Yonsei Med J.
2008 Jun;49(3):400-404. 10.3349/ymj.2008.49.3.400.
Long-Term Outcomes of Acute Ischemic Stroke in Patients Aged 80 Years and Older
- Affiliations
-
- 1Department of Neurology, 1Hangang Sacred Heart Hospital, Seoul, Korea. dowonc@naver.com
- 2Hallym University Sacred Heart Hospital, Anyang, Korea.
- 3Hallym University College of Medicine, Chuncheon, Korea.
- KMID: 724254
- DOI: http://doi.org/10.3349/ymj.2008.49.3.400
Abstract
- PURPOSE
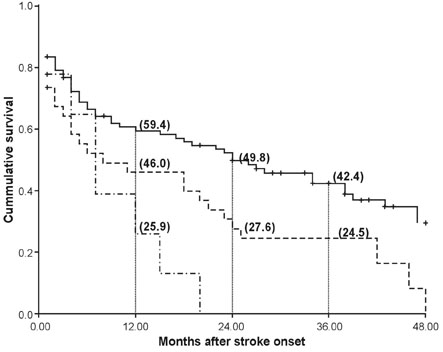
Short life expectancy influences decision-making when treating very old patients with acute ischemic stroke (AIS). We investigated mortality and survival duration in very old AIS patients (> or =80 years) who received hospital care. PATIENTS AND METHODS: Mortality data were obtained from medical records, structured telephone inquiries, death certificates from the Korean National Statistical Office, and social security data 5+/-1.9 years after stroke onset. Age, gender, vascular risk factors, and functional outcomes from modified Rankin scales (MRS) at discharge were analyzed as predictors of mortality. RESULTS: Among 134 patients, 92 (68.7%) died. On Kaplan- Meier analysis, duration of survival of patients aged 80-84 years was longer than those aged 85-89 or 90-94 (24+/-6.4, 8+/-7.3, 7+/-2.0 months, respectively, p=0.002). Duration of survival of patients discharged in a state of MRS 0-1 was longer than the remaining groups at 47+/-4.8 months (p<0.001). In Cox proportional hazard analysis, age and MRS at discharge were independent predictors of mortality. CONCLUSION: Long-term outcomes of very old patients with AIS are not uniformly grave, therefore predictors of mortality and estimated duration of survival should be considered during decision- making for treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Di Carlo A, Lamassa M, Pracucci G, Basile AM, Trefoloni G, Vanni P, et al. Stroke in the very old: clinical presentation and determinants of 3-month functional outcome: A European perspective. European BIOMED Study of Stroke Care Group. Stroke. 1999. 30:2313–2319.2. Sharma JC, Fletcher S, Vassallo M. Strokes in the elderly-higher acute and 3-month mortality-an explanation. Cerebrovasc Dis. 1999. 9:2–9.
Article3. Olindo S, Cabre P, Deschamps R, Chatot-Henry C, René-Corail P, Fournerie P, et al. Acute stroke in the very elderly: epidemiological features, stroke subtypes, management, and outcome in Martinique, French West Indies. Stroke. 2003. 34:1593–1597.4. Altieri M. SPASE-1: a multicenter observational study on pharmacological treatment of acute stroke in the elderly. The Italian Study of Pharmacological Treatment of Acute Stroke in the Elderly group. Neurol Sci. 2002. 23:23–28.
Article5. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991. 325:445–453.6. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blinded placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998. 352:1245–1251.
Article7. Miller MT, Comerota AJ, Tzilinis A, Daoud Y, Hammerling J. Carotid endarterectomy in octogenarians: does increased age indicate "high risk?". J Vasc Surg. 2005. 41:231–237.
Article8. Chen CI, Iguchi Y, Grotta JC, Garami Z, Uchino K, Shaltoni H, et al. Intravenous TPA for very old stroke patients. Eur Neurol. 2005. 54:140–144.
Article9. Engelter ST, Bonati LH, Lyrer PA. Intravenous thrombolysis in stroke patients of > or = 80 versus < 80 years of age-a systematic review across cohort studies. Age Ageing. 2006. 35:572–580.
Article10. Arboix A, García-Eroles L, Massons J, Oliveres M, Targa C. Acute stroke in very old people: clinical features and predictors of in-hospital mortality. J Am Geriatr Soc. 2000. 48:36–41.
Article11. Kammersgaard LP, Jørgensen HS, Reith J, Nakayama H, Pedersen PM, Olsen TS. Short- and long-term prognosis for very old stroke patients. The Copenhagen Stroke Study. Age Ageing. 2004. 33:149–154.
Article12. Lee BC, Hwang SH, Jung S, Yu KH, Lee JH, Cho SJ, et al. The Hallym Stroke Registry: a web-based stroke data bank with an analysis of 1,654 consecutive patients with acute stroke. Eur Neurol. 2005. 54:81–87.
Article13. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.
Article14. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1998. 19:604–607.
Article15. Ovbiagele B, Hills NK, Saver JL, Johnston SC. Secondary-prevention drug prescription in the very elderly after ischemic stroke or TIA. Neurology. 2006. 66:313–318.
Article16. Dennis MS. Stroke unit versus and neurology ward-a short commentary. J Neurol. 2003. 250:1370–1371.17. Hénon H, Durieu I, Lebert F, Pasquier F, Leys D. Influence of prestroke dementia on early and delayed mortality in stroke patients. J Neurol. 2003. 250:10–16.
Article18. Minn YK, Cho SJ, Lee JH, Kim SY, Kim CH, Kwon KH, et al. Significance of silent infarcts in acute ischemic stroke patients aged 80 years and older. Cerebrovasc Dis. 2005. 20:92–95.
Article19. de Jong G, van Raak L, Kessels F, Lodder J. Stroke subtype and mortality: a follow-up study in 998 patients with a first cerebral infarct. J Clin Epidemiol. 2003. 56:262–268.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Inhibition of LPA5 Activity Provides Long-Term Neuroprotection in Mice with Brain Ischemic Stroke
- Epidemiology and Functional Outcome of Acute Stroke Patients in Korea Using Nationwide data
- Long-Term Mortality According to the Characteristics of Early Neurological Deterioration in Ischemic Stroke Patients
- Significances and Outcomes of Mechanical Thrombectomy for Acute Infarction in Very Elderly Patients: A Single Center Experience