Ann Hepatobiliary Pancreat Surg.
2024 Nov;28(4):516-521. 10.14701/ahbps.24-101.
Liver transplantation for organ failure following multiple locoregional treatments for breast cancer metastasis
- Affiliations
-
- 1Department of General, Hepatobiliary and Pancreatic Surgery, Liver Transplantation Service, San Camillo Forlanini Hospital, Rome, Italy
- 2Department of Hepatology, San Camillo Forlanini Hospital, Rome, Italy
- 3Department of Interventional Radiology, San Camillo Forlanini Hospital, Rome, Italy
- 4Department of Nuclear Medicine, San Camillo Forlanini Hospital, Rome, Italy
- 5Department of Oncology, Sapienza University of Rome, Rome, Italy
- KMID: 2561585
- DOI: http://doi.org/10.14701/ahbps.24-101
Abstract
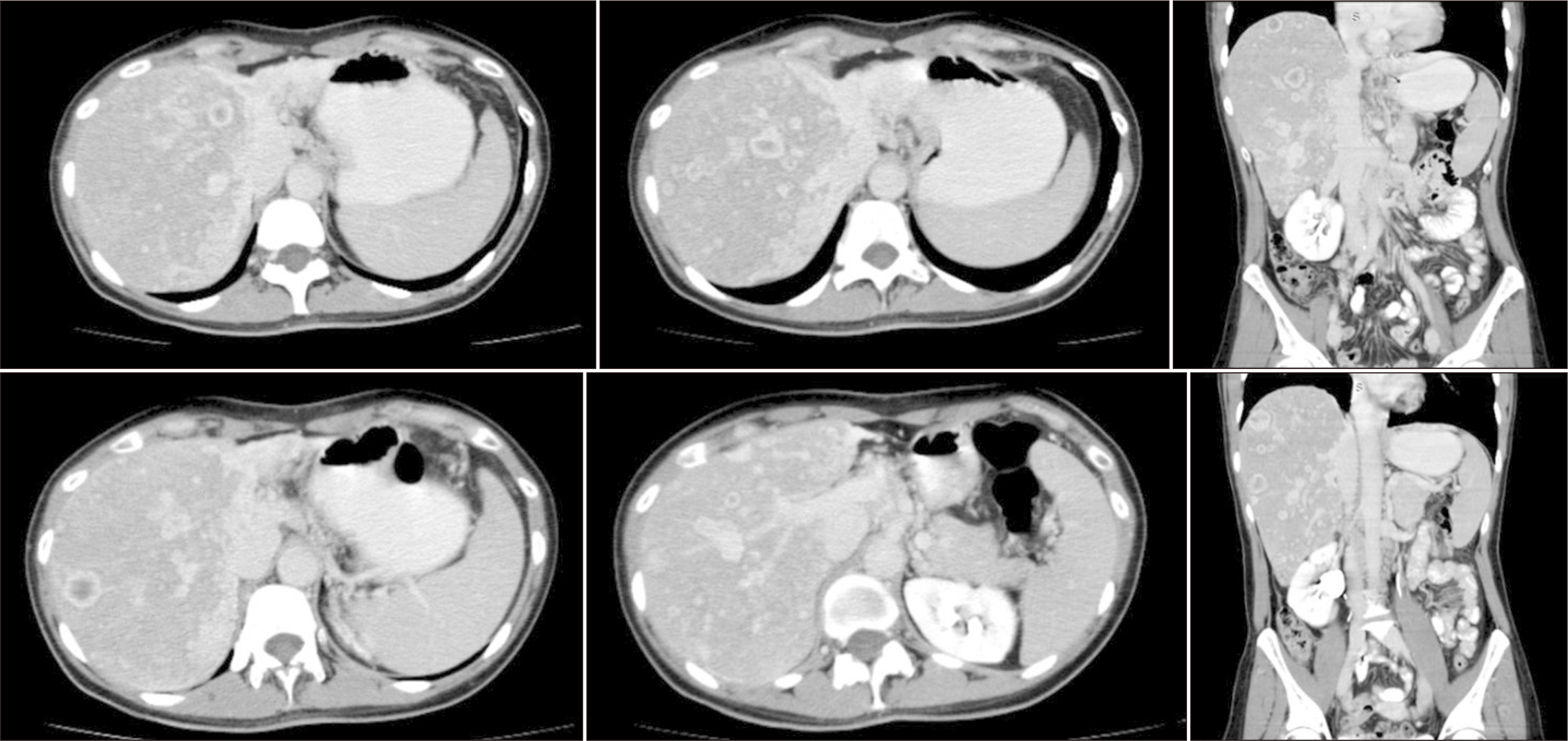
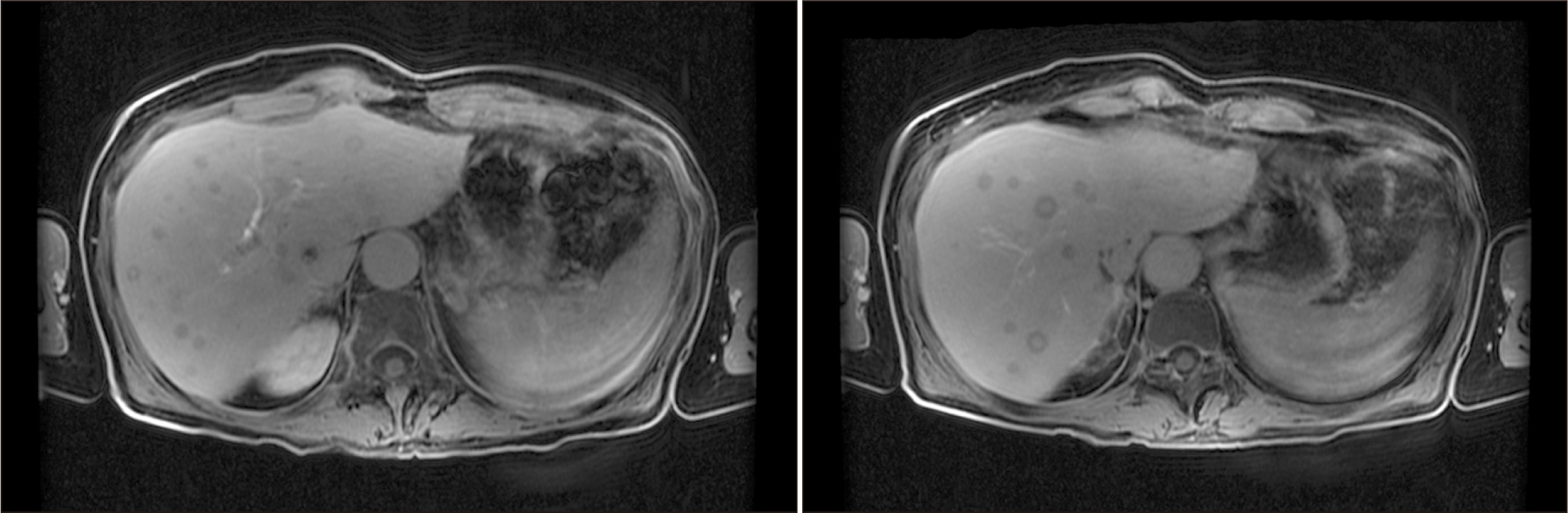
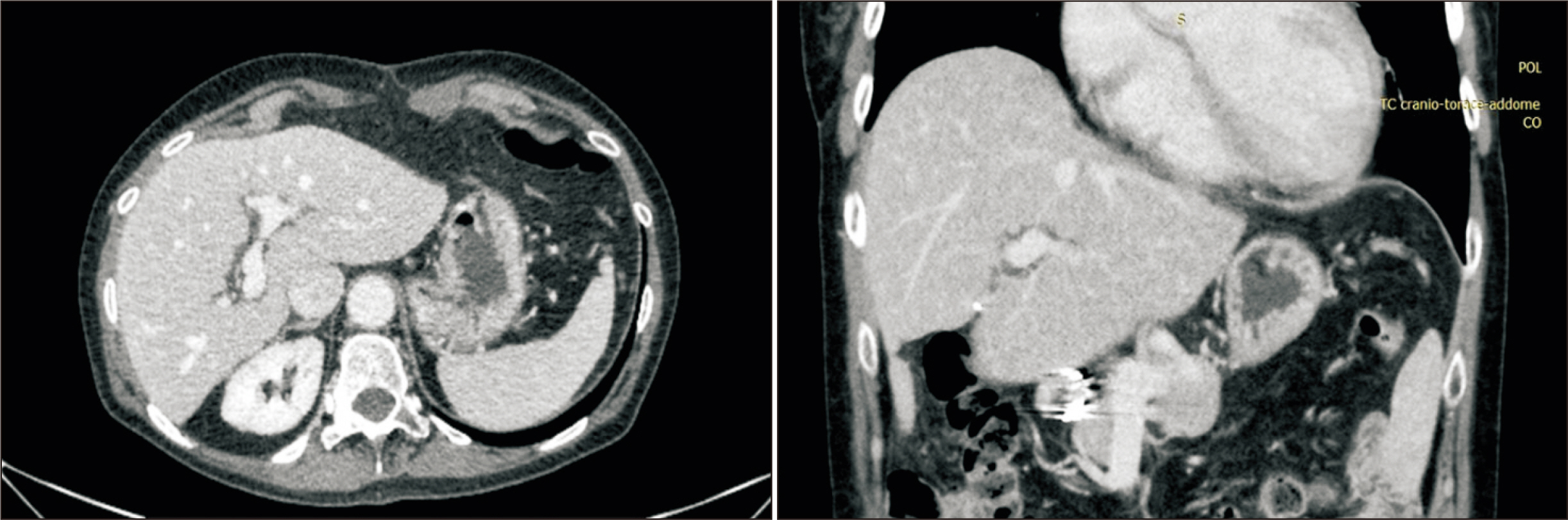
- Patients with nonresectable breast cancer liver metastasis (BCLM) face a dismal prognosis. Despite liver transplantation (LT) for metastatic liver tumors having recently shown good results, BCLM represents an absolute contraindication. This study aimed to investigate the potential for long-term survival after LT for BCLMs in a patient experiencing end-stage liver disease, following multiple oncologic treatments. In July 2019, we performed a deceased donor LT on a 41-year-old female with BCLM controlled with human epidermal growth factor receptor 2 targeted therapy, who developed liver failure following multiple locoregional liver-directed treatments. The primary tumor was treated with surgical resection and adjuvant chemoradiation in 2000. The procedure was performed under a protocol approved by the local ethical committee, and by the Italian National Transplant Center. A 12-month treatment with trastuzumab was performed immediately after LT. Immunosuppression following transplantation was undertaken without steroids, and with everolimus. The patient completed 12 months of follow-up without recurrence. Trastuzumab was then withdrawn. Fifteen months after LT, a liver recurrence occurred that was treated with chemotherapy. In October 2021, she developed 2 brain lesions that were treated with stereotactic radiation. The patient is still alive, with a positron emission tomography/computed tomography performed in January 2024 showing no disease. LT for this patient with BCLM of extreme selectivity showed a good clinical outcome. Perioperative systemic treatment and tumor control are necessary. A specific protocol should be discussed within a multidisciplinary team, and with local and national authorities. Even if tumor recurrence occurs, multimodal therapy can control the disease.
Keyword
Figure
Reference
-
References
1. Giaquinto AN, Sung H, Miller KD, Kramer JL, Newman LA, Minihan A, et al. 2022; Breast cancer statistics, 2022. CA Cancer J Clin. 72:524–541. DOI: 10.3322/caac.21754. PMID: 36190501.2. Khanfir A, Lahiani F, Bouzguenda R, Ayedi I, Daoud J, Frikha M. 2013; Prognostic factors and survival in metastatic breast cancer: a single institution experience. Rep Pract Oncol Radiother. 18:127–132. DOI: 10.1016/j.rpor.2013.01.001. PMID: 24416543. PMCID: PMC3863182.3. Vertriest C, Berardi G, Tomassini F, Vanden Broucke R, Depypere H, Cocquyt V, et al. 2015; Resection of single metachronous liver metastases from breast cancer stage I-II yield excellent overall and disease-free survival. Single center experience and review of the literature. Dig Surg. 32:52–59. DOI: 10.1159/000375132. PMID: 25675843.4. Wyld L, Gutteridge E, Pinder SE, James JJ, Chan SY, Cheung KL, et al. 2003; Prognostic factors for patients with hepatic metastases from breast cancer. Br J Cancer. 89:284–290. DOI: 10.1038/sj.bjc.6601038. PMID: 12865918. PMCID: PMC2394248.5. Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, et al. 2017; 11 years' follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet. 389:1195–1205. DOI: 10.1016/S0140-6736(16)32616-2. PMID: 28215665.6. Wilson JM, Carder P, Downey S, Davies MH, Wyatt JI, Brennan TG. 2003; Treatment of metastatic breast cancer with liver transplantation. Breast J. 9:126–128. DOI: 10.1046/j.1524-4741.2003.09217.x. PMID: 12603387.7. Fendler WP, Lechner H, Todica A, Paprottka KJ, Paprottka PM, Jakobs TF, et al. 2016; Safety, efficacy, and prognostic factors after radioembolization of hepatic metastases from breast cancer: a large single-center experience in 81 patients. J Nucl Med. 57:517–523. DOI: 10.2967/jnumed.115.165050. PMID: 26742710.8. Forner A, Llovet JM, Bruix J. 2012; Chemoembolization for intermediate HCC: is there proof of survival benefit? J Hepatol. 56:984–986. DOI: 10.1016/j.jhep.2011.08.017. PMID: 22008737.9. Hickey R, Lewandowski R, Salem R. 2015; Yttrium-90 radioembolization is a viable treatment option for unresectable, chemorefractory colorectal cancer liver metastases: further evidence in support of a new treatment paradigm. Ann Surg Oncol. 22:706–707. DOI: 10.1245/s10434-014-4165-9. PMID: 25358665.10. Sapisochin G, Hibi T, Toso C, Man K, Berenguer M, Heimbach J, et al. 2021; Transplant oncology in primary and metastatic liver tumors: principles, evidence, and opportunities. Ann Surg. 273:483–493. DOI: 10.1097/SLA.0000000000004071. PMID: 33065633.11. Mazzaferro V, Sposito C, Coppa J, Miceli R, Bhoori S, Bongini M, et al. 2016; The long-term benefit of liver transplantation for hepatic metastases from neuroendocrine tumors. Am J Transplant. 16:2892–2902. DOI: 10.1111/ajt.13831. PMID: 27134017.12. Varley R, Tarazi M, Davé M, Mobarak S, Stott MC, Baltatzis M, et al. 2021; Liver transplantation for non-resectable liver metastases from colorectal cancer: a systematic review and meta-analysis. World J Surg. 45:3404–3413. DOI: 10.1007/s00268-021-06248-4. PMID: 34322717. PMCID: PMC8476371.13. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. 2009; New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247. DOI: 10.1016/j.ejca.2008.10.026. PMID: 19097774.14. Dueland S, Guren TK, Hagness M, Glimelius B, Line PD, Pfeiffer P, et al. 2015; Chemotherapy or liver transplantation for nonresectable liver metastases from colorectal cancer? Ann Surg. 261:956–960. DOI: 10.1097/SLA.0000000000000786. PMID: 24950280.15. Dueland S, Syversveen T, Solheim JM, Solberg S, Grut H, Bjørnbeth BA, et al. 2020; Survival following liver transplantation for patients with nonresectable liver-only colorectal metastases. Ann Surg. 271:212–218. DOI: 10.1097/SLA.0000000000003404. PMID: 31188200.16. Gradishar WJ, Moran MS, Abraham J, Aft R, Agnese D, Allison KH, et al. 2021; NCCN guidelines® insights: breast cancer, version 4.2021. J Natl Compr Canc Netw. 19:484–493. DOI: 10.6004/jnccn.2021.0023. PMID: 34794122.17. Bismuth H. 1994; The need for a consensus agreement on indications of liver transplantation. Hepatology. 20:1S–2S. DOI: 10.1016/0270-9139(94)90263-1. PMID: 8005570.18. Brufsky AM. 2017; Long-term management of patients with hormone receptor-positive metastatic breast cancer: concepts for sequential and combination endocrine-based therapies. Cancer Treat Rev. 59:22–32. DOI: 10.1016/j.ctrv.2017.06.004. PMID: 28719836.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patterns of Locoregional and Systemic Failure after a Mastectomy in Breast Cancer and Risk Factors Predicting Failure
- Decellularlized Matrix in Organ Transplantation
- Current Status of Deceased Donor Liver Transplantation for Alcoholic Liver Disease in Korea in MELD Era
- The Role and Difficulties of the Use of Routine Screening Abdomen Ultrasound for the Detection of a Liver Metastasis in Postoperative Breast Cancer Patients
- The Pattern of Systemic Failure and Factors Influencing on the Outcome after Distant Metastastasis in Breast Cancer