Ewha Med J.
2024 Apr;47(2):e29. 10.12771/emj.2024.e29.
Nontuberculous mycobacterial infection in a sporotricoid distribution in Korea: a case report
- Affiliations
-
- 1Department of Dermatology, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2556318
- DOI: http://doi.org/10.12771/emj.2024.e29
Abstract
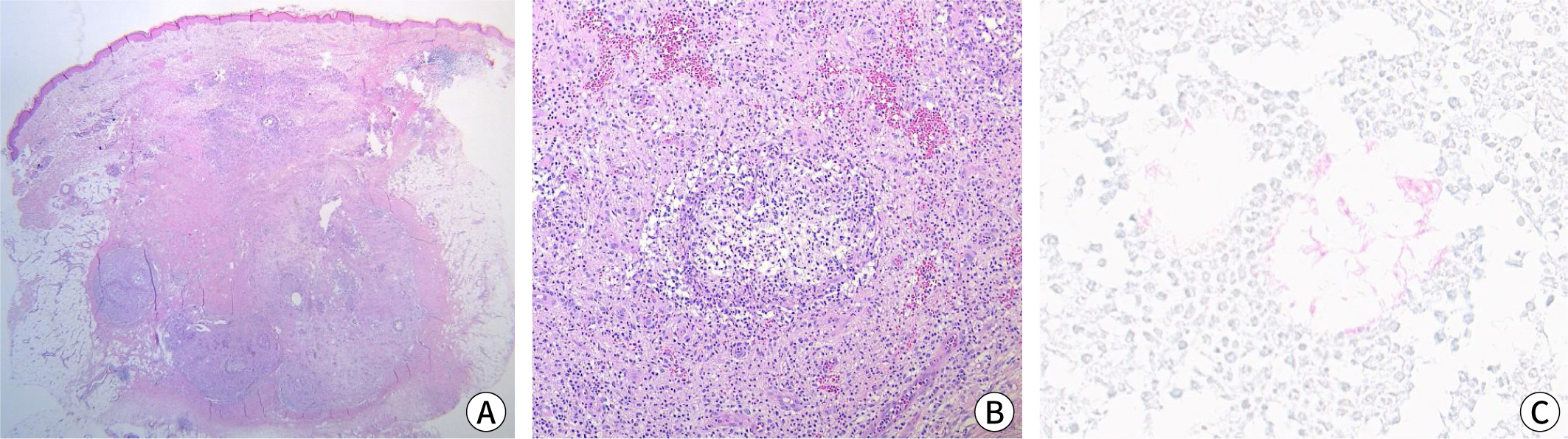
- Nontuberculous mycobacterial infections, which are often acquired from environmental sources such as water and soil, exhibit a variety of cutaneous manifestations that frequently lead to misdiagnoses and delays in treatment. A 77-year-old woman presented with multiple skin lesions in a sporotricoid distribution on her right leg, which persisted despite standard antibiotic treatments. Based on the skin biopsy, revealing granulomatous inflammation with acid-fast bacilli, and PCR testing, a nontuberculous mycobacterial infection was diagnosed. Antimycobacterial drug combinations, including clarithromycin, isoniazid, and rifampicin for 4 months, complete the skin lesion's clearance. This case underscores the need for heightened suspicion and the use of appropriate diagnostic techniques, including tissue biopsies and molecular methods such as PCR.
Keyword
Figure
Reference
-
References
1. Sethi A. Tuberculosis and infections with atypical mycobacteria. In. Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, editors. editors. Fitzpatrick’s dermatology in general medicine. 9th.ed. New York: McGraw-Hill;2019. p. p. 2870–2871.2. Jogi R, Tyring SK. Therapy of nontuberculous mycobacterial infections. Dermatol Ther. 2004; 17(6):491–498. DOI: 10.1111/j.1396-0296.2004.04051.x. PMID: 15571497.3. Gonzalez-Santiago TM, Drage LA. Nontuberculous mycobacteria: skin and soft tissue infections. Dermatol Clin. 2015; 33(3):563–577. DOI: 10.1016/j.det.2015.03.017. PMID: 26143432.4. Weedon D. Weedon’s skin pathology. 3rd ed. London: Churchill Livingstone;2010. p. p. 560.5. Franco-Paredes C, Marcos LA, Henao-Martínez AF, Rodríguez-Morales AJ, Villamil-Gómez WE, Gotuzzo E, et al. Cutaneous mycobacterial infections. Clin Microbiol Rev. 2018; 32(1):e00069-18. DOI: 10.1128/CMR.00069-18. PMID: 30429139. PMCID: PMC6302357.6. Palenque E. Skin disease and nontuberculous atypical mycobacteria. Int J Dermatol. 2000; 39(9):659–666. DOI: 10.1046/j.1365-4362.2000.00821.x. PMID: 11044189.7. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175(4):367–416. DOI: 10.1164/rccm.200604-571ST. PMID: 17277290.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Large Non Healing Ulcer: Non-Tuberculous Mycobacterial Infection of the Laryngopharynx
- Nontuberculous Mycobacterial Tenosynovitis in the Hand: Two Case Reports with the MR Imaging Findings
- Identification of Mycobacteria using High Performance Liquid Chromatography in Clinical Specimens
- A Case of Tenosynovitis Due to Mycobacterium intracellulare in a Patient with Rheumatoid Arthritis
- A Case of Nontuberculous Mycobacterium Infection Complicated by an Esophagomediastinal Fistula in a Human Immunodeficiency Virus Patient