J Korean Neurosurg Soc.
2024 Sep;67(5):550-559. 10.3340/jkns.2023.0238.
A Comprehensive Analysis of Potential Complications after Oblique Lumbar Interbody Fusion : A Review of Postoperative Magnetic Resonance Scans in Over 400 Cases
- Affiliations
-
- 1Department of Neurosurgery, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Department of Neurosurgery, School of Medicine, Pusan National University, Yangsan, Korea
- KMID: 2558680
- DOI: http://doi.org/10.3340/jkns.2023.0238
Abstract
Objective
: This study focuses on identifying potential complications following oblique lumbar interbody fusion (OLIF) through routine magnetic resonance (MR) scans.
Methods
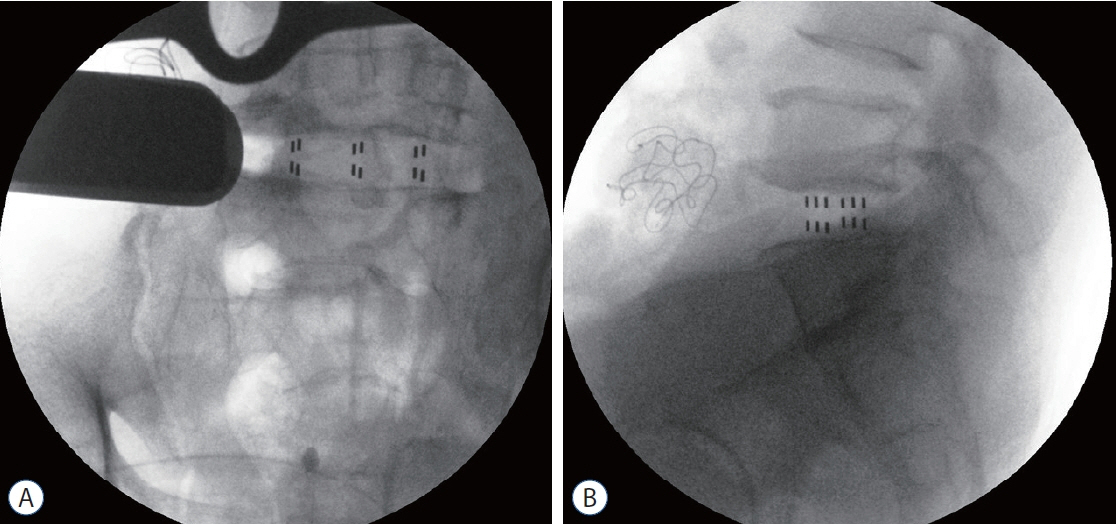
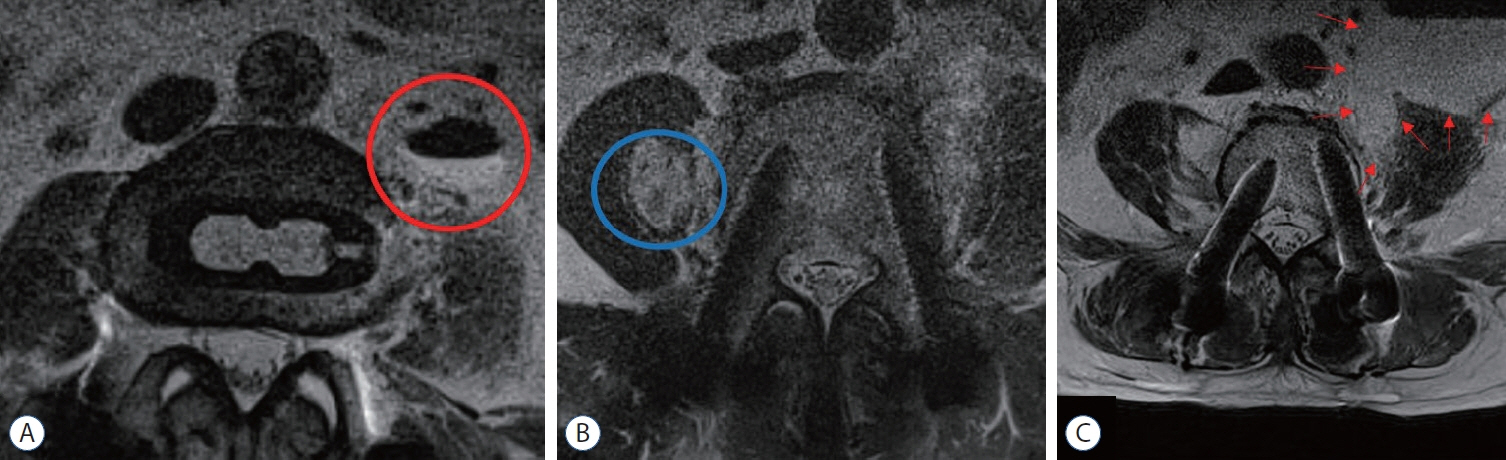
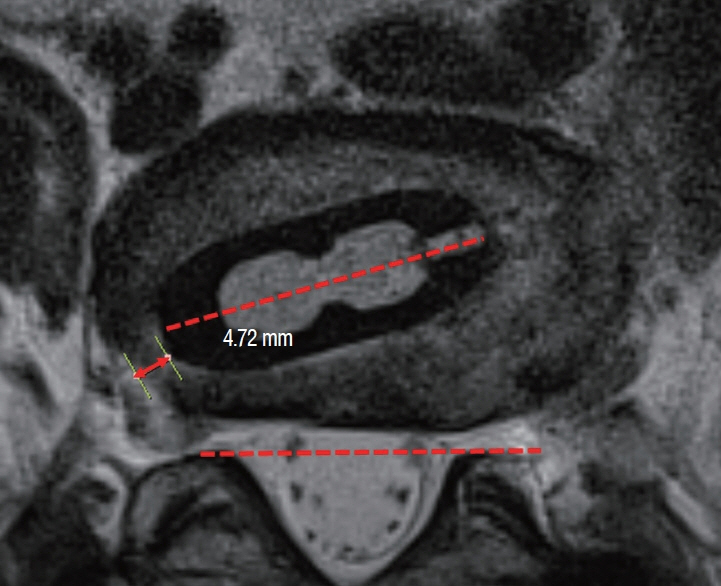
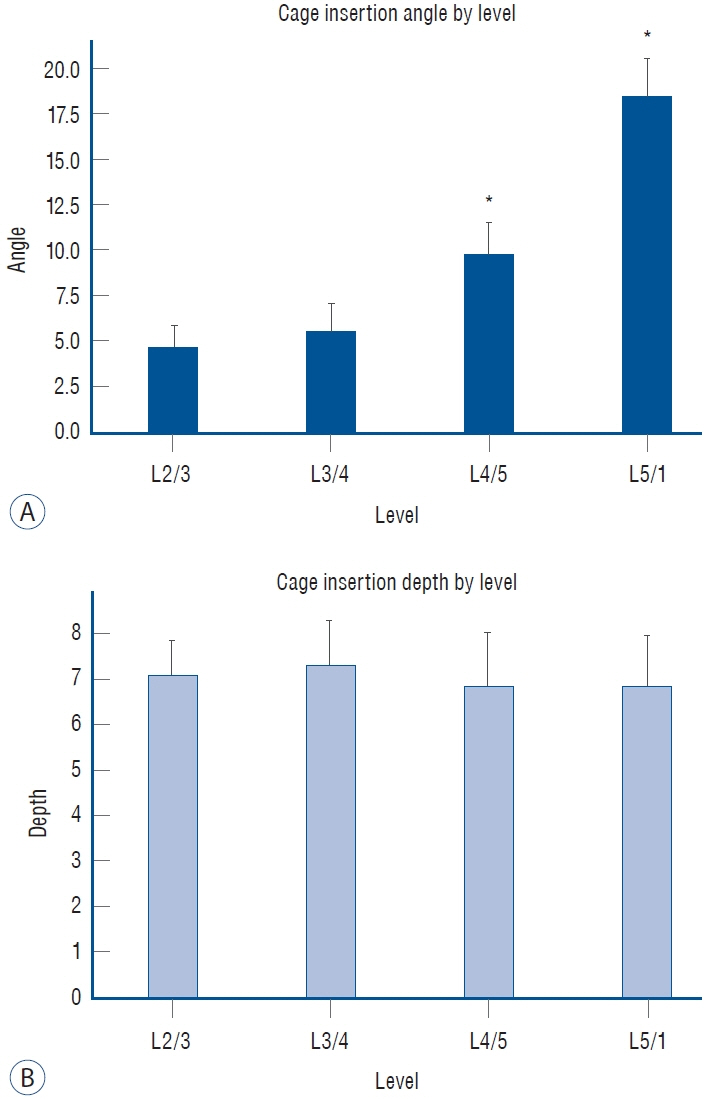
: From 650 patients who underwent OLIF from April 2018 to April 2022, this study included those with MR scans taken 1-week post-operatively, and only for indirect decompression patients. The analysis evaluated postoperative MR images for hematoma, cage insertion angles, and indirect decompression efficiency. Patient demographics, post-operatively symptoms, and complications were also evaluated.
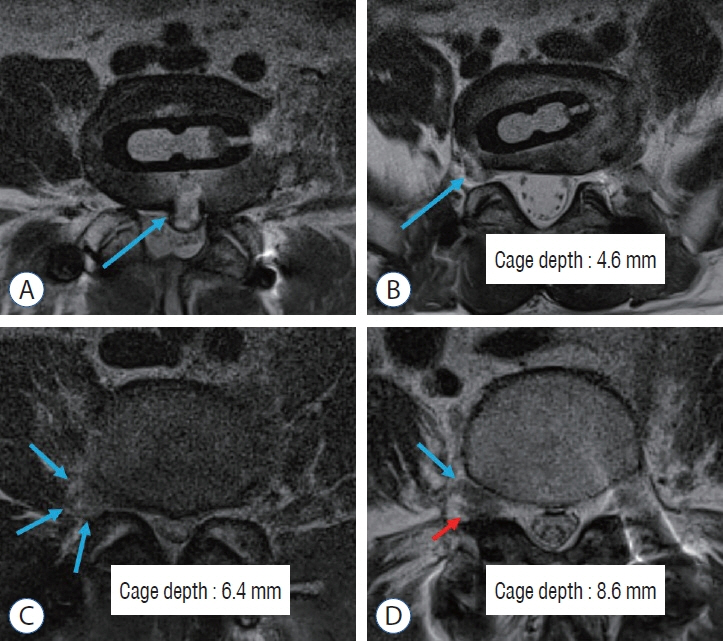
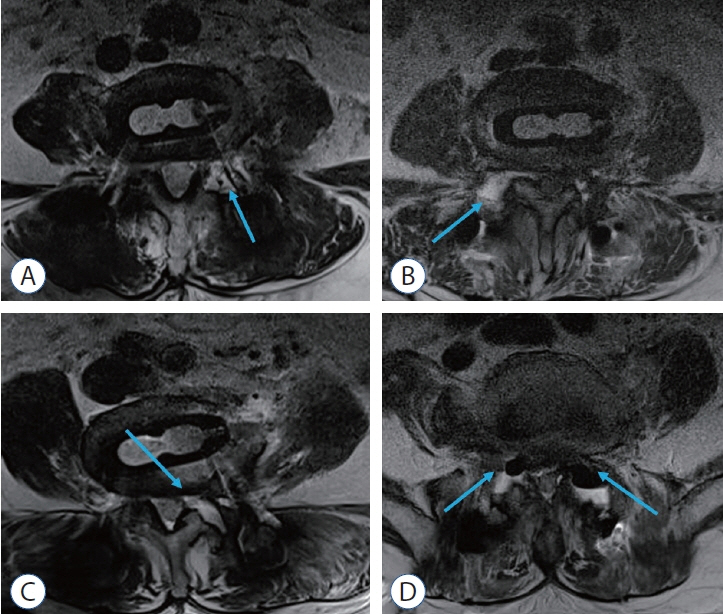
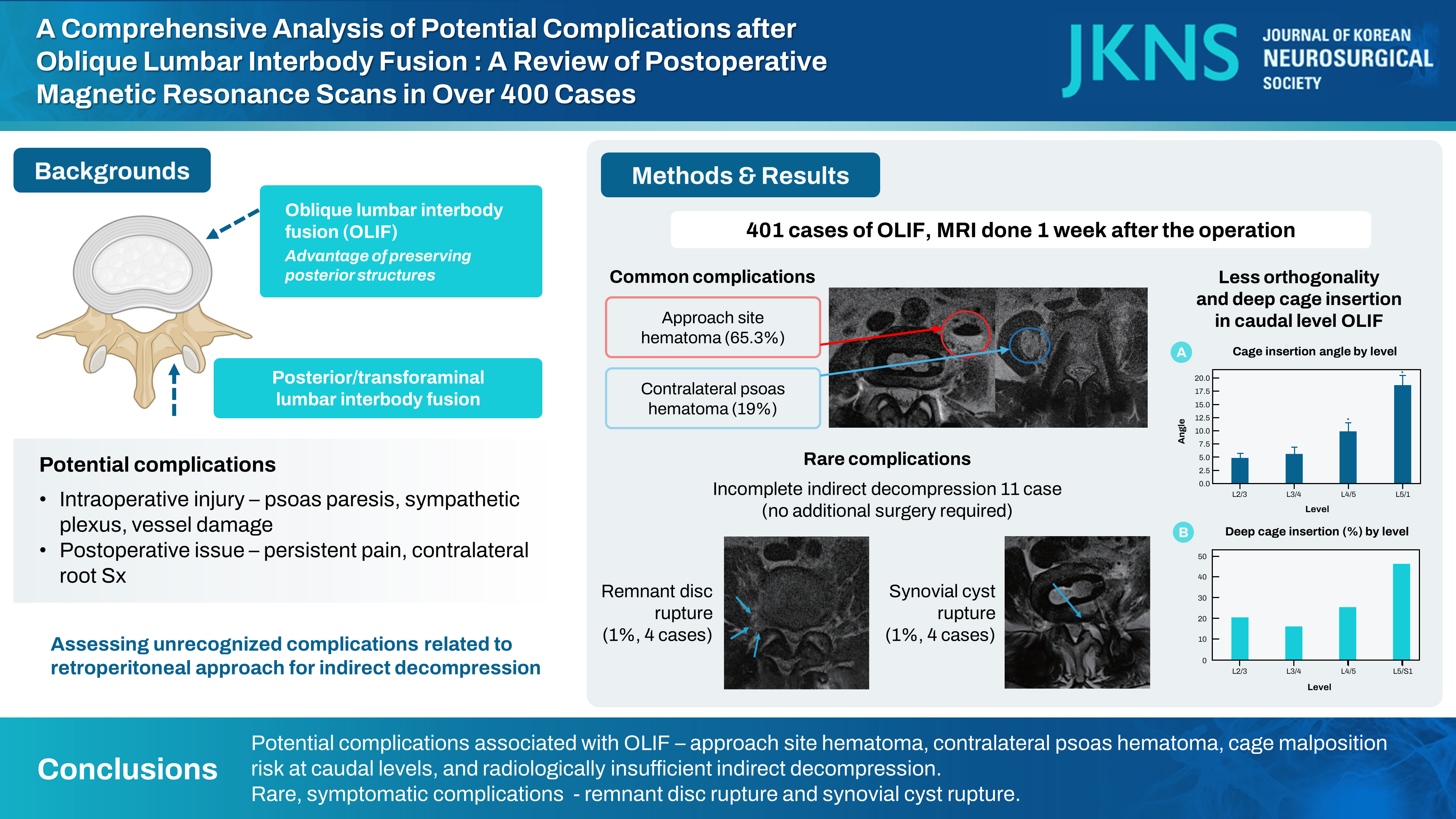
Results
: Out of 401 patients enrolled, most underwent 1- or 2-level OLIF. Common findings included approach site hematoma (65.3%) and contralateral psoas hematoma (19%). The caudal level OLIF was related with less orthogonality and deep insertion of cage. Incomplete indirect decompression occurred in 4.66% of cases but did not require additional surgery. Rare but symptomatic complications included remnant disc rupture (four cases, 1%) and synovial cyst rupture (four cases, 1%).
Conclusion
: This study has identified potential complications associated with OLIF, including approach site hematoma, contralateral psoas hematoma, cage malposition risk at caudal levels, and radiologically insufficient indirect decompression. Additionally, it highlights rare, yet symptomatic complications such as remnant disc rupture and synovial cyst rupture. These findings contribute insights into the relatively under-explored area of OLIF complications.
Keyword
Figure
Reference
-
References
1. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976). 42:55–62. 2017.
Article2. Beckman JM, Vincent B, Park MS, Billys JB, Isaacs RE, Pimenta L, et al. Contralateral psoas hematoma after minimally invasive, lateral retroperitoneal transpsoas lumbar interbody fusion: a multicenter review of 3950 lumbar levels. J Neurosurg Spine. 26:50–54. 2017.3. Chen W, Yang H, Jiang X, Fan S. The effect of oblique lumbar interbody fusion compared with transforaminal lumbar interbody fusion combined with enhanced recovery after surgery program on patients with lumbar degenerative disease at short-term follow-up. Biomed Res Int. 2021:5806066. 2021.
Article4. Chung NS, Lee HD, Jeon CH. Accuracy of the lateral cage placement under intraoperative C-arm fluoroscopy in oblique lateral interbody fusion. J Orthop Sci. 23:918–922. 2018.
Article5. Cui J, Guo X, Zheng Z, Liu H, Wang H, Li Z, et al. Perioperative complications in 255 patients who underwent lateral anterior lumbar interbody fusion (LaLIF) surgery. Eur Spine J. 30:2311–2322. 2021.
Article6. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 40:E175–E182. 2015.
Article7. Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, et al. Complications associated with lateral interbody fusion: nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine (Phila Pa 1976). 42:1478–1484. 2017.
Article8. Hattori S, Maeda T. Contralateral lower limb radiculopathy by extraforaminal disc herniation following oblique lumbar interbody fusion in degenerative lumbar disorder: illustrative cases. J Neurosurg Case Lessons. 5:CASE23198. 2023.9. Huang C, Xu Z, Li F, Chen Q. Does the access angle change the risk of approach-related complications in minimally invasive lateral lumbar interbody fusion? An MRI study. J Korean Neurosurg Soc. 61:707–715. 2018.
Article10. Hung SF, Liao JC, Tsai TT, Li YD, Chiu PY, Hsieh MK, et al. Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci Rep. 11:12783. 2021.
Article11. Ishii K, Isogai N, Shiono Y, Yoshida K, Takahashi Y, Takeshima K, et al. Contraindication of minimally invasive lateral interbody fusion for percutaneous reduction of degenerative spondylolisthesis: a new radiographic indicator of bony lateral recess stenosis using I line. Asian Spine J. 15:455–463. 2021.
Article12. Kim H, Chang BS, Chang SY. Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine. 19:163–176. 2022.
Article13. Kraiwattanapong C, Arnuntasupakul V, Kantawan R, Keorochana G, Lertudomphonwanit T, Sirijaturaporn P, et al. Malposition of cage in minimally invasive oblique lumbar interbody fusion. Case Rep Orthop. 2018:9142074. 2018.
Article14. Lee SH, Son DW, Bae SH, Lee JS, Kim YH, Sung SK, et al. Mini-open intercostal retroperitoneal approach for upper lumbar spine lateral interbody fusion. Neurospine. 20:553–563. 2023.15. Lee YS, Lee DH, Cho DC, Han I, Kim CH, Kwon HD, et al. The change of spinal canal according to oblique lumbar interbody fusion in degenerative spondylolisthesis: a prospective observational study. Neurospine. 19:492–500. 2022.
Article16. Liu Y, Kim JS, Chen CM, Choi G, Lee SH, Ruetten S, et al. A review of full-endoscopic interlaminar discectomy for lumbar disc disease: a historical and technical overview. J Minim Invasive Spine Surg Tech. 6(Suppl 1):S109–S116. 2021.
Article17. Mayer MH. A new microsurgical technique for minimally invasive anterior lumbar interbody fusion1996 scientific program committee. Spine (Phila Pa 1976). 22:691–699. discussion 700. 1997.
Article18. Oh BK, Son DW, Lee SH, Lee JS, Sung SK, Lee SW, et al. Learning curve and complications experience of oblique lateral interbody fusion : a single-center 143 consecutive cases. J Korean Neurosurg Soc. 64:447–459. 2021.
Article19. Oh JY, Seong JH, Kim JS, Park CK. Huge retroperitoneal hematoma following oblique lumbar interbody fusion. J Minim Invasive Spine Surg Tech. 2:32–34. 2017.
Article20. Papanastassiou ID, Eleraky M, Vrionis FD. Contralateral femoral nerve compression: an unrecognized complication after extreme lateral interbody fusion (XLIF). J Clin Neurosci. 18:149–151. 2011.
Article21. Parikh NP, Jhala AC. Contralateral lower limb radiculopathy following minimally invasive oblique lumbar interbody fusion in treatment of degenerative lumbar spine disease. J Minim Invasive Spine Surg Tech. 6:109–114. 2021.22. Quillo-Olvera J, Lin GX, Jo HJ, Kim JS. Complications on minimally invasive oblique lumbar interbody fusion at L2-L5 levels: a review of the literature and surgical strategies. Ann Transl Med. 6:101. 2018.
Article23. Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976). 35:1919–1924. 2010.
Article24. Shimizu T, Fujibayashi S, Otsuki B, Murata K, Matsuda S. Indirect decompression with lateral interbody fusion for severe degenerative lumbar spinal stenosis: minimum 1-year MRI follow-up. J Neurosurg Spine. 33:27–34. 2020.
Article25. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 6:89–97. 2012.
Article26. Son DW, Lee SH. Oblique Lumbar Interbody Fusion (OLIF). In : Ahn Y, Park JK, Park CK, editors. Core Techniques of Minimally Invasive Spine Surgery. Singapore: Springer;2023. p. 243–265.27. Woo JB, Son DW, Lee SH, Lee JS, Lee SW, Song GS. Which factor can predict the effect of indirect decompression using oblique lumbar interbody fusion? Medicine (Baltimore). 101:e29948. 2022.
Article28. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 17:545–553. 2017.
Article29. Yingsakmongkol W, Jitpakdee K, Kerr S, Limthongkul W, Kotheeranurak V, Singhatanadgige W. Successful criteria for indirect decompression with lateral lumbar interbody fusion. Neurospine. 19:805–815. 2022.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pearls and Pitfalls of Oblique Lateral Interbody Fusion: A Comprehensive Narrative Review
- Morphometric Analysis of the Ureter with Respect to Lateral Lumbar Interbody Fusion Using Contrast-Enhanced Computed Tomography
- Oblique Posterior Interbody Fusion with Bone Plugs by Unilateral Approach for Treatment of Lumbar Instability: Technical Note
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Vertebral Body Fracture after Oblique Lumbar Interbody Fusion in 2 Patients: A Case Report