Korean J Radiol.
2012 Jun;13(3):332-341. 10.3348/kjr.2012.13.3.332.
Practical Application of Iterative Decomposition of Water and Fat with Echo Asymmetry and Least-Squares Estimation (IDEAL) Imaging in Minimizing Metallic Artifacts
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Bucheon Hospital, Bucheon 420-767, Korea. mj4907@schmc.ac.kr
- KMID: 1372853
- DOI: http://doi.org/10.3348/kjr.2012.13.3.332
Abstract
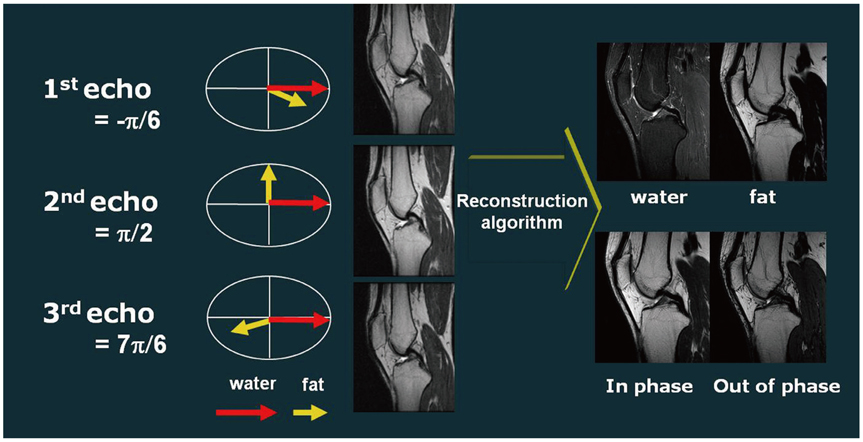
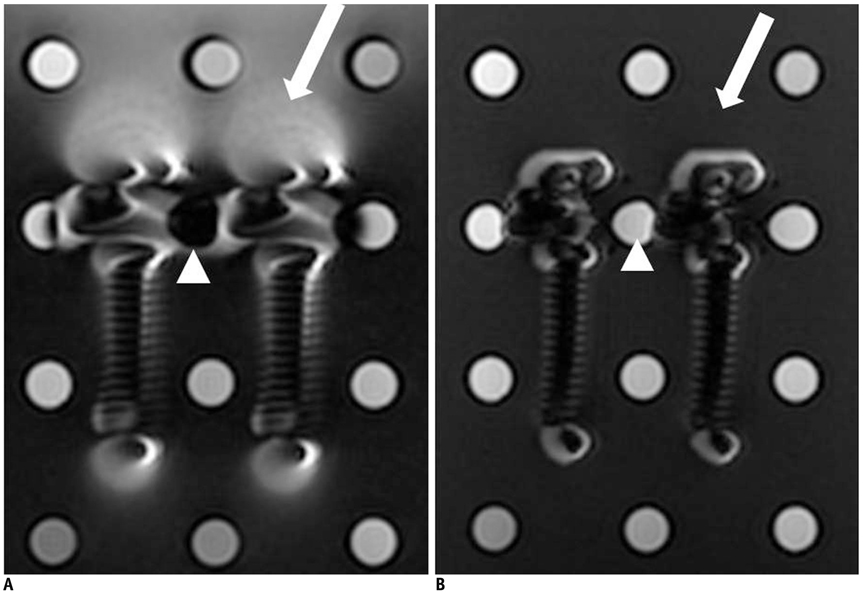
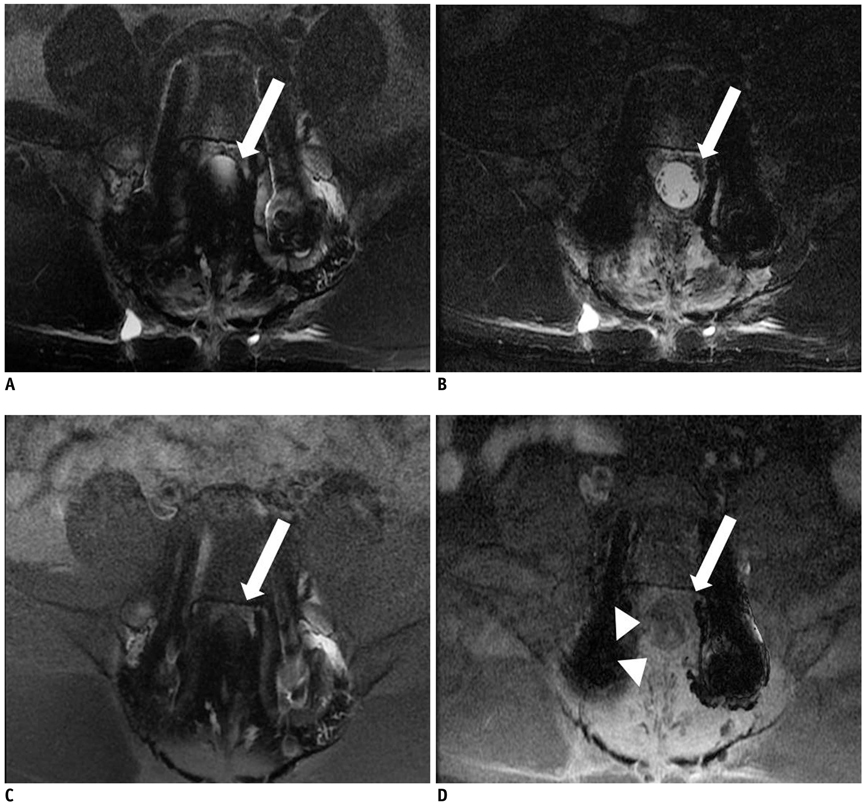
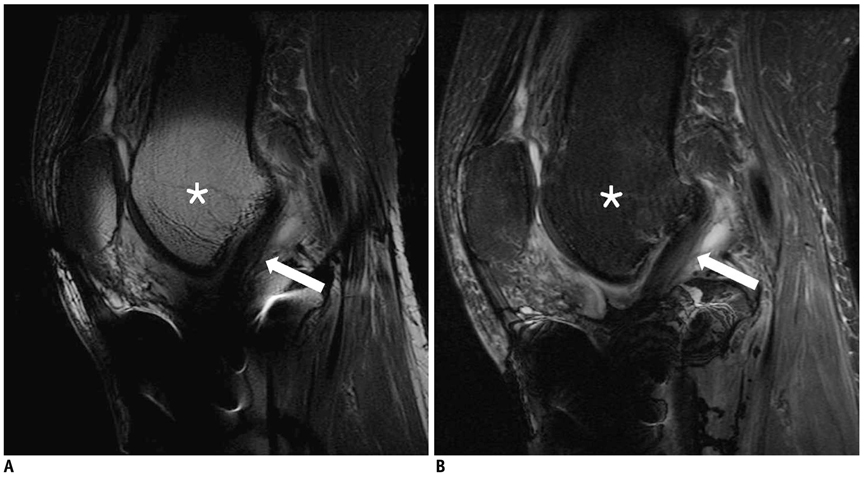
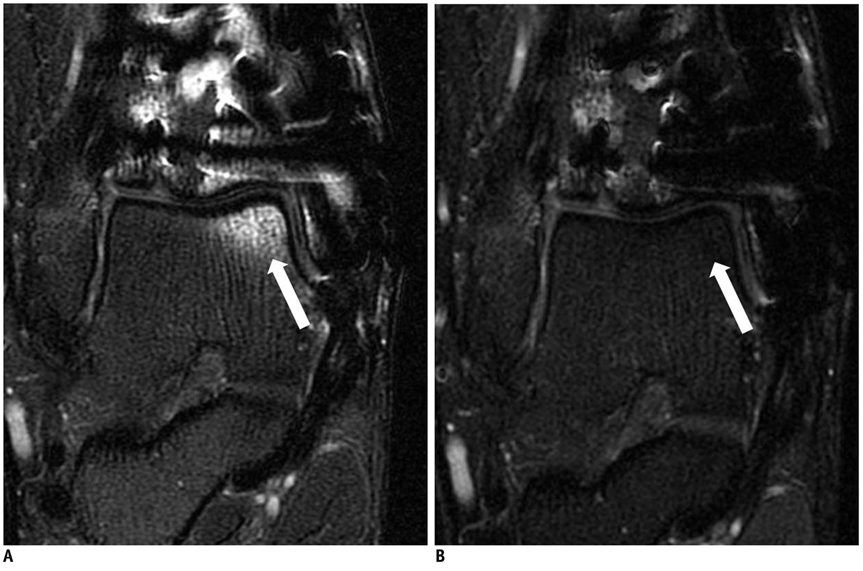
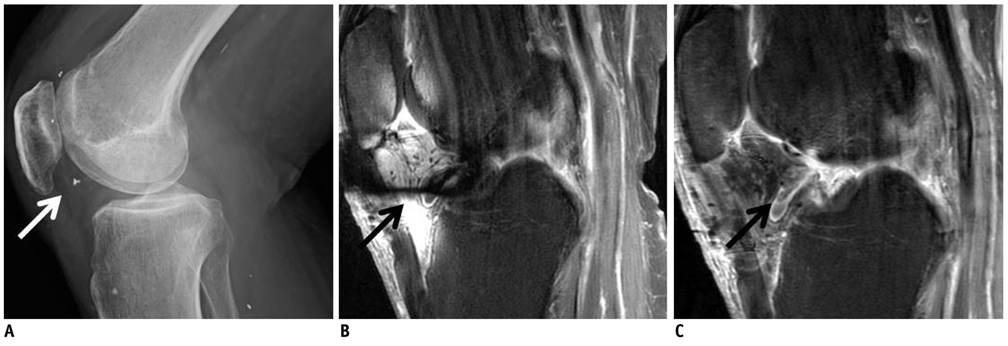
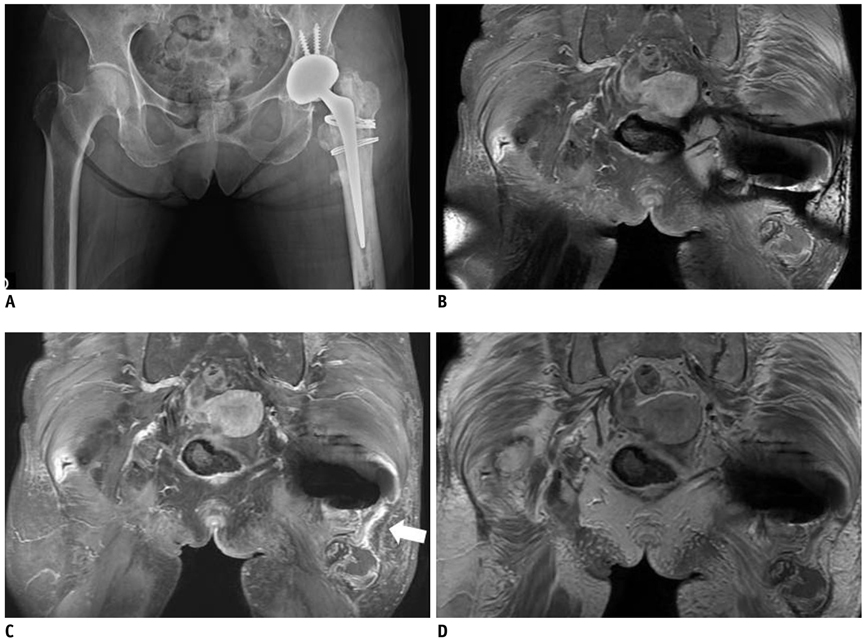
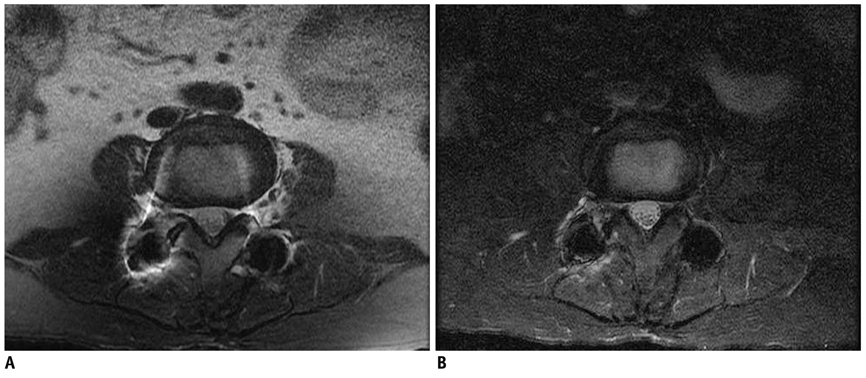
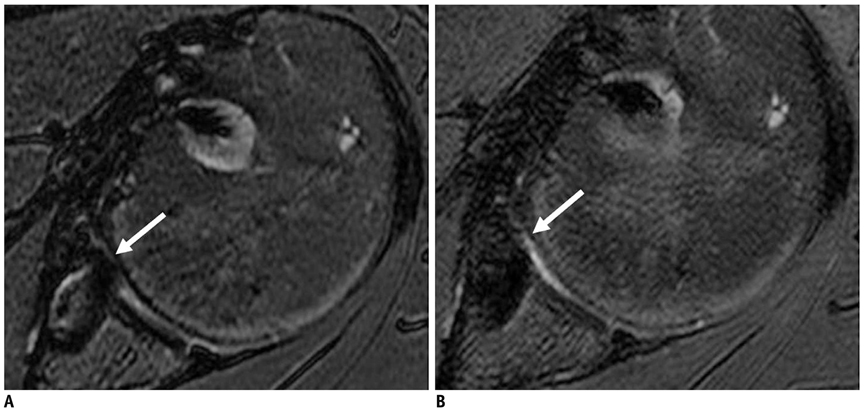
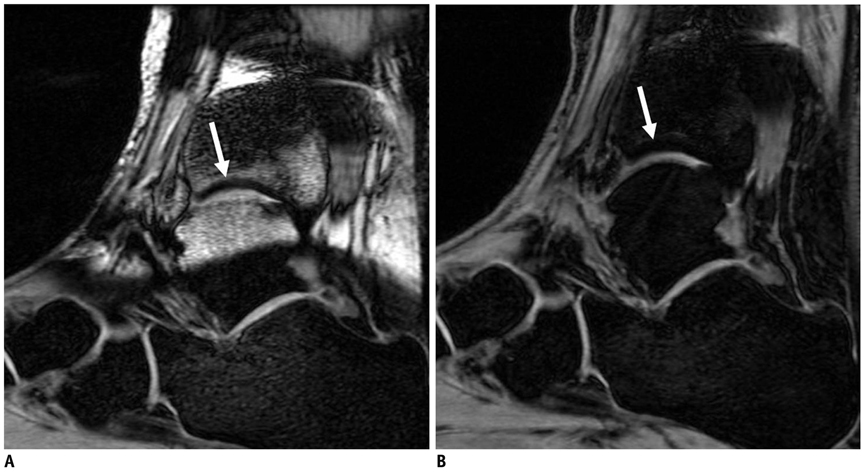
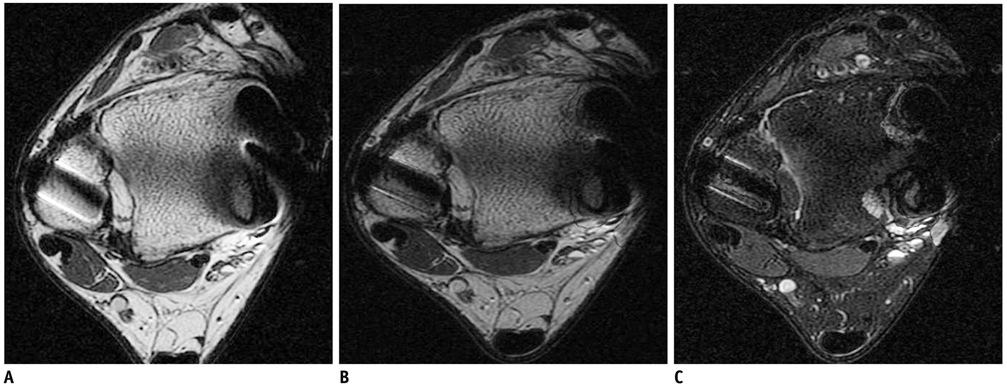
- Iterative decomposition of water and fat with echo asymmetry and the least-squares estimation (IDEAL) is a recently developed method for robust separation of fat and water with very high signal-to-noise-ratio (SNR) efficiency. In contrast to conventional fat-saturation methods, IDEAL is insensitive to magnetic field (B0 and B1) inhomogeneity. The aim of this study was to illustrate the practical application of the IDEAL technique in reducing metallic artifacts in postoperative patients with metallic hardware. The IDEAL technique can help musculoskeletal radiologists make an accurate diagnosis particularly in musculoskeletal imaging by reducing metallic artifacts, enabling the use of contrast enhancement, improving SNR performance, and providing various modes of MR images with one scan parameter.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee MJ, Kim S, Lee SA, Song HT, Huh YM, Kim DH, et al. Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multi-detector CT. Radiographics. 2007. 27:791–803.2. Murakami M, Mori H, Kunimatsu A, Abe O, Chikuda H, Ono T, et al. Postsurgical spinal magnetic resonance imaging with iterative decomposition of water and fat with echo asymmetry and least-squares estimation. J Comput Assist Tomogr. 2011. 35:16–20.3. Harris CA, White LM. Metal artifact reduction in musculoskeletal magnetic resonance imaging. Orthop Clin North Am. 2006. 37:349–359. vi4. Cha JG, Jin W, Lee MH, Kim DH, Park JS, Shin WH, et al. Reducing metallic artifacts in postoperative spinal imaging: usefulness of IDEAL contrast-enhanced T1- and T2-weighted MR imaging--phantom and clinical studies. Radiology. 2011. 259:885–893.5. Gerdes CM, Kijowski R, Reeder SB. IDEAL imaging of the musculoskeletal system: robust water fat separation for uniform fat suppression, marrow evaluation, and cartilage imaging. AJR Am J Roentgenol. 2007. 189:W284–W291.6. Zhuo J, Gullapalli RP. AAPM/RSNA physics tutorial for residents: MR artifacts, safety, and quality control. Radiographics. 2006. 26:275–297.7. Berquist TH. Imaging of the postoperative spine. Radiol Clin North Am. 2006. 44:407–418.8. Vandevenne JE, Vanhoenacker FM, Parizel PM, Butts Pauly K, Lang RK. Reduction of metal artefacts in musculoskeletal MR imaging. JBR-BTR. 2007. 90:345–349.9. Bydder GM, Steiner RE, Blumgart LH, Khenia S, Young IR. MR imaging of the liver using short TI inversion recovery sequences. J Comput Assist Tomogr. 1985. 9:1084–1089.10. Fuller S, Reeder S, Shimakawa A, Yu H, Johnson J, Beaulieu C, et al. Iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL) fast spin-echo imaging of the ankle: initial clinical experience. AJR Am J Roentgenol. 2006. 187:1442–1447.11. Reeder SB, Pineda AR, Wen Z, Shimakawa A, Yu H, Brittain JH, et al. Iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL): application with fast spin-echo imaging. Magn Reson Med. 2005. 54:636–644.12. Yu H, Reeder SB, Shimakawa A, Brittain JH, Pelc NJ. Field map estimation with a region growing scheme for iterative 3-point water-fat decomposition. Magn Reson Med. 2005. 54:1032–1039.13. Reeder SB, Wen Z, Yu H, Pineda AR, Gold GE, Markl M, et al. Multicoil Dixon chemical species separation with an iterative least-squares estimation method. Magn Reson Med. 2004. 51:35–45.14. Crema MD, Roemer FW, Marra MD, Burstein D, Gold GE, Eckstein F, et al. Articular cartilage in the knee: current MR imaging techniques and applications in clinical practice and research. Radiographics. 2011. 31:37–61.15. Leffler S, Disler DG. MR imaging of tendon, ligament, and osseous abnormalities of the ankle and hindfoot. Radiol Clin North Am. 2002. 40:1147–1170.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improvement of Fat Suppression and Artifact Reduction Using IDEAL Technique in Head and Neck MRI at 3T
- MR Imaging of the Spine at 3.0T with T2-Weighted IDEAL Fast Recovery Fast Spin-Echo Technique
- Parameters Affecting India Ink Artifacts on Opposed-Phase MR Images
- MR imaging of metallic artifacts
- In Vivo Assessment of Neurodegeneration in Type C Niemann-Pick Disease by IDEAL-IQ