Yonsei Med J.
2011 Nov;52(6):1022-1024. 10.3349/ymj.2011.52.6.1022.
Successful Catheter Ablation of Focal Automatic Left Ventricular Tachycardia Presented with Tachycardia-Mediated Cardiomyopathy
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Kwandong University College of Medicine, Goyang, Korea.
- 2Cardiology Division, Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea. jinbbai@khu.ac.kr
- 3Cardiology Division, Yonsei Cardiovascular Center and Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1058825
- DOI: http://doi.org/10.3349/ymj.2011.52.6.1022
Abstract
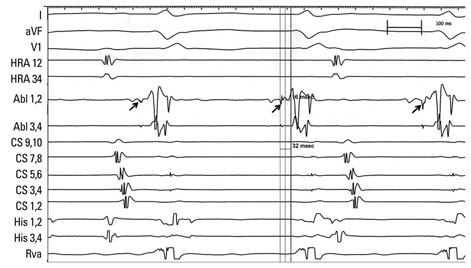
- Non-reentrant focal tachycardias occur spontaneously, facilitated by catecholamine infusion, but they cannot be initiated or terminated with programmed stimulation. These tachycardias exhibit early activation before the QRS, however, do not typically show the mid-diastolic potential that is crucial for reentrant tachycardia maintenance. Electrophysiological studies are useful for distinguishing focal from macro-reentrant ventricular tachycardia. We report herein a case of patient without a history of structural heart disease who presented with a focal Purkinje ventricular tachycardia and heart failure. The focal Purkinje ventricular tachycardia was eliminated by radiofrequency catheter ablation. All of the patien's symptoms were improved after ablation.
MeSH Terms
Figure
Reference
-
1. Nogami A. Idiopathic left ventricular tachycardia: assessment and treatment. Card Electrophysiol Rev. 2002. 6:448–457.2. Latif S, Dixit S, Callans DJ. Ventricular arrhythmias in normal hearts. Cardiol Clin. 2008. 26:367–380. vi
Article3. Markowitz SM, Lerman BB. Mechanisms of focal ventricular tachycardia in humans. Heart Rhythm. 2009. 6:S81–S85.
Article4. Zeppenfeld K, Blom NA, Bootsma M, Schalij MJ. Incessant ventricular tachycardia in fulminant lymphocytic myocarditis: Evidence for origin in the Purkinje system and successful treatment with ablation. Heart Rhythm. 2007. 4:88–91.5. Castro-Rodriguez J, Verbeet T, Morissens M, Lomas O, Tran-Ngoc E, Malekzadeh-Milani S, et al. Complicated Forms of Tachycardia-Mediated Cardiomyopathy Associated with Idiopathic Left Ventricular Tachycardia. Pacing Clin Electrophysiol. 2010.
Article6. Seiler J, Lee JC, Roberts-Thomson KC, Stevenson WG. Intracardiac echocardiography guided catheter ablation of incessant ventricular tachycardia from the posterior papillary muscle causing tachycardia--mediated cardiomyopathy. Heart Rhythm. 2009. 6:389–392.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Treatment of Tachycardia-induced Cardiomyopathy with Radiofrequency Catheter Ablation
- Catheter Ablation of Ventricular Tachycardia/Fibrillation in a Patient with Right Ventricular Amyloidosis with Initial Manifestations Mimicking Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy
- Preexcitation Syndrome with a Mahaim-type Accessory Pathway
- Intramural Reentrant Ventricular Tachycardia in a Patient with Severe Hypertensive Left Ventricular Hypertrophy
- Catheter Ablation of Ventricular Tachycardia in Patients with Post-Infarction Cardiomyopathy