High Prevalence of Ceftazidime-Resistant Klebsiella pneumoniae and Increase of Imipenem-Resistant Pseudomonas aeruginosa and Acinetobacter spp. in Korea: a KONSAR Program in 2004
- Affiliations
-
- 1Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea. whonetkor@yumc.yonsei. ac.kr
- 2Wallace Memorial Baptist Hospital, Busan, Korea.
- 3Wonkwang University Hospital, Iksan, Busan, Korea.
- 4Ajou University Hospital, Suwon, Korea.
- 5Yonsei University Wonju Christian Hospital, Wonju, Korea.
- 6Soonchunhyang Chunan Hospital, Chunan, Korea.
- KMID: 1381244
- DOI: http://doi.org/10.3349/ymj.2006.47.5.634
Abstract
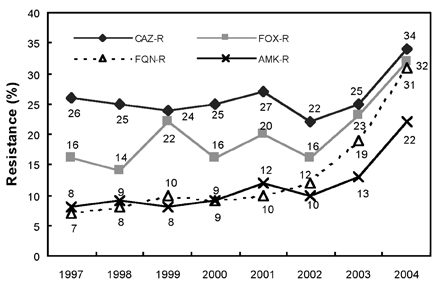
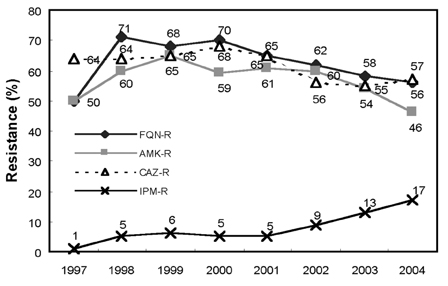
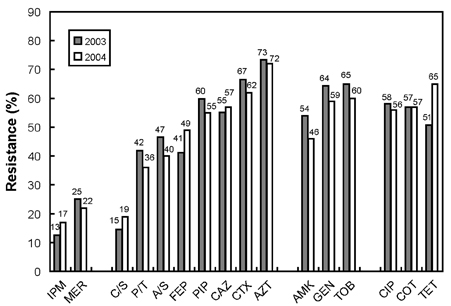
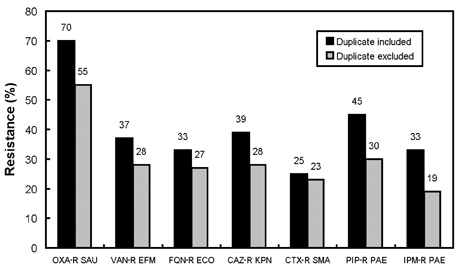
- A nationwide antimicrobial resistance surveillance has been conducted since 1997 in Korea. In this study, susceptibility test data generated in 2004 by KONSAR group hospitals were analyzed and compared to those at a commercial laboratory. In hospitals, the rank orders of organisms in 2004 were identical to those in 2003. The most prevalent species was Staphylococcus aureus (20.2%) in hospitals, but Escherichia coli (29.7%) in the commercial laboratory. The proportions of Enterococcus faecium to all isolates of Enterococcus faecalis plus E. faecium were 47.2% in hospitals and 24.9% in the commercial laboratory. The mean resistance rates of significant antimicrobial-organism combinations in hospitals were: oxacillin-resistant S. aureus (68%), oxacillin-resistant (penicillin- nonsusceptible) Streptococcus pneumoniae (68%), vancomycin-resistant E. faecium (25%), cefotaxime-resistant E. coli (14%), ceftazidime- and cefoxitin-resistant Klebsiella pneumoniae (34% and 32%, respectively), and imipenem-resistant Acinetobacter spp. and Pseudomonas aeruginosa (17% and 24%, respectively). In conclusion, oxacillin-resistant staphylococci, expanded-spectrum cephalosporin-resistant K. pneumoniae, and imipenem-resistant Acinetobacter spp. and P. aeruginosa were prevalent in 2004. Increasing trends were observed for vancomycin-resistant E. faecium, cefoxitin- resistant E. coli and K. pneumoniae, and imipenem-resistant Acinetobacter spp. and P. aeruginosa. Certain antimicrobial- organism combinations were also prevalent among the commercial laboratory-tested strains.
MeSH Terms
-
Pseudomonas aeruginosa/drug effects/isolation & purification
Microbial Sensitivity Tests
Laboratories
Korea
Klebsiella pneumoniae/drug effects/isolation & purification
Imipenem/*pharmacology
Hospitals
Gammaproteobacteria/*drug effects/isolation & purification
Drug Resistance, Multiple, Bacterial
Ceftazidime/*pharmacology
Anti-Bacterial Agents/*pharmacology
Acinetobacter/drug effects/isolation & purification
Figure
Cited by 10 articles
-
Species Distribution and Susceptibility to Azole Antifungals of Candida Bloodstream Isolates from Eight University Hospitals in Korea
Jin-Sol Lee, Jong Hee Shin, Kyungwon Lee, Mi-Na Kim, Bo-Moon Shin, Young Uh, Wee-Gyo Lee, Hye Soo Lee, Chulhun L Chang, Soo Hyun Kim, Myung Geun Shin, Soon Pal Suh, Dong Wook Ryang
Yonsei Med J. 2007;48(5):779-786. doi: 10.3349/ymj.2007.48.5.779.Increase of Ceftazidime- and Fluoroquinolone-Resistant Klebsiella pneumoniae and Imipenem-Resistant Acinetobacter spp. in Korea: Analysis of KONSAR Study Data from 2005 and 2007
Kyungwon Lee, Mi Ae Lee, Chae Hoon Lee, Jongwook Lee, Kyoung Ho Roh, Sunjoo Kim, Jin Ju Kim, Eunmi Koh, Dongeun Yong, Yunsop Chong,
Yonsei Med J. 2010;51(6):901-911. doi: 10.3349/ymj.2010.51.6.901.Clinical and Microbiological Characteristics of Healthcare-Associated Infections in Community-Onset Klebsiella pneumoniae Bacteremia
Jeong-a Lee, Cheol-In Kang, Eun-Jeong Joo, Young Eun Ha, So Yeon Park, Doo Ryeon Chung, Kyong Ran Peck, Nam Yong Lee, Jae-Hoon Song
Infect Chemother. 2012;44(2):56-61. doi: 10.3947/ic.2012.44.2.56.A 2011-2012 Survey of Doctors' Perceptions of Korean Guidelines and Empirical Treatment of Community-Acquired Pneumonia
Hye-In Kim, Shin-Woo Kim, Hyun-Ha Chang, Jong-Myung Lee, Kyong Ran Peck
Infect Chemother. 2013;45(4):394-405. doi: 10.3947/ic.2013.45.4.394.Treatment Guidelines for Community-acquired Pneumonia in Korea: An Evidence-based Approach to Appropriate Antimicrobial Therapy
Jae-Hoon Song, Ki-Suck Jung
J Korean Med Assoc. 2010;53(1):20-42. doi: 10.5124/jkma.2010.53.1.20.The crisis of antimicrobial resistance: current status and future strategies
Jae-Hoon Song, Eun-Jeong Joo
J Korean Med Assoc. 2010;53(11):999-1005. doi: 10.5124/jkma.2010.53.11.999.Therapeutic strategy for the management of multidrug-resistant gram-negative bacterial infections
Cheol-In Kang
J Korean Med Assoc. 2011;54(3):325-331. doi: 10.5124/jkma.2011.54.3.325.Multidrug-resistant Organisms and Healthcare-associated Infections
Mi-Na Kim
Hanyang Med Rev. 2011;31(3):141-152. doi: 10.7599/hmr.2011.31.3.141.Carbapenem Resistance Mechanisms and Molecular Epidemiology of
Acinetobacter spp. from Four Hospitals in Seoul and Gyeonggi Province in 2006
Kyoung Ho Roh, Chang-Ki Kim, Jong Hwa Yum, Dongeun Yong, Seok Hoon Jeong, Chae Seung Lim, Chang Kyu Lee, Yunjung Cho, Kyungwon Lee, Yunsop Chong
Korean J Clin Microbiol. 2010;13(1):27-33. doi: 10.5145/KJCM.2010.13.1.27.Characteristics of Microorganisms Isolated from Blood Cultures at Nine University Hospitals in Korea during 2009
Hee-Jung Kim, Nam Yong Lee, Sunjoo Kim, Jeong Hwan Shin, Mi-Na Kim, Eui-Chong Kim, Sun Hoi Koo, Nam Hee Ryoo, Jae-Seok Kim, Ji-Hyun Cho
Korean J Clin Microbiol. 2011;14(2):48-54. doi: 10.5145/KJCM.2011.14.2.48.
Reference
-
1. Morris AK, Masterton RG. Antibiotic resistance surveillance: action for international studies. J Antimicrob Chemother. 2002. 49:7–10.2. Bax R, Bywater R, Cornaglia G, Goossens H, Hunter P, Isham V, et al. Surveillance of antimicrobial resistance-what, how and whither? Clin Microbiol Infect. 2001. 7:316–325.3. Van Beneden CA, Lexau C, Baughman W, Barnes B, Bennett N, Cassidy PM, et al. Aggregated antibiograms and monitoring of drug-resistant Streptococcus pneumoniae. Emerg Infect Dis. 2003. 9:1089–1095.4. Felmingham D, White AR, Jacobs MR, Appelbaum PC, Poupard J, Miller LA, et al. The Alexander Project: the benefit from a decade of surveillance. J Antimicrob Chemother. 2005. 56:Suppl 2. ii3–ii21.5. Cornaglia G, Hryniewicz W, Jarlier V, Kahlmeter G, Mittermayer H, Stratchounski L, et al. European recommendations for antimicrobial resistance surveillance. Clin Microbiol Infect. 2004. 10:349–383.6. Chong Y, Lee K, Park YJ, Jeon DS, Lee MH, Kim MY, et al. Korean nationwide surveillance of antimicrobial resistance of bacteria in 1997. Yonsei Med J. 1998. 39:569–577.7. Lee K, Park KH, Jeong SH, Lim HS, Shin JH, Yong D, et al. Further increase of vancomycin-resistant Enterococcus faecium, amikacin- and fluoroquinolone-resistant Klebsiella pneumoniae, and imipenem-resistant Acinetobacter spp. in Korea: 2003 KONSAR surveillance. Yonsei Med J. 2006. 47:43–54.8. Lee K, Lee WG, Uh Y, Ha GY, Cho J, Chong Y, et al. VIM- and IMP-type metallo-β-lactamase-producing Pseudomonas spp. and Acinetobacter spp. in Korean hospitals. Emerg Infect Dis. 2003. 9:868–871.9. Lee K, Lee M, Shin JH, Lee MH, Kang SH, Park AJ, et al. Prevalence of plasmid-mediated AmpC β-Lactamases in Escherichia coli and Klebsiella pneumoniae in Korea. Microb Drug Resist. 2006. 12:44–49.10. Gniadkowski M. Evolution and epidemiology of extended-spectrum β-lactamases (ESBLs) and ESBL-producing microorganisms. Clin Microbiol Infect. 2001. 7:597–608.11. Urban C, Segal-Maurer S, Rahal JJ. Considerations in control and treatment of nosocomial infections due to multidrug-resistant Acinetobacter baumannii. Clin Infect Dis. 2003. 36:1268–1274.12. Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-β-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005. 18:306–325.13. National Committee for Clinical Laboratory Standards. Analysis and presentation of cumulative antimicrobial susceptibility test data. Approved guideline M39-A. 2002. Wayne, PA: NCCLS.14. Fridkin SK, Hill HA, Volkova NV, Edwards JR, Lawton RM, Gaynes RP, et al. Temporal changes in prevalence of antimicrobial resistance in 23 U.S. hospitals. Emerg Infect Dis. 2002. 8:697–701.15. Stelling JM, O'Brien TF. Surveillance of antimicrobial resistance: the WHONET program. Clin Infect Dis. 1997. 24:Suppl 1. 157–168.16. Sahm DF, Marsilio MK, Piazza G. Antimicrobial resistance in key bloodstream bacterial isolates: electronic surveillance with the Surveillance Network Database-USA. Clin Infect Dis. 1999. 29:259–263.17. National Committee for Clinical Laboratory Standards. Performance Standards for antimicrobial susceptibility testing: fourteenth informational supplement. 2004. Wayne, PA: NCCLS.18. Yasunaka K, Kono K. Epidemiological study of methicillin-resistant Staphylococcus aureus at Fukuoka University Hospital. Microb Drug Resist. 1999. 5:207–213.19. Tiemersma EW, Bronzwaer SL, Lyytikainen O, Degener JE, Schrijnemakers P, Bruinsma N, et al. Methicillin-resistant Staphylococcus aureus in Europe, 1999-2002. Emerg Infect Dis. 2004. 10:1627–1634.20. Song JH, Jung SI, Ko KS, Kim NY, Son JS, Chang HH, et al. High prevalence of antimicrobial resistance among clinical Streptococcus pneumoniae isolates in Asia (an ANSORP Study). Antimicrob Agents Chemother. 2004. 48:2101–2107.21. Mera RM, Miller LA, Daniels JJ, Weil JG, White AR. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States over a 10-year period: Alexander Project. Diagn Microbiol Infect Dis. 2005. 51:195–200.22. Hunter PA, Reeves DS. The current status of surveillance of resistance to antimicrobial agents: report on a meeting. J Antimicrob Chemother. 2002. 49:17–23.23. Zapantis A, Lacy MK, Horvat RT, Grauer D, Barnes BJ, O'Neal B, et al. Nationwide antibiogram analysis using NCCLS M39-A guidelines. J Clin Microbiol. 2005. 43:2629–2634.24. Treitman AN, Yarnold PR, Warren J, Noskin GA. Emerging incidence of Enterococcus faecium among hospital isolates (1993 to 2002). J Clin Microbiol. 2005. 43:462–463.25. Pai H, Choi EH, Lee HJ, Hong JY, Jacoby GA. Identification of CTX-M-14 extended-spectrum β-lactamase in clinical isolates of Shigella sonnei, Escherichia coli, and Klebsiella pneumoniae in Korea. J Clin Microbiol. 2001. 39:3747–3749.26. Jeong SH, Bae IK, Lee JH, Sohn SG, Kang GH, Jeon GJ, et al. Molecular characterization of extended-spectrum beta-lactamases produced by clinical isolates of Klebsiella pneumoniae and Escherichia coli from a Korean nationwide survey. J Clin Microbiol. 2004. 42:2902–2906.27. Ryoo NH, Kim EC, Hong SG, Park YJ, Lee K, Bae IK, et al. Dissemination of SHV-12 and CTX-M-type extended-spectrum β-lactamases among clinical isolates of Escherichia coli and Klebsiella pneumoniae and emergence of GES-3 in Korea. J Antimicrob Chemother. 2005. 56:698–702.28. Hirakata Y, Matsuda J, Miyazaki Y, Kamihira S, Kawakami S, Miyazawa Y, et al. Regional variation in the prevalence of extended-spectrum β-lactamase-producing clinical isolates in the Asia-Pacific region (SENTRY 1998-2002). Diagn Microbiol Infect Dis. 2005. 52:323–329.29. Goossens H, Grabein B. Prevalence and antimicrobial susceptibility data for extended-spectrum (-lactamase- and AmpC-producing Enterobacteriaceae from the MYSTIC Program in Europe and the United States (1997-2004). Diagn Microbiol Infect Dis. 2005. 53:257–264.30. Song W, Kim JS, Kim MN, Kim EC, Park YJ, Yong D, et al. Occurrence and genotypic distribution of plasmid-mediated AmpC β-lactamase-producing Eshcherichia coli and Klebsiella pneumoniae in Korea. Korean J Lab Med. 2002. 22:410–416.31. Yong D, Lim Y, Song W, Choi YS, Park DY, Lee H, et al. Plasmid-mediated, inducible AmpC β-lactamase (DHA-1)-producing Enterobacteriaceae at a Korean hospital: wide dissemination in Klebsiella pneumoniae and Klebsiella oxytoca and emergence in Proteus mirabilis. Diagn Microbiol Infect Dis. 2005. 53:65–70.32. Philippon A, Arlet G, Jacoby GA. Plasmid-determined AmpC-type beta-lactamases. Antimicrob Agents Chemother. 2002. 46:1–11.33. Bidet P, Burghoffer B, Gautier V, Brahimi N, Mariani-Kurkdjian P, El-Ghoneimi A, et al. In vivo transfer of plasmid-encoded ACC-1 AmpC from Klebsiella pneumoniae to Escherichia coli in an infant and selection of impermeability to imipenem in K. pneumoniae. Antimicrob Agents Chemother. 2005. 49:3562–3565.34. Jeong SH, Lee K, Chong Y, Yum JH, Lee SH, Choi HJ, et al. Characterization of a new integron containing VIM-2, a metallo-β-lactamase gene cassette, in a clinical isolate of Enterobacter cloacae. J Antimicrob Chemother. 2003. 51:397–400.35. Lee HK, Park YJ, Kim JY, Chang E, Cho SG, Chae HS, et al. Prevalence of decreased susceptibility to carbapenems among Serratia marcescens, Enterobacter cloacae, and Citrobacter freundii and investigation of carbapenemases. Diagn Microbiol Infect Dis. 2005. 52:331–336.36. Higgins PG, Wisplinghoff H, Stefanik D, Seifert H. In vitro activities of the beta-lactamase inhibitors clavulanic acid, sulbactam, and tazobactam alone or in combination with beta-lactams against epidemiologically characterized multidrug-resistant Acinetobacter baumannii strains. Antimicrob Agents Chemother. 2004. 48:1586–1592.37. Smolyakov R, Borer A, Riesenberg K, Schlaeffer F, Alkan M, Porath A, et al. Nosocomial multi-drug resistant Acinetobacter baumannii bloodstream infection: risk factors and outcome with ampicillin-sulbactam treatment. J Hosp Infect. 2003. 54:32–38.38. Livermore DM, Woodford N. Carbapenemases: a problem in waiting? Curr Opin Microbiol. 2000. 3:489–495.39. Kim IS, Oh WI, Song JH, Lee NY. Screening and identification of metallo-β-lactamase gene in clinical isolates of imipenem-resistant Pseudomonas aeruginosa. Korean J Lab Med. 2004. 24:177–182.40. Kim IS, Lee NY, Ki CS, Oh WS, Peck KR, Song JH. Increasing prevalence of imipenem-resistant Pseudomonas aeruginosa and molecular typing of metallo-β-lactamase producers in a Korean hospital. Microb Drug Resist. 2005. 11:355–359.41. Shin KS, Han K, Lee J, Hong SB, Son BS, Youn SJ, et al. Imipenem-resistant Achromobacter xylosoxidans carrying blaVIM-2-containing class 1 integron. Diagn Microbiol Infect Dis. 2005. 53:215–220.42. Jeon BC, Jeong SH, Bae IK, Kwon SB, Lee K, Young D, et al. Investigation of a nosocomial outbreak of imipenem-resistant Acinetobacter baumannii producing the OXA-23 β-lactamase in Korea. J Clin Microbiol. 2005. 43:2241–2245.43. Reis AO, Luz DAM, Tognim MCB, Sader HS, Gales AC. Polymyxin-resistant Acinetobacter spp. isolates; what is next? Emerg Infect Dis. 2003. 9:1025–1027.44. Hooper DC. The future of the quinolones. APUA Newsletter. 2001. 19:1–5.45. Park MS, Kang YH, Lee SJ, Song CY, Lee BK. Characteristics of epidemic multidrugresistant Salmonella enterica serovar Typhimurium DT104 strains first isolated in Korea. Korean J Infect Dis. 2002. 34:1–8.46. Hasegawa K, Chiba N, Kobayashi R, Murayama Y, Iwata S, Sunakawa K, et al. Rapidly increasing prevalence of β-lactamase-nonproducing, ampicillin-resistant Haemophilus influenzae type b in patients with meningitis. Antimicrob Agents Chemother. 2004. 48:1509–1514.47. Lauderdale TL, McDonald LC, Shiau YR, Chen PC, Wang HY, Lai JF, et al. The status of antimicrobial resistance in Taiwan among gram-negative pathogens: the Taiwan surveillance of antimicrobial resistance (TSAR) program, 2000. Diagn Microbiol Infect Dis. 2004. 48:211–219.48. Diekema DJ, BootsMiller BJ, Vaughn TE, Woolson RF, Yankey JW, Ernst EJ, et al. Antimicrobial resistance trends and outbreak frequency in United States hospitals. Clin Infect Dis. 2004. 38:78–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Increase of Ceftazidime- and Fluoroquinolone-Resistant Klebsiella pneumoniae and Imipenem-Resistant Acinetobacter spp. in Korea: Analysis of KONSAR Study Data from 2005 and 2007
- Increase in the Prevalence of Carbapenem-Resistant Acinetobacter Isolates and Ampicillin-Resistant Non-Typhoidal Salmonella Species in Korea: A KONSAR Study Conducted in 2011
- Further Increases in Carbapenem-, Amikacin-, and Fluoroquinolone-Resistant Isolates of Acinetobacter spp. and P. aeruginosa in Korea: KONSAR Study 2009
- Trend of Bacterial Resistance for the Past 50 Years in Korea and Future Perspectives - Gram-negative Bacteria
- Increasing Prevalence of Vancomycin-Resistant Enterococci, and Cefoxitin-, Imipenem- and Fluoroquinolone-Resistant Gram-Negative Bacilli: A KONSAR Study in 2002