Ewha Med J.
2024 Oct;47(4):e72. 10.12771/emj.2024.e72.
Clinical practice guidelines for the diagnosis and treatment of scabies in Korea: Part 2. Treatment and prevention — a secondary publication
- Affiliations
-
- 1Department of Dermatology, Jeonbuk National University Medical School, Jeonju, Korea
- 2Department of Dermatology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- 3Department of Dermatology, Uijeongbu St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- 4Department of Dermatology, Incheon St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- 5Department of Dermatology, Korea University Guro Hospital, Seoul, Korea
- 6Department of Dermatology, Inha University Hospital, Incheon, Korea
- KMID: 2561425
- DOI: http://doi.org/10.12771/emj.2024.e72
Abstract
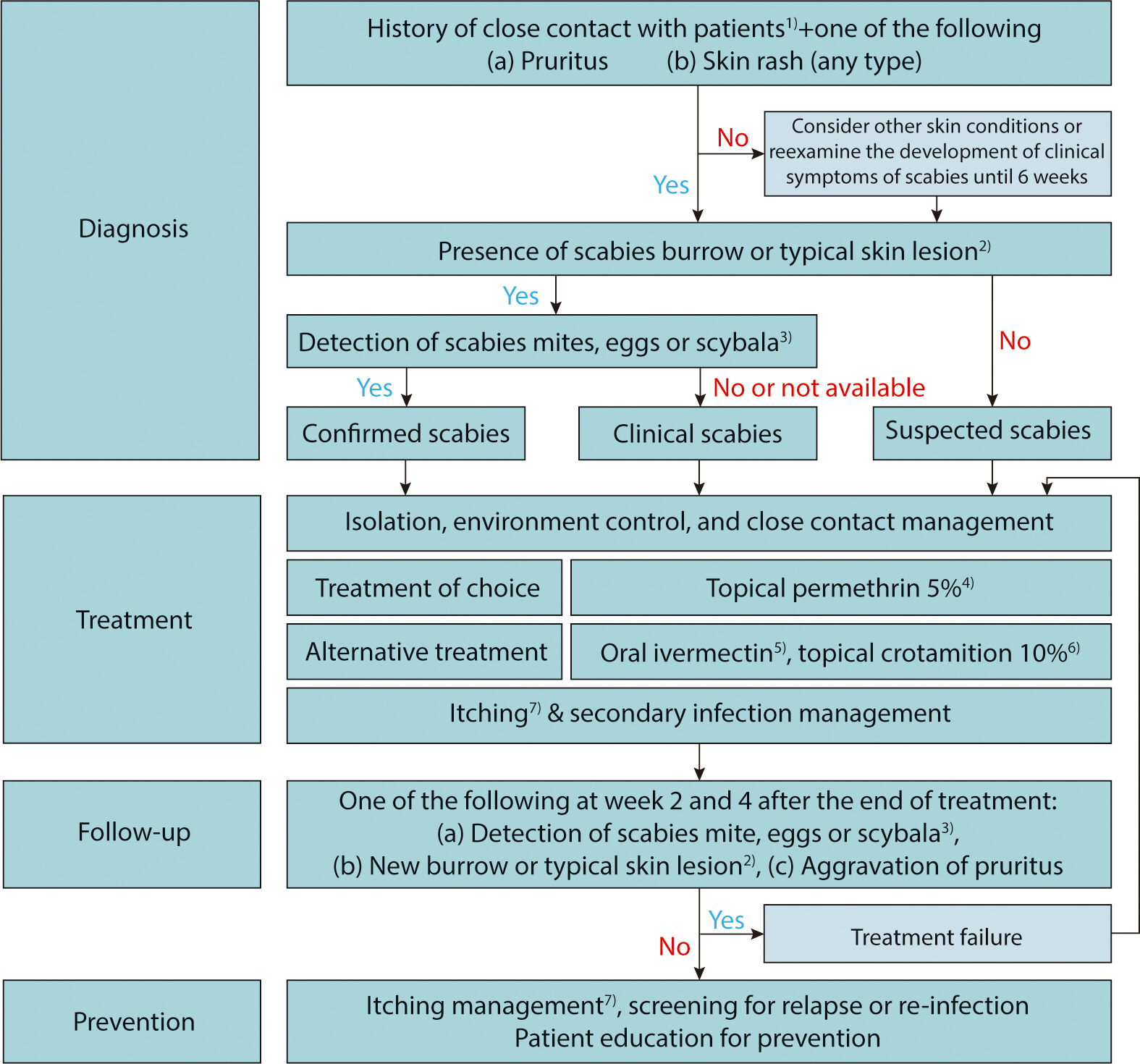
- Treatment should be initiated for all suspected, clinical, or confirmed cases of scabies. Patients affected should be adequately isolated, and high-risk groups with close contact histories should be treated regardless of their symptoms. Optimal treatment strategies can be selected based on age, clinical subtype, and the patient's health status. In Korea, commercially available preparations for scabies treatment include topical 5% permethrin, topical 10% crotamiton, and oral ivermectin. Topical 5% permethrin is the first-line selective treatment for both classic and crusted scabies. Alternative treatments include topical 10% crotamiton and oral ivermectin. After completing treatment, followup visits at 2 and 4 weeks are recommended to monitor the therapeutic response. Treatment is considered to have failed if scabies mites or burrows are detected, new clinical characteristics develop, or there is an aggravation of pruritus. Scabies itch should be adequately managed with emollients, oral antihistamines, and topical corticosteroids. Preventive measures, including personal hygiene, patient education, and environmental control, should be implemented to reduce the transmission of scabies.
Figure
Cited by 1 articles
Reference
-
References
1. Rosumeck S, Nast A, Dressler C. Evaluation of ivermectin vs permethrin for treating scabies: summary of a Cochrane review. JAMA Dermatol. 2019; 155(6):730–732. DOI: 10.1001/jamadermatol.2019.0279. PMID: 31017622.
Article2. Pallesen K, Lassen JA, Munk NT, Hartmeyer GN, Hvid L, Bygum A. In vitro survival of scabies mites. Clin Exp Dermatol. 2020; 45(6):712–715. DOI: 10.1111/ced.14209. PMID: 32112428.3. Hackenberg B, Horváth ON, Petachti M, Schult R, Yenigün N, Bannenberg P. Skabiestherapie in Deutschland: ergebnisse einer bundesweiten umfrage mit besonderem fokus auf die wirksamkeit der erstlinientherapie mit permethrin. Hautarzt. 2020; 71(5):374–379. DOI: 10.1007/s00105-020-04561-y. PMID: 32144440.4. Mazzatenta C, Piccolo V, Argenziano G, Bassi A. Is scabies becoming less sensitive to permethrin therapy? J Eur Acad Dermatol Venereol. 2021; 35(9):e607–e609. DOI: 10.1111/jdv.17339.5. Meyersburg D, Kaiser A, Bauer JW. ‘Loss of efficacy of topical 5% permethrin for treating scabies: an Austrian single-center study’. J Dermatolog Treat. 2022; 33(2):774–777. DOI: 10.1080/09546634.2020.1774489. PMID: 32495666.
Article6. Centers for Disease Control and Prevention (CDC)’s Division of Parasitic Diseases and Malaria. Resources of health professionals - medication, in: parasites – scabies [Internet]. Atlanta (GA): CDC;c2023. [cited 2023 Jun 12]. Available from. https://www.cdc.gov/parasites/scabies/health_professionals/meds.html.7. Salavastru CM, Chosidow O, Boffa MJ, Janier M, Tiplica GS. European guideline for the management of scabies. J Eur Acad Dermatol Venereol. 2017; 31(8):1248–1253. DOI: 10.1111/jdv.14351. PMID: 28639722.
Article8. Executive Committee of Guideline for the Diagnosis and Treatment of Scabies. Guideline for the diagnosis and treatment of scabies in Japan. J Dermatol. 2017; 44(9):991–1014. DOI: 10.1111/1346-8138.13896. PMID: 28561292.9. Richards RN. Scabies: diagnostic and therapeutic update. J Cutan Med Surg. 2021; 25(1):95–101. DOI: 10.1177/1203475420960446. PMID: 32998532.
Article10. Nishizawa T, Ishikawa K, Takamizawa M, Arioka H. Successful treatment of refractory crusted scabies. BMJ Case Rep. 2022; 15:e251842. DOI: 10.1136/bcr-2022-251842. PMID: 36357115. PMCID: PMC9660564.11. Currie BJ, McCarthy JS. Permethrin and ivermectin for scabies. N Engl J Med. 2010; 362(8):717–725. DOI: 10.1056/NEJMct0910329. PMID: 20181973.
Article12. Sunderkötter C, Feldmeier H, Fölster-Holst R, Geisel B, Klinke-Rehbein S, Nast A, et al. S1 guidelines on the diagnosis and treatment of scabies – short version. J Dtsch Dermatol Ges. 2016; 14(11):1155–1167. DOI: 10.1111/ddg.13130. PMID: 27879074.13. Mumcuoglu KY, Gilead LT. Recommendations for the treatment of scabies infestations in Israel. Isr Med Assoc J. 2006; 8(3):196–199.14. van der Rhee HJ, Farquhar JA, Vermeulen NP. Efficacy and transdermal absorption of permethrin in scabies patients. Acta Derm Venereol. 1989; 69(2):170–173.15. Fölster-Holst R, Rufli T, Christophers E. Die skabiestherapie unter besonderer berücksichtigung des frühen kindesalters, der schwangerschaft und stillzeit. Hautarzt. 2000; 51(1):7–13. DOI: 10.1007/s001050050003. PMID: 10663033.
Article16. Romani L, Whitfeld MJ, Koroivueta J, Kama M, Wand H, Tikoduadua L, et al. Mass drug administration for scabies control in a population with endemic disease. N Engl J Med. 2015; 373(24):2305–2313. DOI: 10.1056/NEJMoa1500987. PMID: 26650152.
Article17. Strong M, Johnstone P. Interventions for treating scabies. Cochrane Database Syst Rev. 2007; 2007(3):CD000320. DOI: 10.1002/14651858.CD000320.pub2. PMID: 17636630. PMCID: PMC6532717.
Article18. Jannic A, Bernigaud C, Brenaut E, Chosidow O. Scabies itch. Dermatol Clin. 2018; 36(3):301–308. DOI: 10.1016/j.det.2018.02.009. PMID: 29929601.
Article19. Bhat SA, Mounsey KE, Liu X, Walton SF. Host immune responses to the itch mite, Sarcoptes scabiei, in humans. Parasit Vectors. 2017; 10(1):385. DOI: 10.1186/s13071-017-2320-4. PMID: 28797273. PMCID: PMC5553898.20. Kim HS, Hashimoto T, Fischer K, Bernigaud C, Chosidow O, Yosipovitch G. Scabies itch: an update on neuroimmune interactions and novel targets. J Eur Acad Dermatol Venereol. 2021; 35(9):1765–1776. DOI: 10.1111/jdv.17334. PMID: 33960033.21. Thomas C, Coates SJ, Engelman D, Chosidow O, Chang AY. Ectoparasites: scabies. J Am Acad Dermatol. 2020; 82(3):533–548. DOI: 10.1016/j.jaad.2019.05.109. PMID: 31310840.22. Sunderkötter C, Wohlrab J, Hamm H. Scabies: epidemiology, diagnosis, and treatment. Dtsch Arztebl Int. 2021; 118:695–704. DOI: 10.3238/arztebl.m2021.0296. PMID: 34615594. PMCID: PMC8743988.
Article23. Bernigaud C, Fischer K, Chosidow O. The management of scabies in the 21st century: past, advances and potentials. Acta Derm Venereol. 2020; 100(9):adv00112. DOI: 10.2340/00015555-3468. PMID: 32207535. PMCID: PMC9128908.24. Mittal A, Garg A, Agarwal N, Gupta L, Khare AK. Treatment of nodular scabies with topical tacrolimus. Indian Dermatol Online J. 2013; 4(1):52–53. DOI: 10.4103/2229-5178.105486. PMID: 23437425. PMCID: PMC3573456.
Article25. Kim JC, Chung BY, Lee SY, Park JS, Kang SY, Cho SI, et al. The prognosis of post-scabetic itch. J Korean Dermatol Assoc. 2023; 61(1):43–51.26. Legat FJ. The antipruritic effect of phototherapy. Front Med. 2018; 5:333. DOI: 10.3389/fmed.2018.00333. PMID: 30560129. PMCID: PMC6287194.
Article27. Widaty S, Miranda E, Cornain EF, Rizky LA. Scabies: update on treatment and efforts for prevention and control in highly endemic settings. J Infect Dev Ctries. 2022; 16(02):244–251. DOI: 10.3855/jidc.15222. PMID: 35298417.
Article28. May PJ, Tong SYC, Steer AC, Currie BJ, Andrews RM, Carapetis JR, et al. Treatment, prevention and public health management of impetigo, scabies, crusted scabies and fungal skin infections in endemic populations: a systematic review. Trop Med Int Health. 2019; 24(3):280–293. DOI: 10.1111/tmi.13198. PMID: 30582783. PMCID: PMC6850630.
Article29. Ong CY, Vasanwala FF. Infected with scabies again? Focus in management in long-term care facilities. Diseases. 2018; 7(1):3. DOI: 10.3390/diseases7010003. PMID: 30597979. PMCID: PMC6473425.
Article30. McCarthy-Khan P. Infection prevention and control–standard operating procedure for scabies in a healthcare setting. Geneva: Infection Prevention and Control Policy Review Group;2021.31. Korea Disease Control and Prevention Agency. Guide for prevention and management of scabies and head lice. Cheongju: Korea Disease Control and Prevention Agency;2018.32. Korea Disease Control and Prevention Agency. Guide for prevention and management of scabies in convalescent hospital. Cheongju: Korea Disease Control and Prevention Agency;2019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Practice Guidelines for the Diagnosis and Treatment of Scabies in Korea: Part 2. Treatment and Prevention
- Clinical practice guidelines for the diagnosis and treatment of scabies in Korea: Part 1. Epidemiology, clinical manifestations, and diagnosis — a secondary publication
- Clinical Practice Guidelines for the Diagnosis and Treatment of Scabies in Korea: Part 1. Epidemiology, Clinical Manifestations, and Diagnosis
- Guideline for the diagnosis and treatment of scabies
- Secondary Prevention as Integral Part of Stroke Rehabilitation