J Korean Neurosurg Soc.
2023 Mar;66(2):155-161. 10.3340/jkns.2022.0079.
Morphometric Analysis of the Ureter with Respect to Lateral Lumbar Interbody Fusion Using Contrast-Enhanced Computed Tomography
- Affiliations
-
- 1Department of Orthopedics, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
- KMID: 2539876
- DOI: http://doi.org/10.3340/jkns.2022.0079
Abstract
Objective
: To analyze the anatomical location of the ureter in relation to lateral lumbar interbody fusion and evaluate the potential risk of ureteral injury.
Methods
: One hundred eight patients who performed contrast-enhanced computed tomographic scans were enrolled in this study. The location of the ureter from L2-L3 to L4-L5 was evaluated. The distances between the ureter and psoas muscle, intervertebral disc, and retroperitoneal vessels were also recorded bilaterally.
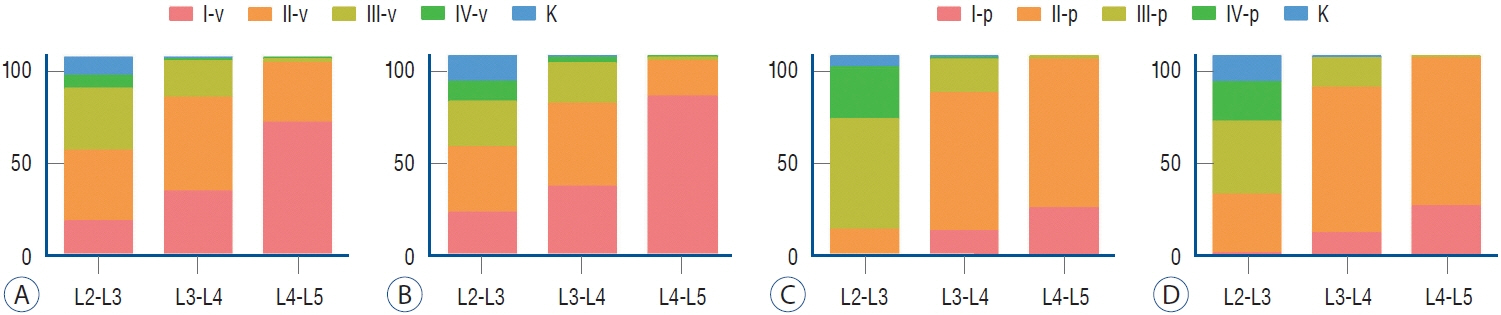
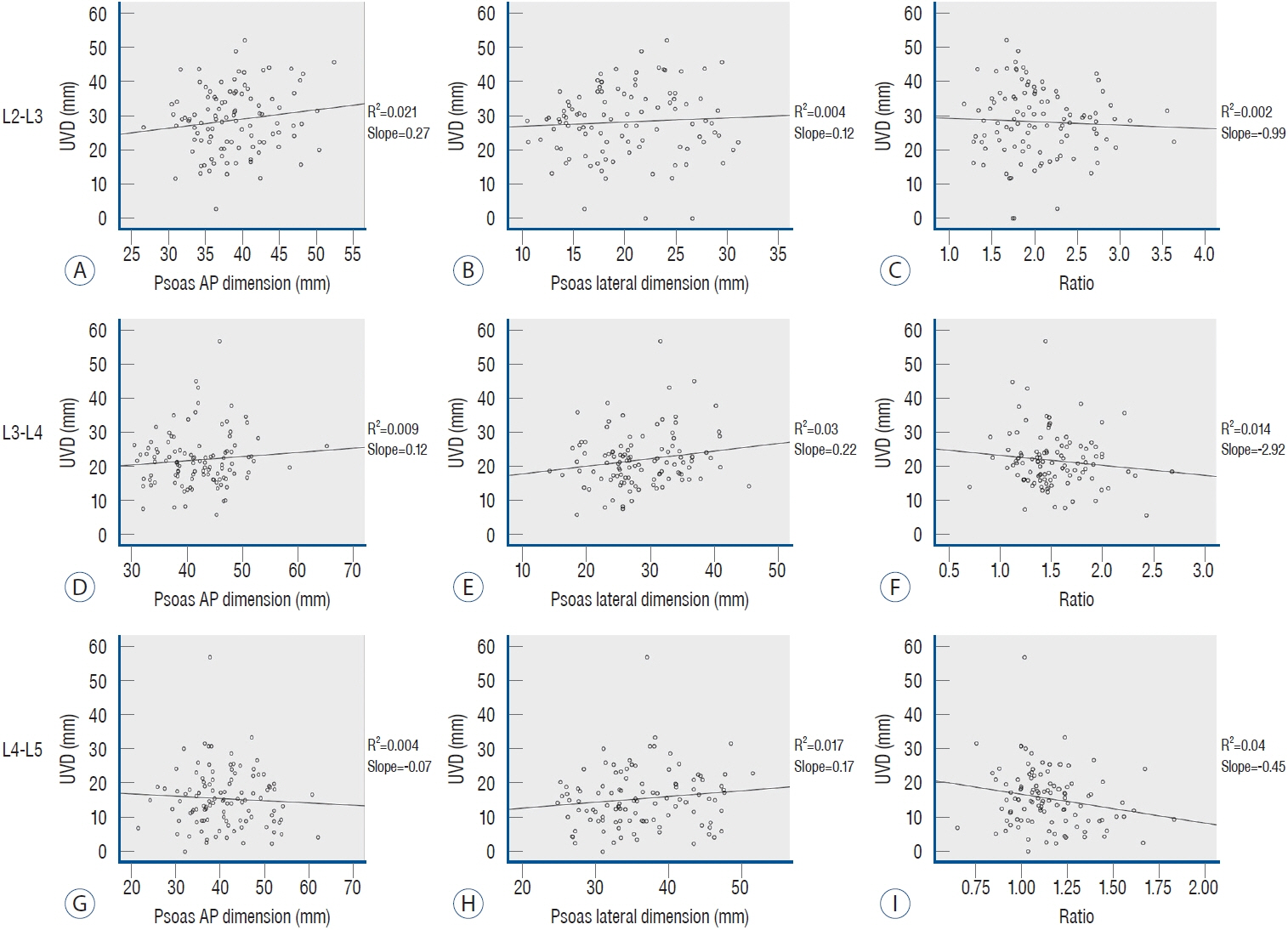
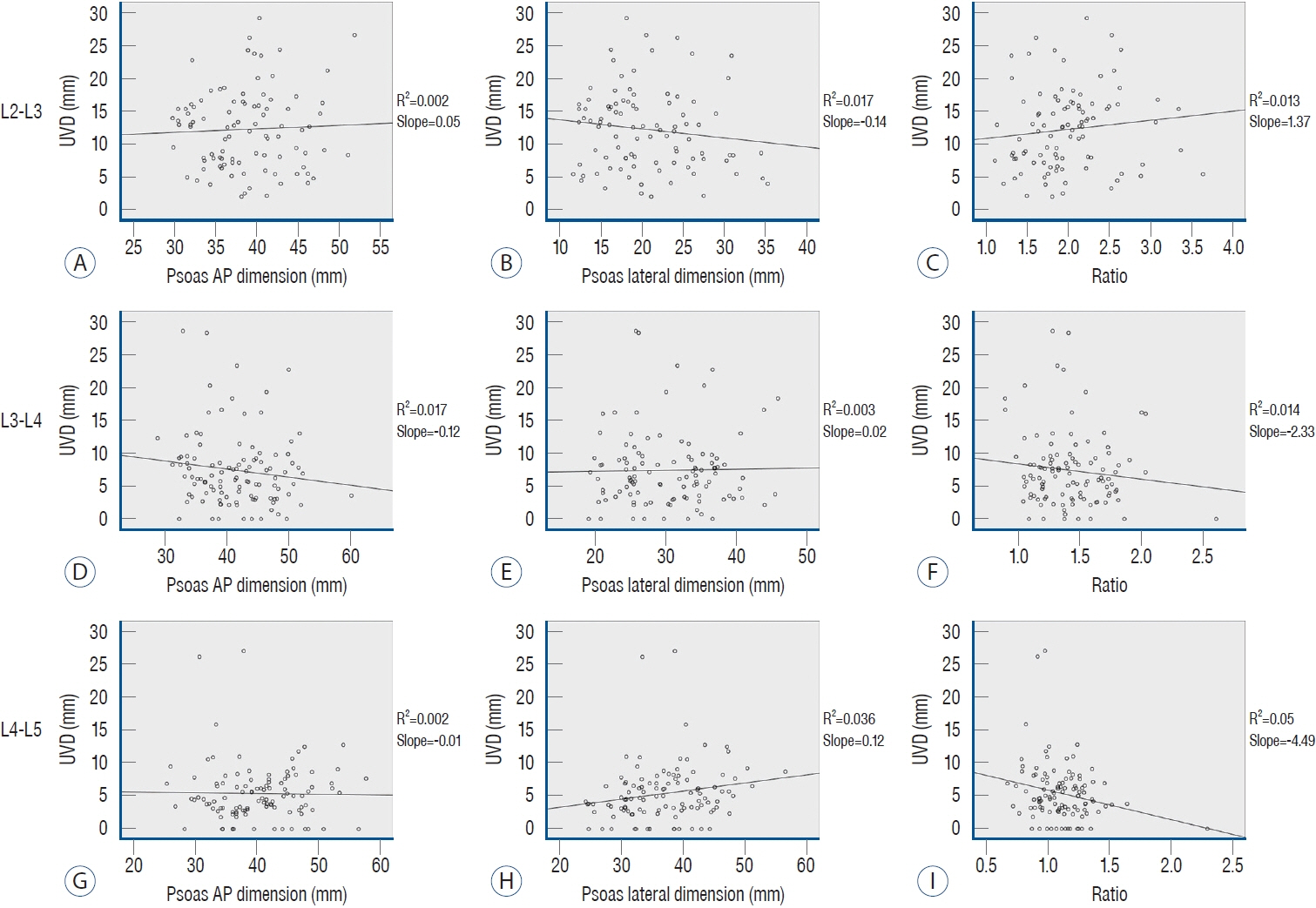
Results
: Over 30% of the ureters were close to the working corridor of extreme lumbar interbody fusion at L2-L3. Most of the ureters were close to working corridor of oblique lumbar interbody fusion, especially at L4-L5. The distance from the ureter to the great vessels on the left side was significantly narrowing from L2-L3 to L4-L5 (28.8±9.5 mm, 22.0±8.0 mm, 15.5±8.4 mm), and it was significantly larger than that on the right side (12.3±6.1 mm, 7.4±5.7 mm, 5.4±4.4 mm).
Conclusion
: Our findings indicate that the location of the ureter varies widely among individuals. To avoid unexpected damage to the ureter, it is imperative to directly visualize it and verify the ureter is not in the surgical pathway during lateral lumbar interbody fusion.
Keyword
Figure
Reference
-
References
1. Anand N, Baron EM. Urological injury as a complication of the transpsoas approach for discectomy and interbody fusion. J Neurosurg Spine. 18:18–23. 2013.2. Bjurlin MA, Rousseau LA, Vidal PP, Hollowell CM. Iatrogenic ureteral injury secondary to a thoracolumbar lateral revision instrumentation and fusion. Spine J. 9:e13–e15. 2009.3. Deukmedjian AR, Le TV, Dakwar E, Martinez CR, Uribe JS. Movement of abdominal structures on magnetic resonance imaging during positioning changes related to lateral lumbar spine surgery: a morphometric study: clinical article. J Neurosurg Spine. 16:615–623. 2012.4. Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, Nagashima H, et al. Complications associated with lateral interbody fusion: nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine (Phila Pa 1976). 42:1478–1484. 2017.5. Hijji FY, Narain AS, Bohl DD, Ahn J, Long WW, DiBattista JV, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J. 17:1412–1419. 2017.6. Krieg SM, Bobinski L, Albers L, Meyer B. Lateral lumbar interbody fusion without intraoperative neuromonitoring: a single-center consecutive series of 157 surgeries. J Neurosurg Spine. 30:1–7. 2019.7. Kubota G, Orita S, Umimura T, Takahashi K, Ohtori S. Insidious intraoperative ureteral injury as a complication in oblique lumbar interbody fusion surgery: a case report. BMC Res Notes. 10:193. 2017.8. Lee HJ, Kim JS, Ryu KS, Park CK. Ureter injury as a complication of oblique lumbar interbody fusion. World Neurosurg. 102:e7–e14. 2017.9. Makanji HS, Le H, Wood KB, Jenis LG, Cha TD. Morphometric analysis of the retroperitoneal vessels with respect to lateral access surgery in adult scoliosis. Clin Spine Surg. 30:E1010–E1014. 2017.10. Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res. 474:2020–2027. 2016.11. Ouchida J, Kanemura T, Satake K, Nakashima H, Segi N. Anatomic evaluation of retroperitoneal organs for lateral approach surgery: a prospective imaging study using computed tomography in the lateral decubitus position. Eur Spine J. 28:835–841. 2019.12. Regev GJ, Chen L, Dhawan M, Lee YP, Garfin SR, Kim CW. Morphometric analysis of the ventral nerve roots and retroperitoneal vessels with respect to the minimally invasive lateral approach in normal and deformed spines. Spine (Phila Pa 1976). 34:1330–1335. 2009.13. Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med. 6:104. 2018.14. Yoon SG, Kim MS, Kwon SC, Lyo IU, Sim HB. Delayed ureter stricture and kidney atrophy after oblique lumbar interbody fusion. World Neurosurg. 134:137–140. 2020.15. Yusof MI, Nadarajan E, Abdullah MS. The morphometric study of l3-L4 and L4-L5 lumbar spine in Asian population using magnetic resonance imaging: feasibility analysis for transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 39:E811–E816. 2014.16. Zhang F, Xu H, Yin B, Tao H, Yang S, Sun C, et al. Does right lateral decubitus position change retroperitoneal oblique corridor? A radiographic evaluation from L1 to L5. Eur Spine J. 26:646–650. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- The Changes of the Dimension of Intervertebral Disc,-Neural Foramen and Spinal Canal after Anterior Lumbar Interbody Fusion in the Lumbar Spine
- Pearls and Pitfalls of Oblique Lateral Interbody Fusion: A Comprehensive Narrative Review
- Lateral Lumbar Interbody Fusion
- Effect of the Pedicle Screw Fixation on the Anterior Lumbar Interbody Fusion Using the Freeze - Dried Structural Allograft