J Korean Neurosurg Soc.
2025 Mar;68(2):159-176. 10.3340/jkns.2024.0118.
Epidemiology and Functional Outcome of Acute Stroke Patients in Korea Using Nationwide data
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, College of Medicine, Soonchunhyang University, Cheonan, Korea
- 2Department of Neurosurgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Neurosurgery, Bundang CHA Medical Center, CHA University, Seongnam, Korea
- 4Department of Neurosurgery, Soonchunhyang University Seoul Hospital, College of Medicine, Soonchunhyang University, Seoul, Korea
- 5Department of Neurosurgery, Inje University Haeundae Paik Hospital, Busan, Korea
- 6Department of Neurosurgery, Hallym University College of Medicine, Chuncheon, Korea
- 7Health Insurance Review & Assessment Service (HIRA), Wonju, Korea
- 8Healthcare Review and Assessment Committee (HCRAC), Seoul, Korea
- 9Cardio-Cerebrovascular Disease Assessment Division, Quality Assessment Administration Department, Healthcare Review and Assessment Committee (HCRAC), Seoul, Korea
- 10Quality Assessment Management Division, Quality Assessment Department , Healthcare Review and Assessment Committee (HCRAC), Seoul, Korea
- KMID: 2565274
- DOI: http://doi.org/10.3340/jkns.2024.0118
Abstract
Objective
: Korea’s healthcare system and policy promotes early, actively stroke treatment to improve prognosis. This study represents stroke epidemiology and outcomes in Korea.
Methods
: This study investigated data from the Acute Stroke Assessment Registry. The registry collects data from over 220 hospitals nationwide, focusing on quality stroke service management. Data analysis included patient demographics, stroke severity assessment, and discharge prognosis measurement using standardized scales.
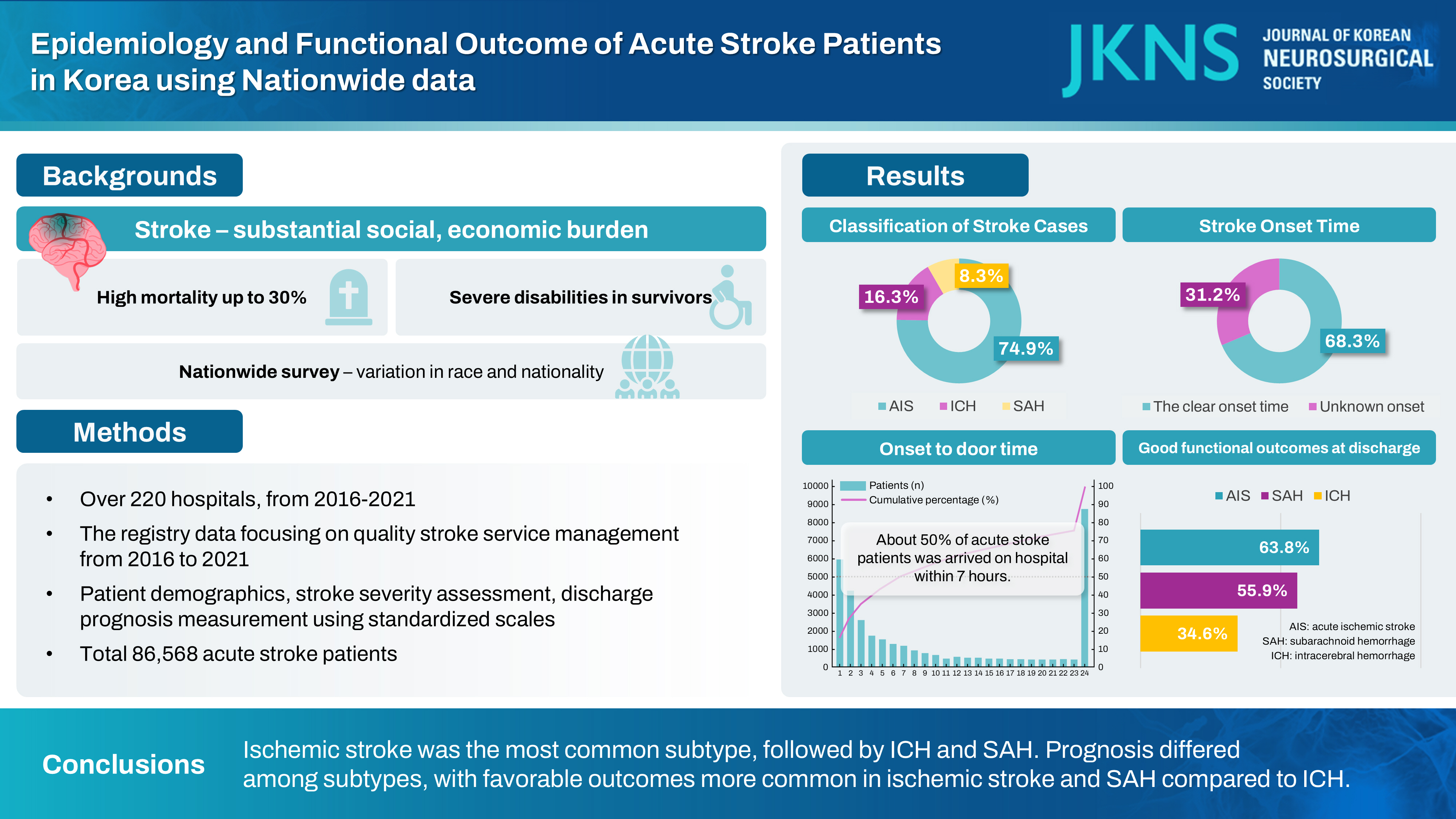
Results
: Eighty-six thousand five hundred sixty-eight acute stroke patients were collected with demographic and clinical characteristics during 18 months from 2016, 2018, and between 2020 to 2021, focusing on acute subarachnoid hemorrhage (SAH), acute intracerebral hemorrhage (ICH), and acute ischemic stroke. Of these 86568 patients, 8.3% was SAH, 16.3% ICH, and 74.9% ischemic stroke. Trends showed decreasing SAH and increasing ICH cases over the years. 68.3% stroke patients had the clear onset time. 49.6% stroke patients arrived within 4.5 hours of symptom onset, with more patients treated at general hospitals. Good functional outcomes at discharge was obtained with 58.3% of acute stroke patients, 55.9% of SAH patients, 34.6% of ICH patients, and 63.8% of ischemic stroke patients.
Conclusion
: The results showed that ischemic stroke was the most common subtype, followed by ICH and SAH. Prognosis differed among subtypes, with favorable outcomes more common in ischemic stroke and SAH compared to ICH.
Figure
Cited by 1 articles
-
Editors’ Pick in March 2025
Hee-Jin Yang
J Korean Neurosurg Soc. 2025;68(2):111-112. doi: 10.3340/jkns.2025.0046.
Reference
-
References
1. Chen RL, Balami JS, Esiri MM, Chen LK, Buchan AM. Ischemic stroke in the elderly: an overview of evidence. Nat Rev Neurol. 6:256–265. 2010.
Article2. Hamdan A, Barnes J, Mitchell P. Subarachnoid hemorrhage and the female sex: analysis of risk factors, aneurysm characteristics, and outcomes. J Neurosurg. 121:1367–1373. 2014.
Article3. Heldner MR, Zubler C, Mattle HP, Schroth G, Weck A, Mono ML, et al. National institutes of health stroke scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke. 44:1153–1157. 2013.
Article4. Heo NH, Lee MR, Yang KH, Hong OR, Shin JH, Lee BY, et al. Short- and long-term mortality after intravenous thrombolysis for acute ischemic stroke: a propensity score-matched cohort with 5-year follow-up. Medicine (Baltimore). 100:e27652. 2021.5. Kim H, Marchuk DA, Pawlikowska L, Chen Y, Su H, Yang GY, et al. : Genetic considerations relevant to intracranial hemorrhage and brain arteriovenous malformations in Huang FP, Xi G, Muraszko K, Zhou LF, Keep RF, Chen XC, et al. (eds) : Cerebral Hemorrhage. Acta Neurochirurgica Supplementum. Vienna : Springer, Vol 105, pp199-206.6. Lee JY, Heo NH, Lee MR, Ahn JM, Oh HJ, Shim JJ, et al. Short and long-term outcomes of subarachnoid hemorrhage treatment according to hospital volume in Korea: a nationwide multicenter registry. J Korean Med Sci. 36:e146. 2021.
Article7. Park SW, Han JJ, Heo NH, Lee EC, Lee DH, Lee JY, et al. High-volume hospital had lower mortality of severe intracerebral hemorrhage patients. J Korean Neurosurg Soc. 67:622–636. 2024.
Article8. Park SW, Lee JY, Heo NH, Han JJ, Lee EC, Hong DY, et al. Change of mortality of patients with acute ischemic stroke before and after 2015. Front Neurol. 13:947992. 2022.
Article9. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 46:3020–3235. 2015.
Article10. Roeder HJ, Lopez JR, Miller EC. Ischemic stroke and cerebral venous sinus thrombosis in pregnancy. Handb Clin Neurol. 172:3–31. 2020.
Article11. Singer J, Gustafson D, Cummings C, Egelko A, Mlabasati J, Conigliaro A, et al. Independent ischemic stroke risk factors in older Americans: a systematic review. Aging (Albany NY). 11:3392–3407. 2019.
Article12. Tabuchi S. Relationship between postmenopausal estrogen deficiency and aneurysmal subarachnoid hemorrhage. Behav Neurol. 2015:720141. 2015.
Article13. Tada Y, Wada K, Shimada K, Makino H, Liang EI, Murakami S, et al. Estrogen protects against intracranial aneurysm rupture in ovariectomized mice. Hypertension. 63:1339–1344. 2014.
Article14. Turan N, Heider RA, Zaharieva D, Ahmad FU, Barrow DL, Pradilla G. Sex differences in the formation of intracranial aneurysms and incidence and outcome of subarachnoid hemorrhage: review of experimental and human studies. Transl Stroke Res. 7:12–19. 2016.
Article15. Wáng YX, He J, Zhang L, Li Y, Zhao L, Liu H, et al. A higher aneurysmal subarachnoid hemorrhage incidence in women prior to menopause: a retrospective analysis of 4,895 cases from eight hospitals in China. Quant Imaging Med Surg. 6:151–156. 2016.
Article16. Weir CJ, Bradford AP, Lees KR. The prognostic value of the components of the glasgow coma scale following acute stroke. QJM. 96:67–74. 2003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association between Neurological Prognosis and Serum Glucose Level by Stroke Subtype in Acute Ischemic Stroke
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Epidemiology of Stroke in Korea
- The Significance of Motor Evoked Potentials as a Prognostic Factor in the Early Stage of Stroke Patients
- Clinical Assessment in Stroke Patients: Introduction of Neurologic Stroke Scales