J Breast Cancer.
2011 Feb;14(Suppl 1):S57-S63. 10.4048/jbc.2011.14.S.S57.
Incidence of Brain Metastasis and Related Subtypes in Patients with Breast Cancer Receiving Adjuvant Radiation Therapy after Surgery
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. doho.choi@samsung.com
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1340915
- DOI: http://doi.org/10.4048/jbc.2011.14.S.S57
Abstract
- PURPOSE
To assess the incidence of brain metastasis in patients with breast cancer receiving surgery and adjuvant radiotherapy (RT) and to evaluate subtypes associated with brain metastasis.
METHODS
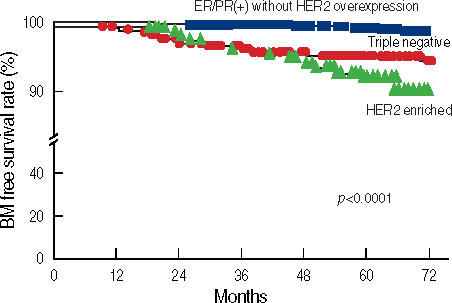
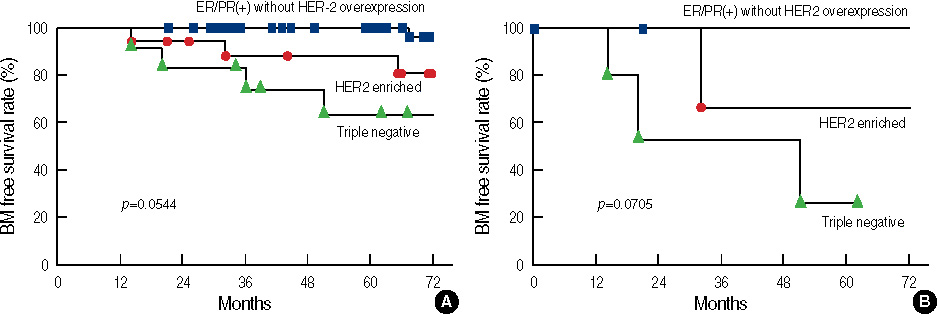
We retrospectively reviewed the medical records of 1,000 patients with breast cancer who were treated with surgery and adjuvant RT for a cure between January 2001 and July 2005 at Samsung Medical Center. Seventy-one patients received neoadjuvant chemotherapy before surgery. The pathological stage was I in 430 patients, II in 327, and III in 243. We divided the patients into three subtypes according to immunohistochemistry: triple negative (TN, 245 patients), human epidermal growth factor 2 (HER2) enriched (HE, 166 patients) and positive estrogen receptor or progesterone receptor without HER2 overexpression (EP, 589 patients). The median follow up time was 72 months after surgery.
RESULTS
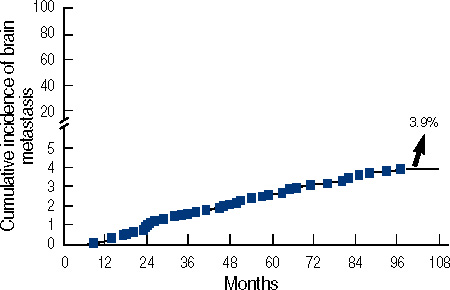
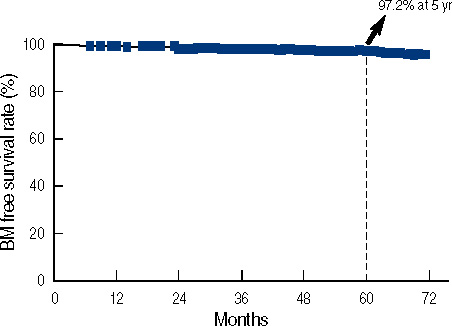
Locoregional failure-free survival rate and distant metastasis-free survival rate at 5 years were 92.8% and 86.1%, respectively. The disease free survival rate and overall survival rate at 5 years were 84.6% and 94.7%, respectively. Thirty-nine patients had brain metastasis, and the brain metastasis-free survival rate at 5 years was 97.2%. A univariate analysis showed that younger age, neoadjuvant chemotherapy, modified radical mastectomy, advanced pathological stage and the TN and HE subtypes were significant risk factors for brain metastasis. A multivariate analysis revealed that age, neoadjuvant chemotherapy, pathological stage and the TN and HE subtypes were statistically significant factors for brain metastasis.
CONCLUSION
The cumulative incidence of brain metastasis was 3.9% after curative treatment. If patients have a clinically suspicious symptoms suggesting brain metastasis, clinicians should be aware that an early brain imaging work up and management are necessary. Because patients with the TN or HE subtypes accompanied by younger age and advanced pathological stage have increased brain metastasis (>10%), annual regular imaging follow-up may be recommended for these high risk patients.
Figure
Reference
-
1. Zimm S, Wampler GL, Stablein D, Hazra T, Young HF. Intracerebral metastases in solid-tumor patients: natural history and results of treatment. Cancer. 1981. 48:384–394.
Article2. Lin NU, Bellon JR, Winer EP. CNS metastases in breast cancer. J Clin Oncol. 2004. 22:3608–3617.
Article3. Tsukada Y, Fouad A, Pickren JW, Lane WW. Central nervous system metastasis from breast carcinoma. Autopsy study. Cancer. 1983. 52:2349–2354.
Article4. Lai R, Dang CT, Malkin MG, Abrey LE. The risk of central nervous system metastases after trastuzumab therapy in patients with breast carcinoma. Cancer. 2004. 101:810–816.
Article5. Lower EE, Drosick DR, Blau R, Brennan L, Danneman W, Hawley DK. Increased rate of brain metastasis with trastuzumab therapy not associated with impaired survival. Clin Breast Cancer. 2003. 4:114–119.
Article6. Clayton AJ, Danson S, Jolly S, Ryder WD, Burt PA, Stewart AL, et al. Incidence of cerebral metastases in patients treated with trastuzumab for metastatic breast cancer. Br J Cancer. 2004. 91:639–643.
Article7. Ono M, Ando M, Yunokawa M, Nakano E, Yonemori K, Matsumoto K, et al. Brain metastases in patients who receive trastuzumab-containing chemotehrapy for HER2-overexpressing metastatic breast cancer. Int J Clin Oncol. 2009. 14:48–52.
Article8. Perou CM, Sorlie T, Eisen MB, Van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000. 406:747–752.
Article9. Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001. 98:10869–10874.
Article10. Sørlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003. 100:8418–8423.
Article11. Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005. 11:5678–5685.
Article12. Smid M, Wang Y, Klijn JG, Sieuwerts AM, Zhang Y, Atkins D, et al. Genes associated with breast cancer metastatic to bone. J Clin Oncol. 2006. 24:2261–2267.
Article13. Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordon-Cardo C, et al. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. 2003. 3:537–549.
Article14. Deckers M, van Dinther M, Buijs J, Que I, Lowik C, Van der Pluijm G, et al. The tumor suppressor Smad4 is required for transforming growth factor beta-induced epithelial to mesenchymal transition and bone metastasis of breast cancer cells. Cancer Res. 2006. 66:2202–2209.
Article15. Minn AJ, Gupta GP, Siegel PM, Bos PD, Shu W, Giri DD, et al. Genes that mediate breast cancer metastasis to lung. Nature. 2005. 436:518–524.
Article16. Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JG, et al. Subtypes of breast cancer show preferential site of relapse. Cancer Res. 2008. 68:3108–3114.
Article17. Slimane K, Andre F, Delaloge S, Dunant A, Perez A, Grenier J, et al. Risk factors for brain relapse in patients with metastatic breast cancer. Ann Oncol. 2004. 15:1640–1644.
Article18. Kaal EC, Vecht CJ. CNS complications of breast cancer: current and emerging treatment options. CNS Drugs. 2007. 21:559–579.19. Graesslin O, Abdulkarim BS, Coutant C, Huguet F, Gabos Z, Hsu L, et al. Nomogram to predict subsequent brain metastasis in patients with metastatic breast cancer. J Clin Oncol. 2010. 28:2032–2037.
Article20. Gonzalez-Angulo AM, Cristofanilli M, Strom EA, Buzdar AU, Kau SW, Broglio KR, et al. Central nervous system metastases in patients with high-risk breast carcinoma after multimodality treatment. Cancer. 2004. 101:1760–1766.
Article21. American Joint Committee on Cancer (AJCC). AJCC Cancer Staging Manual. 2010. 7th ed. New York: Springer.22. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005. 365:1687–1717.23. Lee SS, Ahn JH, Kim MK, Sym SJ, Gong G, Ahn SD, et al. Brain metastases in breast cancer: prognostic factors and management. Breast Cancer Res Treat. 2008. 111:523–530.
Article24. Korean Breast Cancer Society. 2006-2008 Breast Cancer Facts & Figures. 2008. Seoul: Korean Breast Cancer Society;5–12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effective Treatment of Solitary Pituitary Metastasis with Panhypopituitarism in HER2-Positive Breast Cancer by Lapatinib
- Preliminary Result of Concurrent Chemotherapy and Rediotherapy in Stage I and II Breast Cancer Patients Treated with Breast Conservation Surgery
- Incidence and Risk Factors for Leptomeningeal Carcinomatosis in Breast Cancer Patients with Parenchymal Brain Metastases
- Changes of Symptom Distress and Quality of Life in Breast Cancer Patients Receiving Adjuvant Therapy
- Preliminary Result of Concurrent Chemotherapy and Radiotherapy in Stage I and II Breast Cancer Patients Treated with Breast Conservation Surgery