J Korean Orthop Assoc.
2019 Jun;54(3):203-210. 10.4055/jkoa.2019.54.3.203.
Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 2Department of Orthopedic Surgery and Spine Center, Soonchunhyang University Seoul Hospital, Seoul, Korea. jlee@schmc.ac.kr
- KMID: 2450139
- DOI: http://doi.org/10.4055/jkoa.2019.54.3.203
Abstract
- The aim of this review was to evaluate minimally invasive lateral lumbar interbody fusion on the latest update. Lumbar interbody fusion was introduced recently. This study performed, a literature review of the indications, clinical outcomes, fusion rate, and complications regarding recently highlighted minimally invasive lateral lumbar interbody fusion. The indications of lateral lumbar interbody fusion are similar to the conventional anterior and posterior interbody fusion in degenerative lumbar diseases. In particular, lateral lumbar interbody fusion is an effective minimally invasive surgery in spinal stenosis, degenerative spondylolisthesis, degenerative adult deformity, degenerative disc disease and adjacent segment disease. In addition, the clinical outcomes and fusion rates of lateral lumbar interbody fusion are similar compared to conventional lumbar fusion. On the other hand, non-specific complications including hip flexor weakness, nerve injury, vascular injury, visceral injury, cage subsidence and pseudohernia have been reported. Lateral lumbar interbody fusion is a very useful minimally invasive surgery because it has advantages over conventional anterior and posterior interbody fusion without many of the disadvantages. Nevertheless, nonspecific complications during lateral lumbar interbody fusion procedure remain a challenge to be improved.
MeSH Terms
Figure
Reference
-
References
1. Bertagnoli R, Vazquez RJ. The Anterolateral TransPsoatic Approach (ALPA): a new technique for implanting prosthetic disc-nucleus devices. J Spinal Disord Tech. 2003. 16:398–404.2. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006. 6:435–43.
Article3. Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976). 2010. 35:S331–7.
Article4. Pawar A, Hughes A, Girardi F, Sama A, Lebl D, Cammisa F. Lateral lumbar interbody fusion. Asian Spine J. 2015. 9:978–83.
Article5. Salzmann SN, Shue J, Hughes AP. Lateral lumbar interbody fusion-outcomes and complications. Curr Rev Musculoskelet Med. 2017. 10:539–46.
Article6. Yang Y, Zhang L, Dong J. . Intraoperative myelography in transpsoas lateral lumbar interbody fusion for degenerative lumbar spinal stenosis: a preliminary prospective study. Biomed Res Int. 2017. 2017. 3742182.
Article7. Pawar AY, Hughes AP, Sama AA, Girardi FP, Lebl DR, Cam-misa FP. A comparative study of lateral lumbar interbody fusion and posterior lumbar interbody fusion in degenerative lumbar spondylolisthesis. Asian Spine J. 2015. 9:668–74.
Article8. Goyal A, Kerezoudis P, Alvi MA, Goncalves S, Bydon M. Outcomes following minimally invasive lateral transpsoas interbody fusion for degenerative low grade lumbar spondylolisthesis: a systematic review. Clin Neurol Neurosurg. 2018. 167:122–8.
Article9. Dakwar E, Cardona RF, Smith DA, Uribe JS. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010. 28:E8.
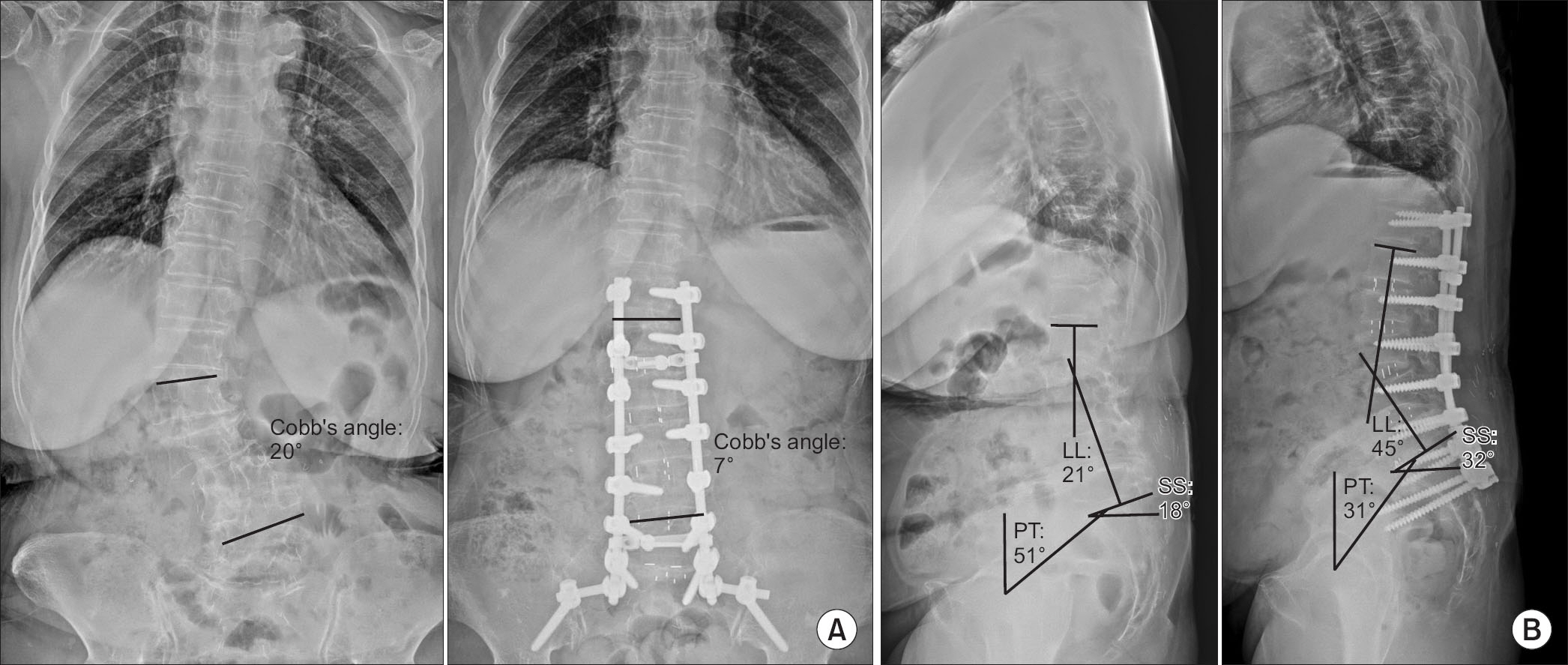
Article10. Acosta FL, Liu J, Slimack N, Moller D, Fessler R, Koski T. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine. 2011. 15:92–6.
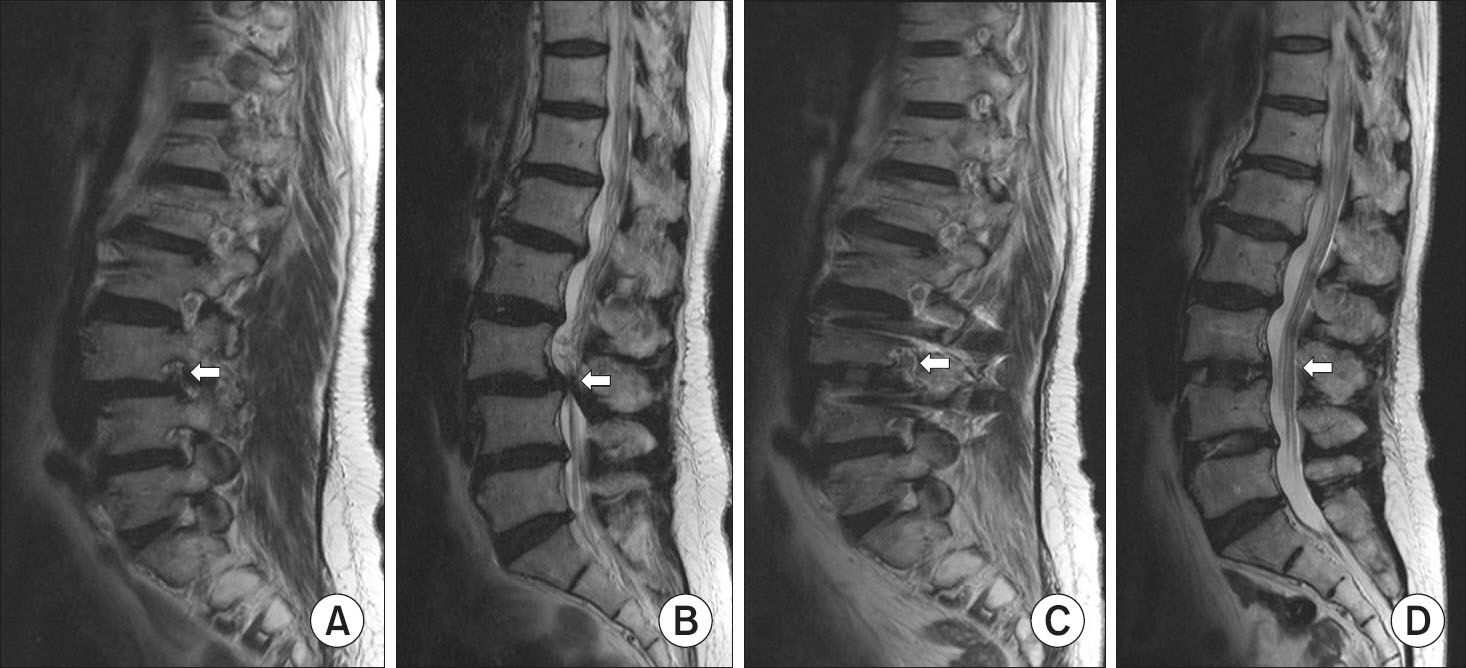
Article11. Park HY, Ha KY, Kim YH. . Minimally invasive lateral lumbar interbody fusion for adult spinal deformity: clinical and radiological efficacy with minimum two years follow-up. Spine (Phila Pa 1976). 2018. 43:E813–21.12. Mummaneni PV, Shaffrey CI, Lenke LG. . The minimally invasive spinal deformity surgery algorithm: a reproducible rational framework for decision making in minimally invasive spinal deformity surgery. Neurosurg Focus. 2014. 36:E6.
Article13. Louie PK, Varthi AG, Narain AS. . Stand-alone lateral lumbar interbody fusion for the treatment of symptomatic adjacent segment degeneration following previous lumbar fusion. Spine J. 2018. 18:2025–32.
Article14. Metzger MF, Robinson ST, Maldonado RC, Rawlinson J, Liu J, Acosta FL. Biomechanical analysis of lateral interbody fusion strategies for adjacent segment degeneration in the lumbar spine. Spine J. 2017. 17:1004–11.
Article15. Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976). 2011. 36:26–32.16. Kotwal S, Kawaguchi S, Lebl D. . Minimally invasive lateral lumbar interbody fusion: clinical and radiographic outcome at a minimum 2-year follow-up. J Spinal Disord Tech. 2015. 28:119–25.17. Malham GM, Parker RM, Blecher CM, Chow FY, Seex KA. Choice of approach does not affect clinical and radiologic outcomes: a comparative cohort of patients having anterior lumbar interbody fusion and patients having lateral lumbar interbody fusion at 24 months. Global Spine J. 2016. 6:472–81.
Article18. Keorochana G, Setrkraising K, Woratanarat P, Arirachakaran A, Kongtharvonskul J. Clinical outcomes after minimally invasive transforaminal lumbar interbody fusion and lateral lumbar interbody fusion for treatment of degenerative lumbar disease: a systematic review and meta-analysis. Neurosurg Rev. 2018. 41:755–70.
Article19. Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: influence of technique on fusion rate and clinical outcome. Spine (Phila Pa 1976). 2004. 29:455–63.20. Berjano P, Langella F, Damilano M. . Fusion rate following extreme lateral lumbar interbody fusion. Eur Spine J. 2015. 24 Suppl 3:369–71.
Article21. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013. 19:110–8.
Article22. Cappuccino A, Cornwall GB, Turner AW. . Biomechanical analysis and review of lateral lumbar fusion constructs. Spine (Phila Pa 1976). 2010. 35:S361–7.
Article23. Tohmeh AG, Rodgers WB, Peterson MD. Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine. 2011. 14:31–7.
Article24. Lee YP, Regev GJ, Chan J. . Evaluation of hip flexion strength following lateral lumbar interbody fusion. Spine J. 2013. 13:1259–62.
Article25. Lykissas MG, Aichmair A, Hughes AP. . Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J. 2014. 14:749–58.
Article26. Hijji FY, Narain AS, Bohl DD. . Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J. 2017. 17:1412–9.
Article27. Kueper J, Fantini GA, Walker BR, Aichmair A, Hughes AP. Incidence of vascular complications during lateral lumbar interbody fusion: an examination of the mini-open access technique. Eur Spine J. 2015. 24:800–9.
Article28. Al Maaieh MA, Du JY, Aichmair A. . Multivariate analysis on risk factors for postoperative ileus after lateral lumbar interbody fusion. Spine (Phila Pa 1976). 2014. 39:688–94.29. Le TV, Baaj AA, Dakwar E. . Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012. 37:1268–73.
Article30. Dakwar E, Le TV, Baaj AA. . Abdominal wall paresis as a complication of minimally invasive lateral transpsoas interbody fusion. Neurosurg Focus. 2011. 31:E18.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Surgical Technique and Review
- Pearls and Pitfalls of Oblique Lateral Interbody Fusion: A Comprehensive Narrative Review
- Lateral Lumbar Interbody Fusion
- Biportal Endoscopic Lumbar Interbody Fusion: Review of Current Evidence and the Literature
- Complications of Minimally Invasive Transforaminal Lumbar Interbody Fusion