J Stroke.
2024 Sep;26(3):434-445. 10.5853/jos.2024.01389.
Mechanical Thrombectomy Versus Intravenous Thrombolysis in Distal Medium Vessel Acute Ischemic Stroke: A Multinational Multicenter Propensity Score-Matched Study
- Affiliations
-
- 1Department of Radiology, Division of Neuroradiology, Johns Hopkins Medical Center, Baltimore, MD, USA
- 2Neuroendovascular Program, Massachusetts General Hospital, Harvard University, Boston, MA, USA
- 3Department of Neurosurgery and Interventional Neuroradiology, Louisiana State University, Baton Rouge, LA, USA
- 4Department of Neurological Surgery and Montefiore-Einstein Cerebrovascular Research Lab, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY, USA
- 5Department of Neurosurgery, Thomas Jefferson University, Philadelphia, PA, USA
- 6Department of Neurology, University of Massachusetts Chan Medical School, Worcester, MA, USA
- 7Department of Neurology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
- 8Department of Endovascular Neurosurgery and Neuroradiology NJMS, Newark, NJ, USA
- 9Division of Neurointerventional Radiology, Department of Radiology, University of Massachusetts Medical Center, Worcester, MA, USA
- 10Cooper Neurological Institute, Cooper University Hospital, Cooper Medical School of Rowen University, Camden, NJ, USA
- 11Departments of Neurological Surgery & Radiology, Mayo Clinic, Rochester, MN, USA
- 12Department of Neuroradiology, Henri Mondor Hospital, Creteil, France
- 13Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
- 14Division of Neurology, Department of Medicine, National University Hospital, Singapore
- 15Department of Interventional Neuroradiology, Stanford Medical Center, Palo Alto, CA, USA
- 16Neurovascular Centre, Divisions of Therapeutic Neuroradiology and Neurosurgery, St. Michael’s Hospital, Toronto, ON, Canada
- 17Department of Neurosurgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA
- 18University Hospital of Limoges, Neuroradiology Department, Dupuytren, Université de Limoges, Limoges, France
- 19Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 20Department of Neurology, UTHealth McGovern Medical School, Houston, TX, USA
- 21Neuroradiology Department, Sana Kliniken, Lübeck GmbH, Lübeck, Germany
- 22Department of Interventional Radiology, Oregon Health and Science University, Portland, OR, USA
- 23Interventional Neuroradiology Department, Bordeaux University Hospital, Bordeaux, France
- 24Interventistica Neurovascolare, Ospedale Careggi di Firenze, Florence, Italy
- 25Department of Diagnostic and Interventional Neuroradiology, Centro Hospitalar Universitário do Porto, Porto, Portugal
- 26Department of Neurology, University of Cincinnati Medical Center, Cincinnati, OH, USA
- 27Department of Neuroradiology, Gui de Chauliac Hospital, Montpellier University Medical Center, Montpellier, France
- 28Department of Neurosurgery, Tokyo Metropolitan Tama Medical Center, Tokyo, Japan
- 29Division of Stroke and Endovascular Neurosurgery, Department of Neurological Surgery, Keck School of Medicine, University of Southern California (USC), Los Angeles, CA, USA
- 30Department of Neurosurgery, Westchester Medical Center at New York Medical College, Valhalla, NY, USA
- 31Department of Neuroradiology, Pitié-Salpêtrière Hospital, Paris, France; GRC BioFast, Sorbonne University, Paris VI, Paris, France
- 32Departments of Radiology & Neurology, Boston Medical Center, Boston, MA, USA
- 33Department of Neurology, Centro Hospitalar Universitário do Porto, Porto, Portugal
- 34Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, CA, USA
- 35Sektion Vaskuläre und Interventionelle Neuroradiologie, Universitätsklinikum Heidelberg, Heidelberg, Germany
- 36Department of Interventional Neuroradiology, Nancy University Hospital, Nancy, France
- 37INSERM U1254, IADI, Université de Lorraine, Vandoeuvre-les-Nancy, France
- 38Department of Radiology, Interventional Neuroradiology Section, University Medical Center Münster, Münster, Germany
- 39Departments of Neurology & Neurosurgery, Christian Doppler Clinic, Paracelsus Medical University, Salzburg, Austria
- 40UCLA Stroke Center and Department of Neurology Department, University of California, Los Angeles, Los Angeles, CA, USA
- 41UOSA Neuroradiologia Interventistica, Fondazione Policlinico Universitario A. Gemelli IRCCS Roma, Roma, Italy
- 42Department of Neurology, Hôpital Civil Marie Curie, Charleroi, Belgium
- 43Department of Diagnostic and Interventional Neuroradiology, Erasme University Hospital, Brussels, Belgium
- KMID: 2559561
- DOI: http://doi.org/10.5853/jos.2024.01389
Abstract
- Background and Purpose
The management of acute ischemic stroke (AIS) due to distal medium vessel occlusion (DMVO) remains uncertain, particularly in comparing the effectiveness of intravenous thrombolysis (IVT) plus mechanical thrombectomy (MT) versus IVT alone. This study aimed to evaluate the safety and efficacy in DMVO patients treated with either MT-IVT or IVT alone.
Methods
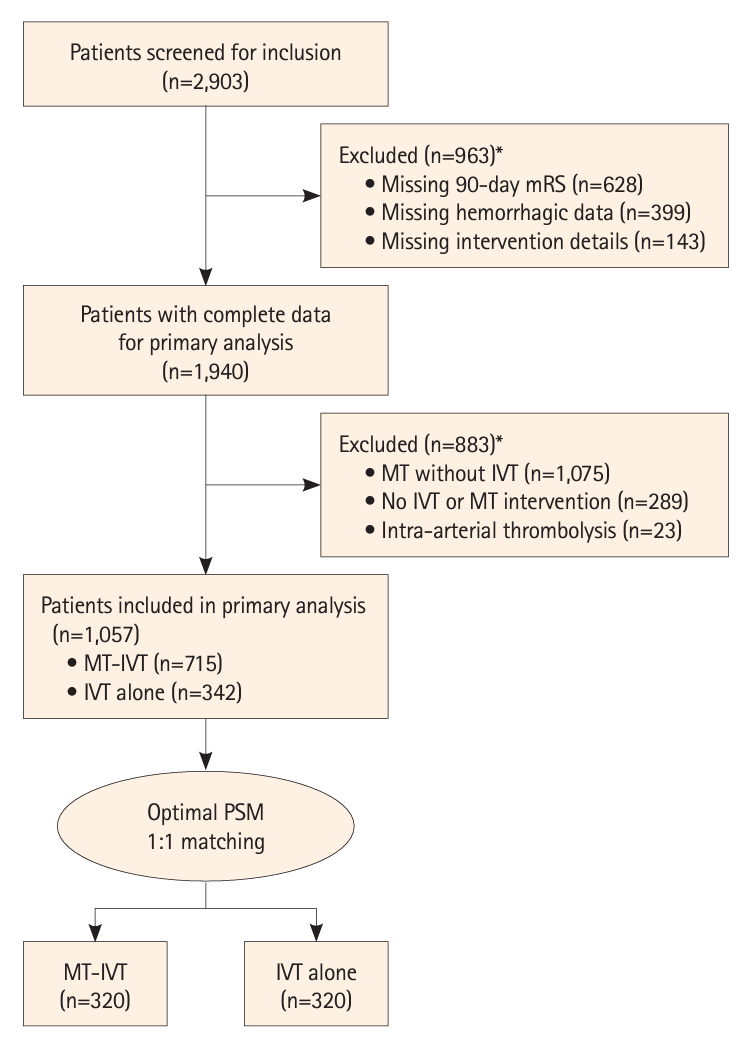
This multinational study analyzed data from 37 centers across North America, Asia, and Europe. Patients with AIS due to DMVO were included, with data collected from September 2017 to July 2023. The primary outcome was functional independence, with secondary outcomes including mortality and safety measures such as types of intracerebral hemorrhage.
Results
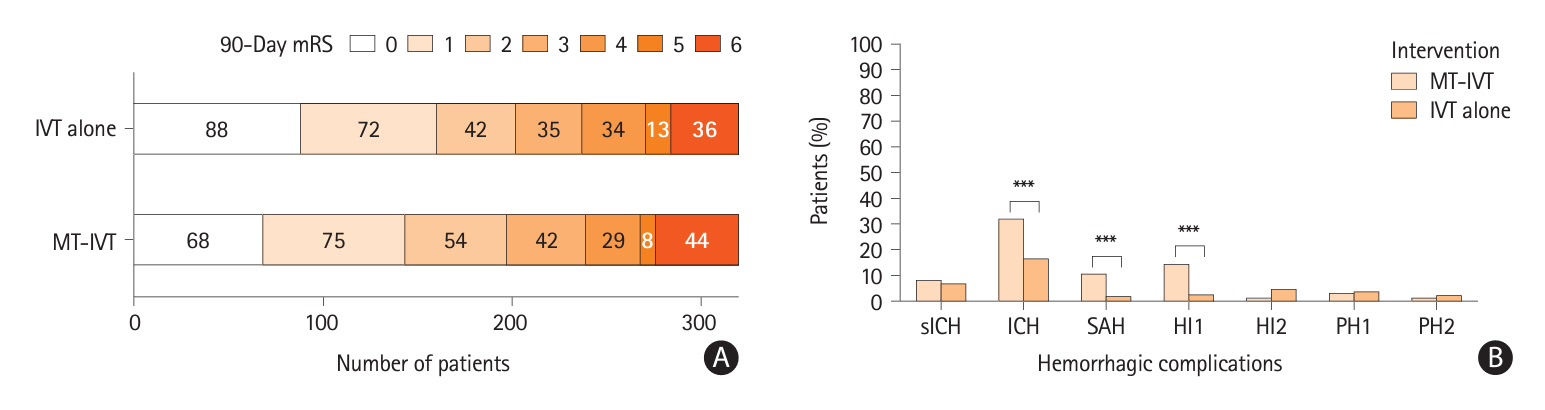
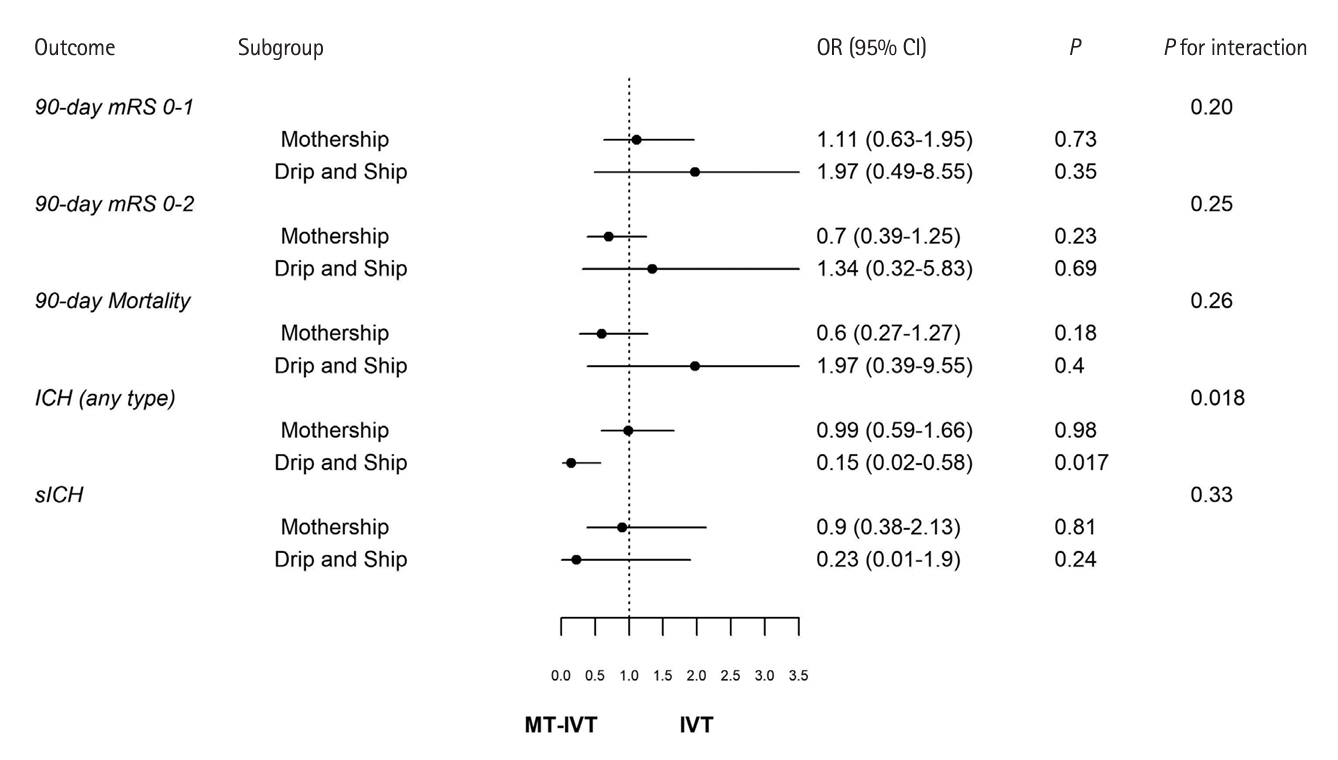
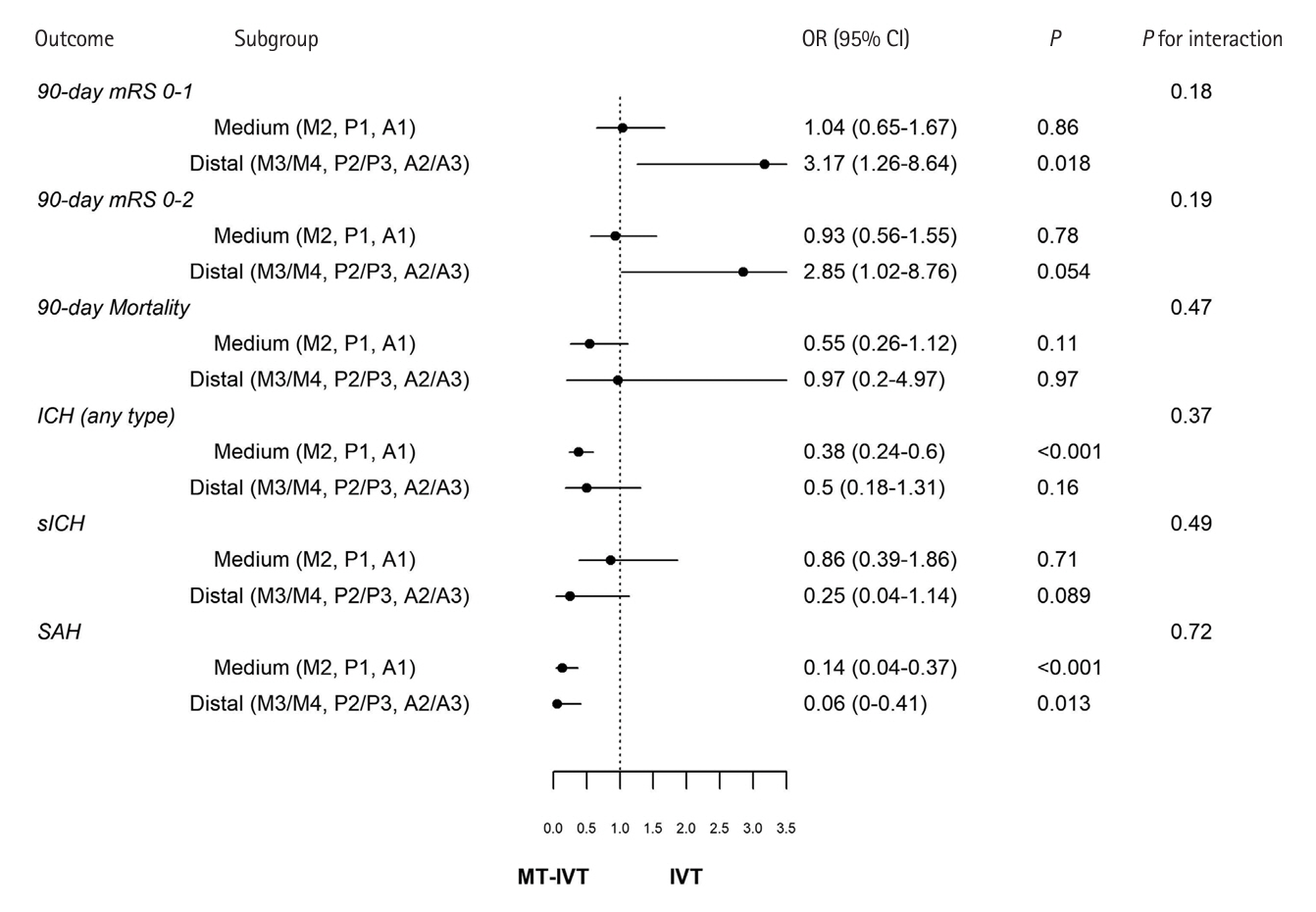
The study involved 1,057 patients before matching, and 640 patients post-matching. Functional outcomes at 90 days showed no significant difference between groups in achieving good functional recovery (modified Rankin Scale 0–1 and 0–2), with adjusted odds ratios (OR) of 1.21 (95% confidence interval [CI] 0.81 to 1.79; P=0.35) and 1.00 (95% CI 0.66 to 1.51; P>0.99), respectively. Mortality rates at 90 days were similar between the two groups (OR 0.75, 95% CI 0.44 to 1.29; P=0.30). The incidence of symptomatic intracerebral hemorrhage was comparable, but any type of intracranial hemorrhage was significantly higher in the MT-IVT group (OR 0.43, 95% CI 0.29 to 0.63; P<0.001).
Conclusion
The results of this study indicate that while MT-IVT and IVT alone show similar functional and mortality outcomes in DMVO patients, MT-IVT presents a higher risk of hemorrhagic complications, thus MT-IVT may not routinely offer additional benefits over IVT alone for all DMVO stroke patients. Further prospective randomized trials are needed to identify patient subgroups most likely to benefit from MT-IVT treatment in DMVO.
Figure
Reference
-
References
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.2. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article3. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.
Article4. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.
Article5. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.6. Ospel JM, Goyal M. A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg. 2021; 13:623–630.
Article7. Australian New Zealand Clinical Trials Registry. Trial review: trial registered on ANZCTR [Internet]. Camperdown: ANZCTR;2021. [accessed March 23, 2024]. Available from: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12621001746820p.8. Dmytriw AA, Musmar B, Salim H, Ghozy S, Siegler JE, Kobeissi H, et al. Incidence and clinical outcomes of perforations during mechanical thrombectomy for medium vessel occlusion in acute ischemic stroke: a retrospective, multicenter, and multinational study. Eur Stroke J. 2024; 9:328–337.9. Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020; 51:2872–2884.10. Sarraj A, Sangha N, Hussain MS, Wisco D, Vora N, Elijovich L, et al. Endovascular therapy for acute ischemic stroke with occlusion of the middle cerebral artery M2 segment. JAMA Neurol. 2016; 73:1291–1296.
Article11. Dmytriw AA, Ghozy S, Salim HA, Musmar B, Siegler JE, Kobeissi H, et al. Assessment of thrombectomy versus combined thrombolysis and thrombectomy in patients with acute ischemic stroke and medium vessel occlusion. Radiology. 2024; 312:e233041.12. Siegler JE, Shaikh H, Khalife J, Oak S, Zhang L, Abdalkader M, et al. Aspiration versus stent-retriever as first-line endovascular therapy technique for primary medium and distal intracranial occlusions: a propensity-score matched multicenter analysis. Stroke Vasc Interv Neurol. 2023; 3:e000931.13. Salim H, Musmar B, Adeeb N, Yedavalli V, Lakhani D, Grewal SS, et al. Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke. Eur Stroke J. 2024; May. 10. [Epub]. Available from: https://doi.org/10.1177/23969873241249295.
Article14. Radu RA, Costalat V, Romoli M, Musmar B, Siegler JE, Ghozy S, et al. Outcomes with general anesthesia compared to conscious sedation for endovascular treatment of medium vessel occlusions: results of an international multicentric study. Clin Neuroradiol. 2024; Apr. 30. [Epub]. Available from: https://doi.org/10.1007/s00062-024-01415-1.
Article15. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019; 13(Suppl 1):S31–S34.
Article16. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007; 4:e296.17. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.18. Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010; 25:1–21.
Article19. Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983; 70:41–55.
Article20. Scheitz JF, Seiffge DJ, Tütüncü S, Gensicke H, Audebert HJ, Bonati LH, et al. Dose-related effects of statins on symptomatic intracerebral hemorrhage and outcome after thrombolysis for ischemic stroke. Stroke. 2014; 45:509–514.
Article21. Zinkstok SM, Engelter ST, Gensicke H, Lyrer PA, Ringleb PA, Artto V, et al. Safety of thrombolysis in stroke mimics: results from a multicenter cohort study. Stroke. 2013; 44:1080–1084.22. Engelter ST, Soinne L, Ringleb P, Sarikaya H, Bordet R, Berrouschot J, et al. IV thrombolysis and statins. Neurology. 2011; 77:888–895.
Article23. Rubin DB. Multiple imputation. In : van Buuren S, editor. Flexible imputation of missing data. 2nd ed. New York: Chapman and Hall/CRC;2018. p. 29–62.24. Goyal M, Ospel JM, Menon BK, Hill MD. MeVO: the next frontier? J Neurointerv Surg. 2020; 12:545–547.
Article25. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article26. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic Stroke. J Neurointerv Surg. 2023; 15:e8.27. Loh EW, Toh KZX, Kwok GYR, Teo YH, Teo YN, Goh C, et al. Endovascular therapy for acute ischemic stroke with distal medium vessel occlusion: a systematic review and meta-analysis. J Neurointerv Surg. 2023; 15:e452–e459.
Article28. Saber H, Desai SM, Haussen D, Al-Bayati A, Majidi S, Mocco J, et al. Endovascular therapy vs medical management for patients with acute stroke with medium vessel occlusion in the anterior circulation. JAMA Netw Open. 2022; 5:e2238154.
Article29. Grossberg JA, Rebello LC, Haussen DC, Bouslama M, Bowen M, Barreira CM, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke. 2018; 49:1662–1668.30. Rizzo F, Romoli M, Simonetti L, Gentile M, Forlivesi S, Piccolo L, et al. Reperfusion strategies in stroke with medium-to-distal vessel occlusion: a prospective observational study. Neurol Sci. 2024; 45:1129–1134.
Article31. Strambo D, Bartolini B, Beaud V, Marto JP, Sirimarco G, Dunet V, et al. Thrombectomy and thrombolysis of isolated posterior cerebral artery occlusion: cognitive, visual, and disability outcomes. Stroke. 2020; 51:254–261.32. Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg. 2018; 10:620–624.
Article33. Nogueira RG, Zaidat OO, Castonguay AC, Haussen DC, Martin CO, Holloway WE, et al. Rescue thrombectomy in large vessel occlusion strokes leads to better outcomes than intravenous thrombolysis alone: a ‘real world’ applicability of the recent trials. Interv Neurol. 2016; 5:101–110.
Article34. Sarraj A, Hassan A, Savitz SI, Grotta JC, Cai C, Parsha KN, et al. Endovascular thrombectomy for mild strokes: how low should we go? Stroke. 2018; 49:2398–2405.
Article35. Sarraj A, Grotta J, Albers GW, Hassan AE, Blackburn S, Day A, et al. Clinical and neuroimaging outcomes of direct thrombectomy vs bridging therapy in large vessel occlusion: analysis of the SELECT cohort study. Neurology. 2021; 96:e2839–e2853.36. Katsanos AH, Sarraj A, Froehler M, Purrucker J, Goyal N, Regenhardt RW, et al. IV thrombolysis initiated before transfer for endovascular stroke thrombectomy: a systematic review and meta-analysis. Neurology. 2023; 100:e1436–e1443.37. Khatri P, Kleindorfer DO, Devlin T, Sawyer RN Jr, Starr M, Mejilla J, et al. Effect of alteplase vs aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neurologic deficits: the PRISMS randomized clinical trial. JAMA. 2018; 320:156–166.
Article38. Chen HS, Cui Y, Zhou ZH, Zhang H, Wang LX, Wang WZ, et al. Dual antiplatelet therapy vs alteplase for patients with minor nondisabling acute ischemic stroke: the ARAMIS randomized clinical trial. JAMA. 2023; 329:2135–2144.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Cell free DNA: A Novel Predictor of Neurological Outcome after Intravenous Thrombolysis and/or Mechanical Thrombectomy in Acute Ischemic Stroke Patients
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series
- Differences in mechanical thrombectomy for acute ischemic stroke on weekdays versus nights/ weekends in a Japanese primary stroke core center
- Intravenous Thrombolysis Prior to Mechanical Thrombectomy in Acute Ischemic Stroke: Silver Bullet or Useless Bystander?