Ann Hepatobiliary Pancreat Surg.
2024 Aug;28(3):291-301. 10.14701/ahbps.24-038.
Evaluation of the impact of prospective payment systems on cholecystectomy: A systematic review and meta-analysis
- Affiliations
-
- 1Group Finance Analytics, Singapore Health Services, Singapore
- 2School of Economics, Singapore Management University, Singapore
- 3Department of Hepatopancreatobiliary and Transplant Surgery, Singapore General Hospital and National Cancer Centre Singapore, Singapore
- 4Duke-National University of Singapore Medical School, Singapore
- 5Liver Transplant Service, SingHealth Duke-National University of Singapore Transplant Centre, Singapore
- 6Finance, SingHealth Community Hospitals, Singapore
- 7Finance, Regional Health System & Strategic Finance, Singapore Health Services, Singapore
- KMID: 2558661
- DOI: http://doi.org/10.14701/ahbps.24-038
Abstract
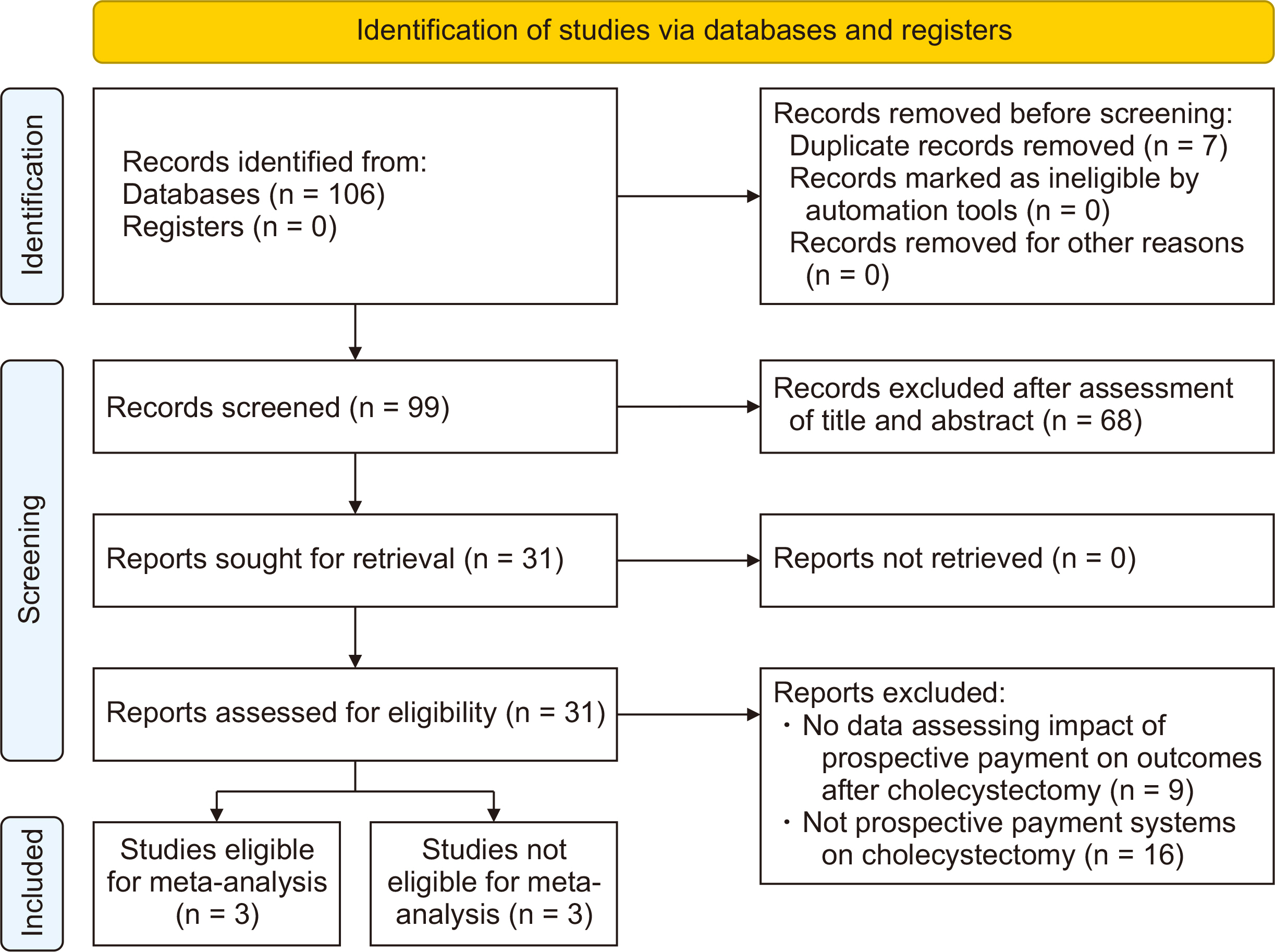
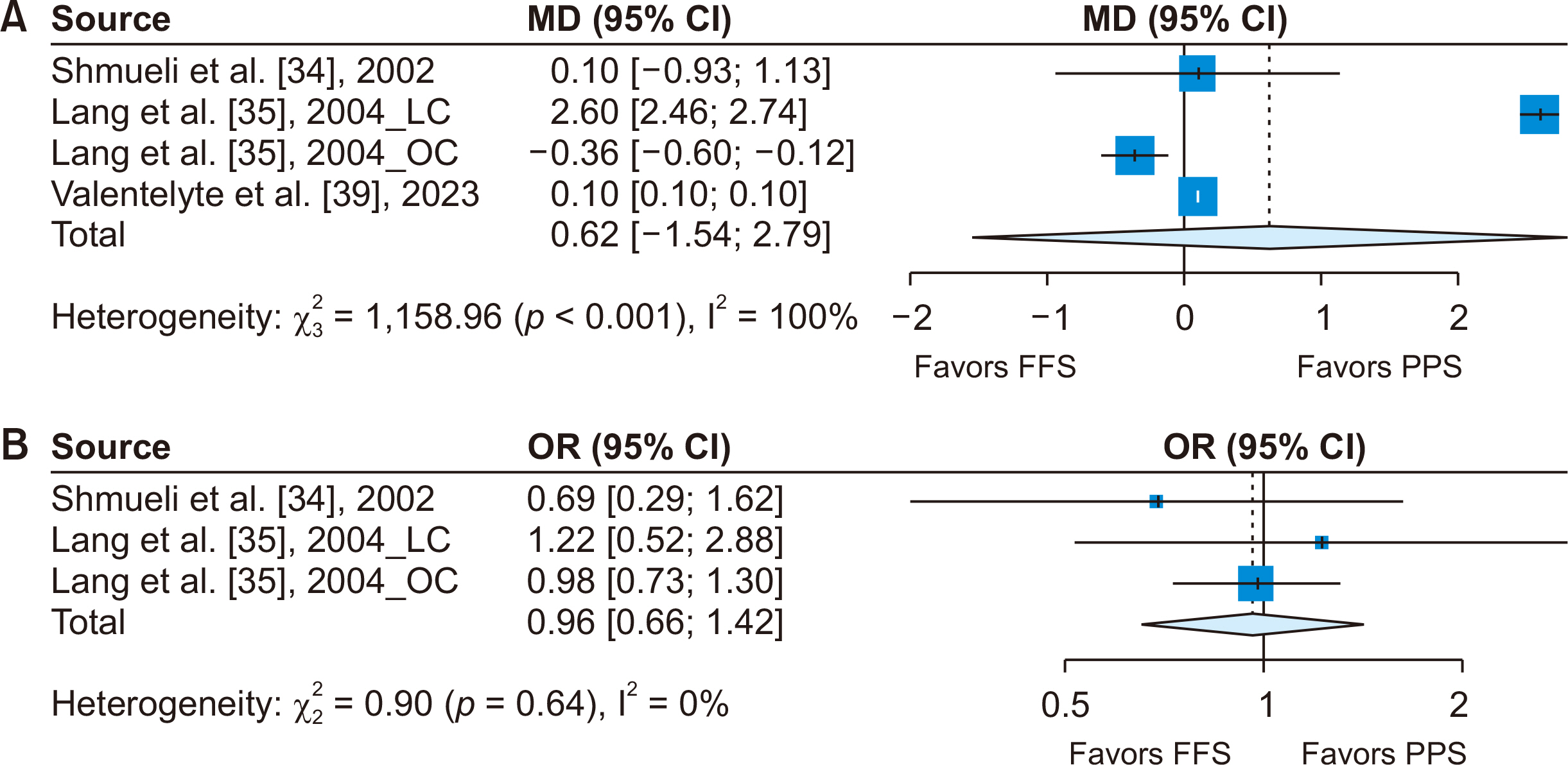
- This systematic review and meta-analysis aimed to evaluate the impact of prospective payment systems (PPSs) on cholecystectomy. A comprehensive literature review was conducted, examining studies published until December 2023. The review process focused on identifying research across major databases that reported critical outcomes such as length of stay (LOS), mortality, complications, admissions, readmissions, and costs following PPS for cholecystectomy. The studies were specifically selected for their relevance to the impact of PPS or the transition from fee-for-service (FFS) to PPS. The study analyzed six papers, with three eligible for meta-analysis, to assess the impact of the shift from FFS to PPS in laparoscopic and open cholecystectomy procedures. Our findings indicated no significant changes in LOS and mortality rates following the transition from FFS to PPS. Complication rates varied and were influenced by the diagnosis-related group categorization and surgeon cost profiles under episode-based payment. There was a slight increase in admissions and readmissions, and mixed effects on hospital costs and financial margins, suggesting varied responses to PPS for cholecystectomy procedures. The impact of PPS on cholecystectomy is nuanced and varies across different aspects of healthcare delivery. Our findings indicate a need for adaptable, patient-centered PPS models that balance economic efficiency with high-quality patient care. The study emphasizes the importance of considering specific surgical procedures and patient demographics in healthcare payment reforms.
Keyword
Figure
Reference
-
References
1. Jakovljevic M, Lamnisos D, Westerman R, Chattu VK, Cerda A. Future health spending forecast in leading emerging BRICS markets in 2030: health policy implications. Health Res Policy Syst. 2022; 20:23. DOI: 10.1186/s12961-022-00822-5. PMID: 35183217. PMCID: PMC8857747.2. Lorenzoni L, Marino A, Morgan D, James C. Health spending projections to 2030: new results based on a revised OECD methodology [Internet]. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/health-spending-projections-to-2030_5667f23d-en. OECD;2019. cited 2019 May 24.3. Carrin G, Hanvoravongchai P. 2003; Provider payments and patient charges as policy tools for cost-containment: how successful are they in high-income countries? Hum Resour Health. 1:6. DOI: 10.1186/1478-4491-1-6. PMID: 12914661. PMCID: PMC179884.4. Mayes R. 2007; The origins, development, and passage of Medicare’s revolutionary prospective payment system. J Hist Med Allied Sci. 62:21–55. DOI: 10.1093/jhmas/jrj038. PMID: 16467485.5. Jegers M, Kesteloot K, De Graeve D, Gilles W. 2002; A typology for provider payment systems in health care. Health policy. 60:255–273. DOI: 10.1016/S0168-8510(01)00216-0. PMID: 11965334.6. Ellis RP, Miller M. Carrin G, Buse K, Heggenhougen HK, Quah SR, editors. 2007. Provider payment methods and incentives. Health systems policy, finance, and organization. Academic Press;p. 322–328.7. Street A, Vitikainen K, Bjorvatn A, Hvenegaard A. Introducing activity-based financing: a review of experience in Australia, Denmark, Norway and Sweden [Internet]. Available from: https://eprints.whiterose.ac.uk/140285. Centre for Health Economics, University of York;2007. cited 2007 Nov 1.8. Glandon GL, Morrisey MA. 1986; Redefining the hospital-physician relationship under prospective payment. Inquiry. 23:166–175.9. Cattel D, Eijkenaar F, Schut FT. 2020; Value-based provider payment: towards a theoretically preferred design. Health Econ Policy Law. 15:94–112. DOI: 10.1017/S1744133118000397. PMID: 30259825.10. Health UDO, Services H. 1983; Medicare program; prospective payments for Medicare inpatient hospital services--HCFA. Interim final rule with comment period. Fed Regist. 48:39752–39890.11. Preston AM, Chua WF, Neu D. 1997; The diagnosis-related group-prospective payment system and the problem of the government of rationing health care to the elderly. Accounting, Organizations and Society. 22:147–164. DOI: 10.1016/S0361-3682(96)00011-6.12. Busse R, Geissler A, Aaviksoo A, Cots F, Häkkinen U, Kobel C, et al. 2013; Diagnosis related groups in Europe: moving towards transparency, efficiency, and quality in hospitals? BMJ. 346:f3197. DOI: 10.1136/bmj.f3197. PMID: 23747967.13. Hodgkin D, Mcguire TG. 1994; Payment levels and hospital response to prospective payment. J Health Econ. 13:1–29. DOI: 10.1016/0167-6296(94)90002-7. PMID: 10134436.14. Moreno-Serra R, Wagstaff A. 2010; System-wide impacts of hospital payment reforms: evidence from Central and Eastern Europe and Central Asia. J Health Econ. 29:585–602. DOI: 10.1016/j.jhealeco.2010.05.007. PMID: 20566226.15. Chulis GS. 1991; Assessing Medicare’s prospective payment system for hospitals. Med Care Rev. 48:167–206. DOI: 10.1177/002570879104800203. PMID: 10113662.16. Congress U. Office of Technology Assessment. Impacts of antibiotic-resistant bacteria. US Government Printing Office;Washington, DC: 1995. Sep. Report No.: OTA-H-629.17. Yin J, Lurås H, Hagen TP, Dahl FA. 2013; The effect of activity-based financing on hospital length of stay for elderly patients suffering from heart diseases in Norway. BMC Health Serv Res. 13:172. DOI: 10.1186/1472-6963-13-172. PMID: 23651910. PMCID: PMC3651263.18. Tan SS, Serdén L, Geissler A, van Ineveld M, Redekop K, Heurgren M, et al. Busse R, Geissler A, Quentin W, Wiley M, editors. 2011. DRGs and cost accounting: which is driving which. Diagnosis-related groups in Europe: moving towards transparency, efficiency and quality in hospitals. Open University Press and WHO Regional Office for Europe;p. 59–74.19. Schuetz P, Albrich WC, Suter I, Hug BL, Christ-Crain M, Holler T, et al. 2011; Quality of care delivered by fee-for-service and DRG hospitals in Switzerland in patients with community-acquired pneumonia. Swiss Med Wkly. 141:w13228. DOI: 10.4414/smw.2011.13228.20. Carroll NV, Erwin WG. 1990; Effect of the prospective-pricing system on drug use in Pennsylvania long-term-care facilities. Am J Hosp Pharm. 47:2251–2254. DOI: 10.1093/ajhp/47.10.2251.21. Qian X, Russell LB, Valiyeva E, Miller JE. 2011; "Quicker and sicker" under Medicare’s prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 63:1–27. DOI: 10.1111/j.1467-8586.2010.00369.x. PMID: 21141646.22. Sutherland JM. Reviewing the potential roles of financial incentives for funding healthcare in Canada: examen du rôle potentiel des incitations financières dans le financement des services de santé au Canada. desLibris;2012.23. Agresta F, Campanile FC, Vettoretto N, Silecchia G, Bergamini C, Maida P, et al. 2015; Laparoscopic cholecystectomy: consensus conference-based guidelines. Langenbecks Arch Surg. 400:429–453. DOI: 10.1007/s00423-015-1300-4. PMID: 25850631.24. Fletcher DR. 1995; Laparoscopic cholecystectomy: what national benefits have been achieved and at what cost? Med J Aust. 163:535–538. DOI: 10.5694/j.1326-5377.1995.tb124722.x. PMID: 8538525.25. Zhao JJ, Syn NL, Chong C, Tan HL, Ng JYX, Yap A, et al. 2021; Comparative outcomes of needlescopic, single-incision laparoscopic, standard laparoscopic, mini-laparotomy, and open cholecystectomy: a systematic review and network meta-analysis of 96 randomized controlled trials with 11,083 patients. Surgery. 170:994–1003. DOI: 10.1016/j.surg.2021.04.004. PMID: 34023139.26. Weiland DE, Caruso DM, Kassir A, Bay RC, Malone JM. 1997; Using delta/DRG diagrams and decision tree analysis to select a cost-effective surgery for cholecystitis. JSLS. 1:175–180.27. Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. 2021; The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 88:105906. DOI: 10.1016/j.ijsu.2021.105906. PMID: 33789826.28. Amir-Behghadami M, Janati A. 2020; Population, intervention, comparison, outcomes and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 37:387. DOI: 10.1136/emermed-2020-209567. PMID: 32253195.29. Luo D, Wan X, Liu J, Tong T. 2018; Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 27:1785–1805. DOI: 10.1177/0962280216669183. PMID: 27683581.30. Wan X, Wang W, Liu J, Tong T. 2014; Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 14:135. DOI: 10.1186/1471-2288-14-135. PMID: 25524443. PMCID: PMC4383202.31. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. 2016; ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 355:i4919. DOI: 10.1136/bmj.i4919. PMID: 27733354. PMCID: PMC5062054.32. Higgins JP, Thompson SG. 2002; Quantifying heterogeneity in a meta-analysis. Stat Med. 21:1539–1558. DOI: 10.1002/sim.1186. PMID: 12111919.33. Page MJ, Sterne JA, Higgins JP, Egger M. 2021; Investigating and dealing with publication bias and other reporting biases in meta-analyses of health research: a review. Res Synth Methods. 12:248–259. DOI: 10.1002/jrsm.1468. PMID: 33166064.34. Shmueli A, Intrator O, Israeli A. 2002; The effects of introducing prospective payments to general hospitals on length of stay, quality of care, and hospitals' income: the early experience of Israel. Soc Sci Med. 55:981–989. DOI: 10.1016/S0277-9536(01)00233-7. PMID: 12220098.35. Lang HC, Chi C, Liu CM. 2004; Impact of the case payment reimbursement method on the utilization and costs of laparoscopic cholecystectomy. Health Policy. 67:195–206. DOI: 10.1016/S0168-8510(03)00119-2. PMID: 14720637.36. Chen JL, Chernew ME, Fendrick AM, Thompson JW, Rose S. 2020; Impact of an episode-based payment initiative by commercial payers in Arkansas on procedure volume: an observational study. J Gen Intern Med. 35:578–585. DOI: 10.1007/s11606-019-05318-7. PMID: 31529377. PMCID: PMC7018907.37. Sheetz KH, Kenney B, Dupree JM, Campbell DA, Englesbe MJ. 2019; Targeting value-driven quality improvement for laparoscopic cholecystectomy in Michigan. Ann Surg. 269:127–132. DOI: 10.1097/SLA.0000000000002438. PMID: 28742681.38. Wu YT, Lin YN, Cheng CT, Fu CY, Liao CH, Hsieh CH. 2021; Diagnosis-related group (DRG)-based prospective hospital payment system can be well adopted for acute care surgery: Taiwanese experience with acute cholecystitis. World J Surg. 45:1080–1087. DOI: 10.1007/s00268-020-05904-5. PMID: 33454793.39. Valentelyte G, Keegan C, Sorensen J. 2023; Hospital response to Activity-Based Funding and price incentives: evidence from Ireland. Health Policy. 137:104915. DOI: 10.1016/j.healthpol.2023.104915. PMID: 37741112.40. Hadley J, Zuckerman S, Feder J. 1989; Profits and fiscal pressure in the prospective payment system: their impacts on hospitals. Inquiry. 354–365.41. Brügger U, Eichler K. Impact of introducing a DRG reimbursement system in an acute impatient hostpital setting: a literature review. In : HTAi 7th Annual Meeting; 2010 Jun 6-9; Dublin, Ireland.42. Palmer KS, Agoritsas T, Martin D, Scott T, Mulla SM, Miller AP, et al. 2014; Activity-based funding of hospitals and its impact on mortality, readmission, discharge destination, severity of illness, and volume of care: a systematic review and meta-analysis. PLoS One. 9:e109975. DOI: 10.1371/journal.pone.0109975. PMID: 25347697. PMCID: PMC4210200.43. Meng Z, Hui W, Cai Y, Liu J, Wu H. 2020; The effects of DRGs-based payment compared with cost-based payment on inpatient healthcare utilization: a systematic review and meta-analysis. Health Policy. 124:359–367. DOI: 10.1016/j.healthpol.2020.01.007. PMID: 32001043.44. Chen YJ, Zhang XY, Yan JQ, Xue-Tang , Qian MC, Ying XH. 2023; Impact of diagnosis-related groups on inpatient quality of health care: a systematic review and meta-analysis. Inquiry. 60:00469580231167011. DOI: 10.1177/00469580231167011. PMID: 37083281. PMCID: PMC10126696.45. Thommen D, Weissenberger N, Schuetz P, Mueller B, Reemts C, Holler T, et al. Head-to-head comparison of length of stay, patients' outcome and satisfaction in Switzerland before and after SwissDRG-Implementation in 2012 in 2012: an observational study in two tertiary university centers. Swiss Med Wkly. 2014; 144:w13972. DOI: 10.4414/smw.2014.13972. PMID: 24963880.46. Jian W, Lu M, Chan KY, Poon AN, Han W, Hu M, et al. 2015; Payment reform pilot in Beijing hospitals reduced expenditures and out-of-pocket payments per admission. Health Aff (Millwood). 34:1745–1752. DOI: 10.1377/hlthaff.2015.0074. PMID: 26438752.47. Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. 2001; Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 234:549–558. DOI: 10.1097/00000658-200110000-00014. PMID: 11573048. PMCID: PMC1422078.48. Pucci MJ, Brunt ML, Deziel DJ. 2016; Safety first, total cholecystectomy second. J Am Coll Surg. 223:543–544. DOI: 10.1016/j.jamcollsurg.2016.06.005. PMID: 27569667.49. Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. 2015; SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc. 29:3074–3085. DOI: 10.1007/s00464-015-4079-z. PMID: 25669635.50. Strasberg SM, Brunt ML. 2010; Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 211:132–138. DOI: 10.1016/j.jamcollsurg.2010.02.053. PMID: 20610259.51. Strasberg SM, Brunt LM. 2017; The critical view of safety: why it is not the only method of ductal identification within the standard of care in laparoscopic cholecystectomy. Ann Surg. 265:464–465. DOI: 10.1097/SLA.0000000000002054. PMID: 27763898.52. Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. 2005; Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 241:786–792. DOI: 10.1097/01.sla.0000161029.27410.71. PMID: 15849514. PMCID: PMC1357133.53. Dolan JP, Diggs BS, Sheppard BC, Hunter JG. 2009; The national mortality burden and significant factors associated with open and laparoscopic cholecystectomy: 1997-2006. J Gastrointest Surg. 13:2292–2301. DOI: 10.1007/s11605-009-0988-2. PMID: 19727976.54. Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Sys Rev. 2013; (6):CD005440. DOI: 10.1002/14651858.CD005440.pub3.55. Song GM, Bian W, Zeng XT, Zhou JG, Luo YQ, Tian X. 2016; Laparoscopic cholecystectomy for acute cholecystitis: early or delayed?: evidence from a systematic review of discordant meta-analyses. Medicine (Baltimore). 95:e3835. DOI: 10.1097/MD.0000000000003835. PMID: 27281088. PMCID: PMC4907666.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Introduction of the Systematic Review and Meta-Analysis
- Changes in the Mixed Fee-Based Payment System in Primary Care: Cases and Implications
- Systematic Review and Meta-analysis in Digestive Cancer Research
- Systematic Review and Meta-Analysis of Studies Evaluating Diagnostic Test Accuracy: A Practical Review for Clinical Researchers-Part I. General Guidance and Tips
- DRG-based Prospective Payment System on the View of Clinician