
J Korean Soc Surg Hand. 2017;22(3):208-213. doi: 10.12790/jkssh.2017.22.3.208.
Reference
-
1. Ellis DH, Pfeiffer TJ. Ecology, life cycle, and infectious propagule of Cryptococcus neoformans. Lancet. 1990. 336:923–925.2. Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis. 1991. 13:1163–1169.3. Ruiz A, Fromtling RA, Bulmer GS. Distribution of Cryptococcus neoformans in a natural site. Infect Immun. 1981. 31:560–563.4. Kumlin U, Olsen B, Granlund M, Elmqvist LG, Tärnvik A. Cryptococcosis and starling nests. Lancet. 1998. 351:1181.5. Fitzpatrick TB, editor. Dermatology in general medicine. 1993. 4th ed. New York: McGraw-Hill, Health Professions Division.6. Anderson DJ, Schmidt C, Goodman J, Pomeroy C. Cryptococcal disease presenting as cellulitis. Clin Infect Dis. 1992. 14:666–672.7. Neuville S, Dromer F, Morin O, Dupont B, Ronin O, Lortholary O. French Cryptococcosis Study Group. Primary cutaneous cryptococcosis: a distinct clinical entity. Clin Infect Dis. 2003. 36:337–347.8. Probst C, Pongratz G, Capellino S, Szeimies RM, Schölmerich J, Fleck M, et al. Cryptococcosis mimicking cutaneous cellulitis in a patient suffering from rheumatoid arthritis: a case report. BMC Infect Dis. 2010. 10:239.9. Hernandez AD. Cutaneous cryptococcosis. Dermatol Clin. 1989. 7:269–274.10. Powderly WG. Cryptococcal meningitis and AIDS. Clin Infect Dis. 1993. 17:837–842.11. Gatti M, Di Silverio A, Cespa M, Mosca M. Primary unusual cutaneous cryptococcosis in an HIV former drug-abuser patient. Mycoses. 1997. 40:101–102.12. Romano C, Taddeucci P, Donati D, Miracco C, Massai L. Primary cutaneous cryptococcosis due to Cryptococcus neoformans in a woman with non-Hodgkin's lymphoma. Acta Derm Venereol. 2001. 81:220–221.13. Zorman JV, Zupanc TL, Parac Z, Cucek I. Primary cutaneous cryptococcosis in a renal transplant recipient: case report. Mycoses. 2010. 53:535–537.14. Kim YJ, Seo SJ, Ro BI. A case of primary cutaneous cryptococcosis misdiagnosel as skin tuberculosis. Korean J Med Mycol. 2003. 8:16–20.15. Shin DH, Kim KS, Lee JM, Choi JS, Kim KH. Primary cutaneous cryptococosis. Ann Dermatol. 1999. 11:27–29.16. Kim HJ, Min HG, Lee ES. Two cases of cutaneous cryptoccosis mimicking cellulitis. Korean J Med Mycol. 1998. 3:190–194.17. Kang HY, Kim NS, Lee ES. Primary cutaneous cryptococcosis treated with fluconazole. Korean J Dermatol. 2000. 38:838–840.18. Park JH, Ryoo YW, Lee KS. Primary cutaneous cryptococcosis successfully treated with fluconazole. Ann Dermatol. 2000. 12:148–151.19. Pau M, Lallai C, Aste N, Aste N, Atzori L. Primary cutaneous cryptococcosis in an immunocompetent host. Mycoses. 2010. 53:256–258.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cutaneous Cryptococcosis Resembling Pyoderma Gangrenosum
- A Case of Primary Cutaneous Cryptococcosis in a Patient with Iatrogenic Cushing's Syndrome
- Two Cases of Cryptococcosis in Patients with Cushing's Syndrome and Diabetes Mellitus
- Kaposi's Sarcoma in a Patient with Iatrogenic Cushing's Syndrome
- A Case of Primary cutaneous Alternariosis with latrogenic Cushing syndrome