Ewha Med J.
2024 Oct;47(4):e60. 10.12771/emj.2024.e60.
Reduced cardiovascular events through dynamic lifestyle modification in individuals with prediabetes or prehypertension in Korea: a nationwide cohort study
- Affiliations
-
- 1Department of Cardiology, Korea University Anam Hospital, Seoul, Korea
- 2Department of Cardiology, Ewha Womans University Medical Center, Seoul, Korea
- 3Department of Gastroenterology, Ewha Womans University Medical Center, Seoul, Korea
- 4Clinical Trial Center, Ewha Womans University Medical Center, Seoul, Korea
- KMID: 2561415
- DOI: http://doi.org/10.12771/emj.2024.e60
Abstract
Objectives
There is limited knowledge regarding the impact of lifestyle changes on cardiovascular events and mortality among individuals with prehypertension or prediabetes.
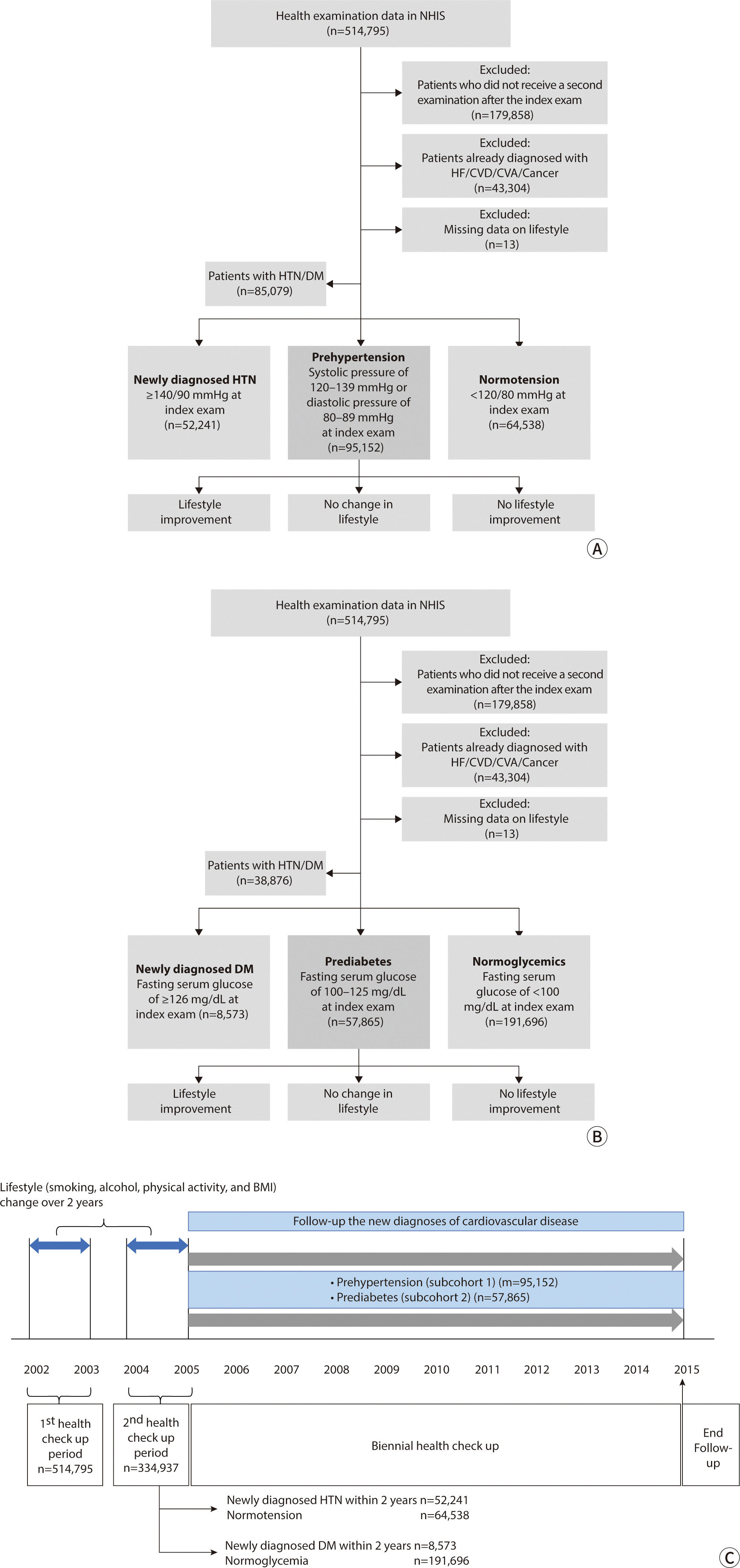
Methods
This was a serial retrospective cohort study utilizing data from the Korean National Health Insurance Service Health Screening Cohort. The primary outcome considered in the study was major adverse cardiovascular events (MACE).
Results
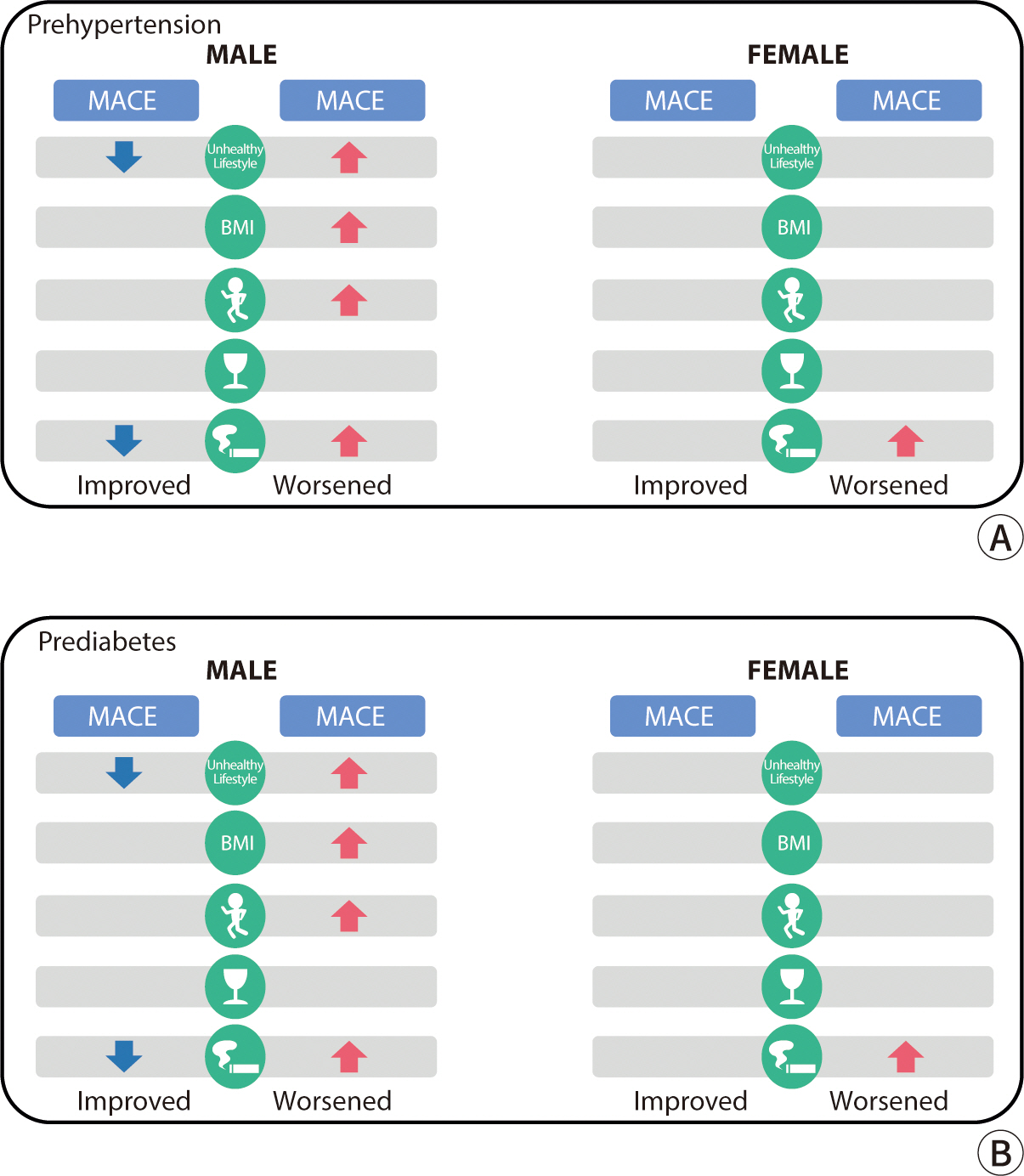
A higher risk of MACE was found in men with prehypertension whose unhealthy lifestyle deteriorated (hazard ratio [HR], 1.13; 95% CI, 1.04–1.23; P=0.004), those who gained weight (HR, 1.15; 95% CI, 1.03–1.28; P=0.010), and those who began smoking (HR, 1.34; 95% CI, 1.17–1.55; P<0.001). Conversely, a reduced risk of MACE was observed in men with prehypertension who improved their unhealthy lifestyle, quit smoking, reduced alcohol consumption, or increased the frequency of physical activity. In men with prediabetes, the risk of MACE was higher in those whose unhealthy lifestyle worsened (HR, 1.23; 95% CI, 1.12–1.35; P<0.001), those who gained weight (HR, 1.19; 95% CI, 1.06–1.33; P=0.003), those who started smoking (HR, 1.41; 95% CI, 1.22–1.64; P<0.001), and those who decreased their physical activity frequency (HR, 1.21; 95% CI, 1.09–1.35; P<0.001).
Conclusion
Preventive lifestyle changes reduce cardiovascular events and mortality, particularly in men at risk of developing hypertension or type 2 diabetes.
Figure
Reference
-
References
1. Gong Q, Zhang P, Wang J, Ma J, An Y, Chen Y, et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol. 2019; 7(6):452–461. DOI: 10.1016/S2213-8587(19)30093-2. PMID: 31036503.
Article2. Faselis C, Doumas M, Kokkinos JP, Panagiotakos D, Kheirbek R, Sheriff HM, et al. Exercise capacity and progression from prehypertension to hypertension. Hypertension. 2012; 60(2):333–338. DOI: 10.1161/HYPERTENSIONAHA.112.196493. PMID: 22753224.
Article3. Lu Q, Zhang Y, Geng T, Yang K, Guo K, Min X, et al. Association of lifestyle factors and antihypertensive medication use with risk of all-cause and cause-specific mortality among adults with hypertension in China. JAMA Netw Open. 2022; 5(2):2146118. DOI: 10.1001/jamanetworkopen.2021.46118. PMID: 35103793. PMCID: PMC8808332.4. Schlesinger S, Neuenschwander M, Ballon A, Nöthlings U, Barbaresko J. Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies. J Epidemiol Community Health. 2020; 74(5):481–487. DOI: 10.1136/jech-2019-213415. PMID: 32075860.
Article5. Ghadieh AS, Saab B. Evidence for exercise training in the management of hypertension in adults. Can Fam Physician. 2015; 61(3):233–239.6. Puddey IB, Beilin LJ, Vandongen R. Regular alcohol use raises blood pressure in treated hypertensive subjects: a randomised controlled trial. Lancet. 1987; 329(8534):647–651. DOI: 10.1016/S0140-6736(87)90413-2. PMID: 2882082.
Article7. Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006; 29(9):2102–2107. DOI: 10.2337/dc06-0560. PMID: 16936160. PMCID: PMC1762038.8. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7(9):016640. DOI: 10.1136/bmjopen-2017-016640. PMID: 28947447. PMCID: PMC5623538.9. Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005; 294(4):466–472. DOI: 10.1001/jama.294.4.466. PMID: 16046653.10. Kim JW, Park CG, Hong SJ, Park SM, Rha SW, Seo HS, et al. Acute and chronic effects of cigarette smoking on arterial stiffness. Blood Press. 2005; 14(2):80–85. DOI: 10.1080/08037050510008896. PMID: 16036484.11. Thuy AB, Blizzard L, Schmidt MD, Luc PH, Granger RH, Dwyer T. The association between smoking and hypertension in a population-based sample of Vietnamese men. J Hypertens. 2010; 28(2):245–250. DOI: 10.1097/HJH.0b013e32833310e0. PMID: 19829145.
Article12. Aeschbacher S, Schoen T, Clair C, Schillinger P, Schönenberger S, Risch M, et al. Association of smoking and nicotine dependence with pre-diabetes in young and healthy adults. Swiss Med Wkly. 2014; 144(4142):w14019. DOI: 10.4414/smw.2014.14019. PMID: 25295968.13. Foy CG, Bell RA, Farmer DF, Goff DC Jr, Wagenknecht LE. Smoking and incidence of diabetes among U.S. adults: findings from the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2005; 28(10):2501–2507. DOI: 10.2337/diacare.28.10.2501. PMID: 16186287.14. Will JC, Galuska DA, Ford ES, Mokdad A, Calle EE. Cigarette smoking and diabetes mellitus: evidence of a positive association from a large prospective cohort study. Int J Epidemiol. 2001; 30(3):540–546. DOI: 10.1093/ije/30.3.540. PMID: 11416080.
Article15. Beziaud F, Halimi JM, Lecomte P, Tichet J. Cigarette smoking and diabetes mellitus. Diabetes Metab. 2004; 30(2):161–166. DOI: 10.1016/S1262-3636(07)70102-7. PMID: 15223988.
Article16. Morrish NJ, Stevens LK, Fuller JH, Jarrett RJ, Keen H. Risk factors for macrovascular disease in diabetes mellitus: the London follow-up to the WHO Multinational Study of Vascular Disease in Diabetics. Diabetologia. 1991; 34(8):590–594. DOI: 10.1007/BF00400279. PMID: 1936663.
Article17. Pan A, Wang Y, Talaei M, Hu FB. Relation of smoking with total mortality and cardiovascular events among patients with diabetes mellitus: a meta-analysis and systematic review. Circulation. 2015; 132(19):1795–1804. DOI: 10.1161/CIRCULATIONAHA.115.017926. PMID: 26311724. PMCID: PMC4643392.
Article18. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013; 309(1):71–82. DOI: 10.1001/jama.2012.113905. PMID: 23280227. PMCID: PMC4855514.
Article19. Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006; 355(8):763–778. DOI: 10.1056/NEJMoa055643. PMID: 16926275.
Article20. Kong KA, Park J, Hong S, Hong YS, Sung YA, Lee H. Associations between body mass index and mortality or cardiovascular events in a general Korean population. PLoS One. 2017; 12(9):0185024. DOI: 10.1371/journal.pone.0185024. PMID: 28915262. PMCID: PMC5600387.21. Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006; 368(9536):666–678. DOI: 10.1016/S0140-6736(06)69251-9. PMID: 16920472.
Article22. Bundhun PK, Li N, Chen MH. Does an obesity paradox really exist after cardiovascular intervention?: a systematic review and meta-analysis of randomized controlled trials and observational studies. Medicine. 2015; 94(44):1910. DOI: 10.1097/MD.0000000000001910. PMID: 26554791. PMCID: PMC4915892.23. Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017; 318(2):175–193. DOI: 10.1001/jama.2017.3303. PMID: 28697259.
Article24. Standl E, Erbach M, Schnell O. Defending the con side: obesity paradox does not exist. Diabetes Care. 2013; 36:Supplement_2. S282–S286. DOI: 10.2337/dcS13-2040. PMID: 23882060. PMCID: PMC3920775.25. Chang SH, Chang YY, Wu LY. Gender differences in lifestyle and risk factors of metabolic syndrome: do women have better health habits than men? J Clin Nurs. 2019; 28(11-12):2225–2234. DOI: 10.1111/jocn.14824. PMID: 30786102.
Article26. Caspersen CJ, Pereira MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc. 2000; 32(9):1601–1609. DOI: 10.1097/00005768-200009000-00013. PMID: 10994912.27. Holtermann A, Schnohr P, Nordestgaard BG, Marott JL. The physical activity paradox in cardiovascular disease and all-cause mortality: the contemporary Copenhagen General Population Study with 104 046 adults. Eur Heart J. 2021; 42(15):1499–1511. DOI: 10.1093/eurheartj/ehab087. PMID: 33831954. PMCID: PMC8046503.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical Nutrition Therapy as a Hospital-Based Lifestyle Modification in the Korean Diabetes Prevention Study
- Prehypertension
- The scientific evidence for the management of prehypertensives and high risk group
- Non-pharmacologic Treatment for Elderly Constipation: Lifestyle Modification
- Association of Serum Vitamin D Status with Prediabetes and Prehypertension in Korean Adults: An Analysis of the 2013–2015 Korea National Health and Nutrition Examination Survey Data