J Stroke.
2024 May;26(2):300-311. 10.5853/jos.2024.00535.
Deep Learning-Based Automatic Classification of Ischemic Stroke Subtype Using Diffusion-Weighted Images
- Affiliations
-
- 1Department of Neurology, Dongguk University Ilsan Hospital, Goyang, Korea
- 2Artificial Intelligence Research Center, JLK Inc., Seoul, Korea
- 3Department of Neuroradiology and Imaging Physics, The University of Texas M.D. Anderson Cancer Center, Houston, TX, USA
- 4Department of Neurology, Korea University Guro Hospital, Seoul, Korea
- 5Department of Neurology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 6Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 8Department of Neurology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 9Department of Neurology, Dong-A University Hospital, Busan, Korea
- 10Department of Radiology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 11Department of Radiology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 12National Priority Research Center for Stroke, Goyang, Korea
- KMID: 2556050
- DOI: http://doi.org/10.5853/jos.2024.00535
Abstract
- Background and Purpose
Accurate classification of ischemic stroke subtype is important for effective secondary prevention of stroke. We used diffusion-weighted image (DWI) and atrial fibrillation (AF) data to train a deep learning algorithm to classify stroke subtype.
Methods
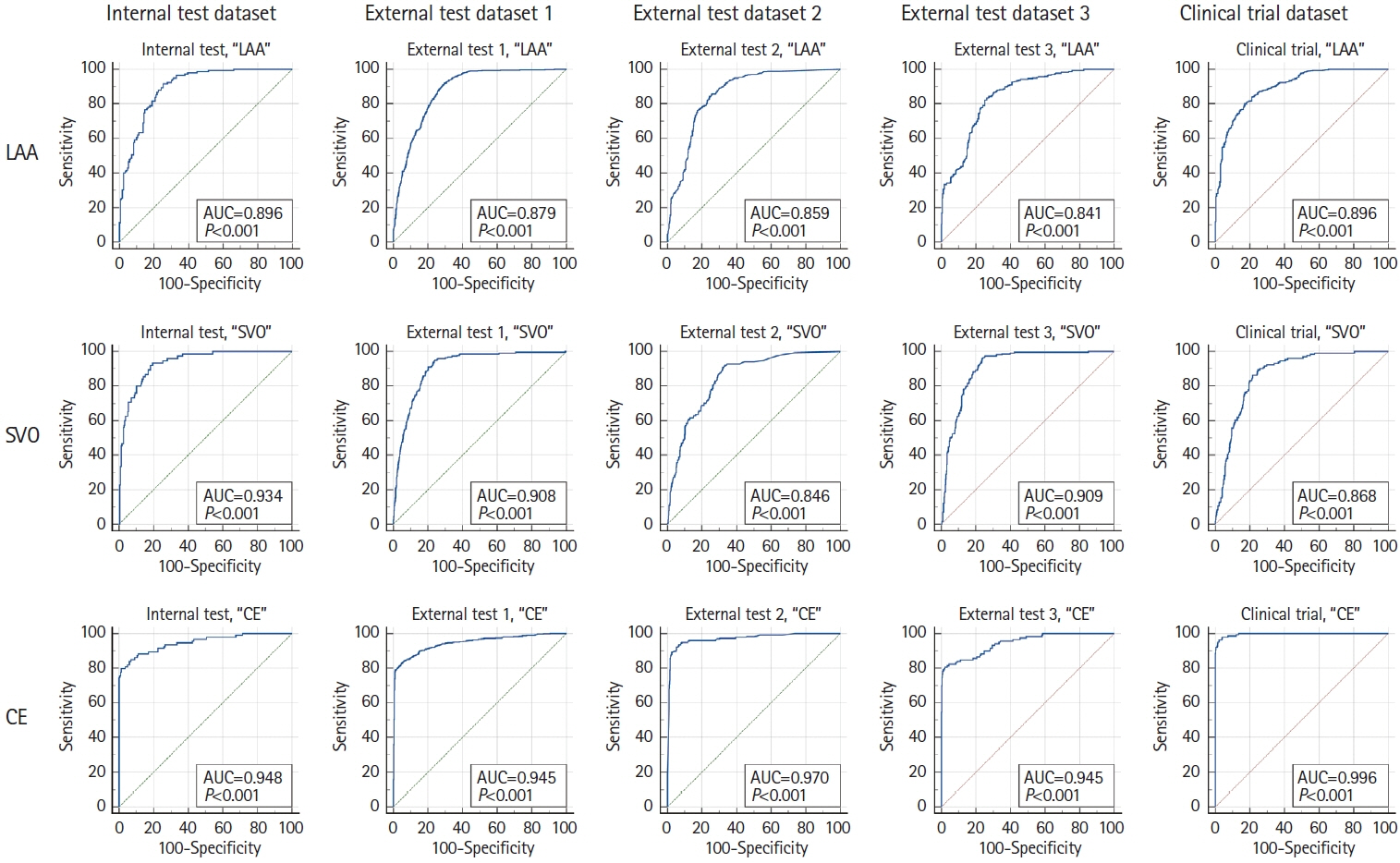
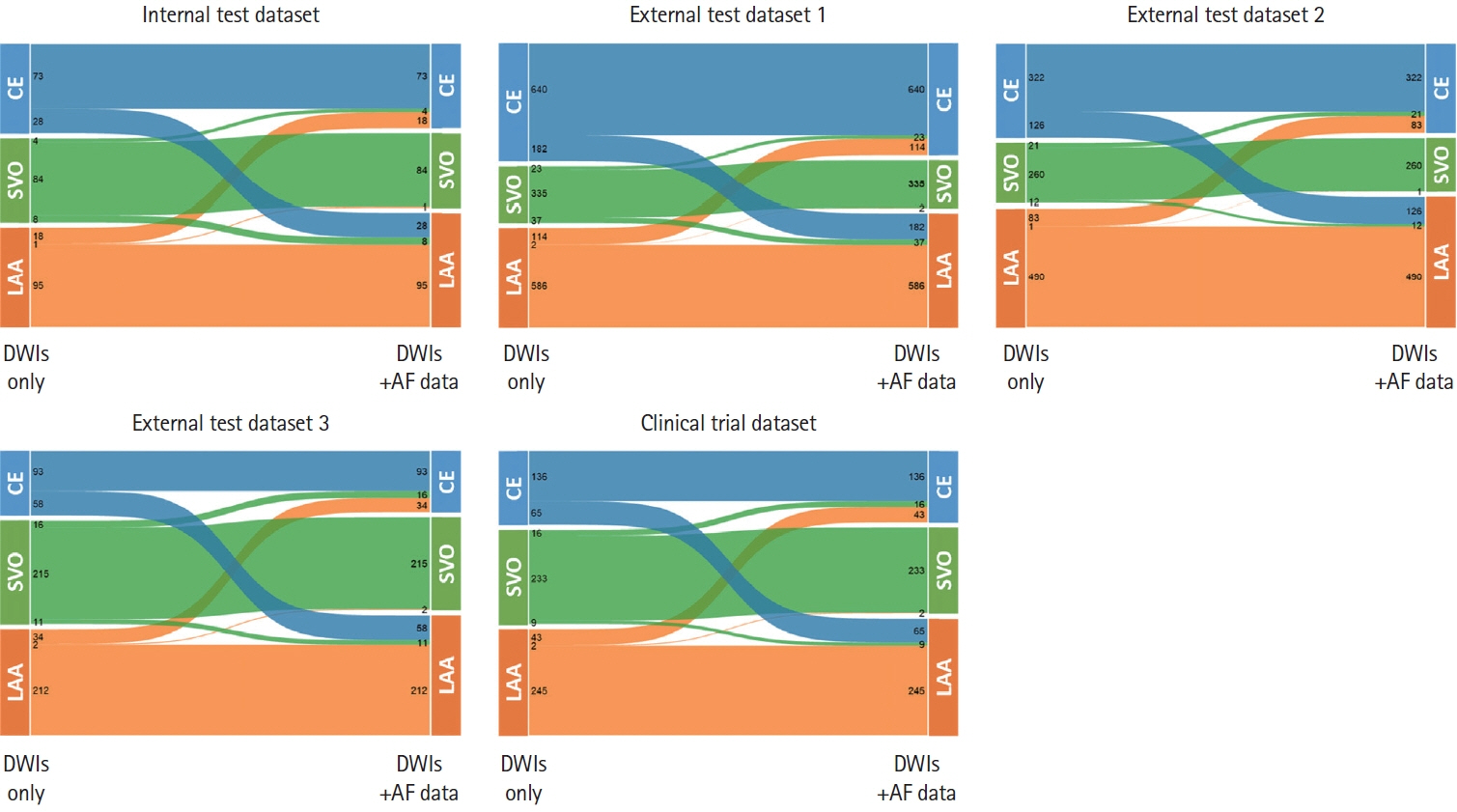
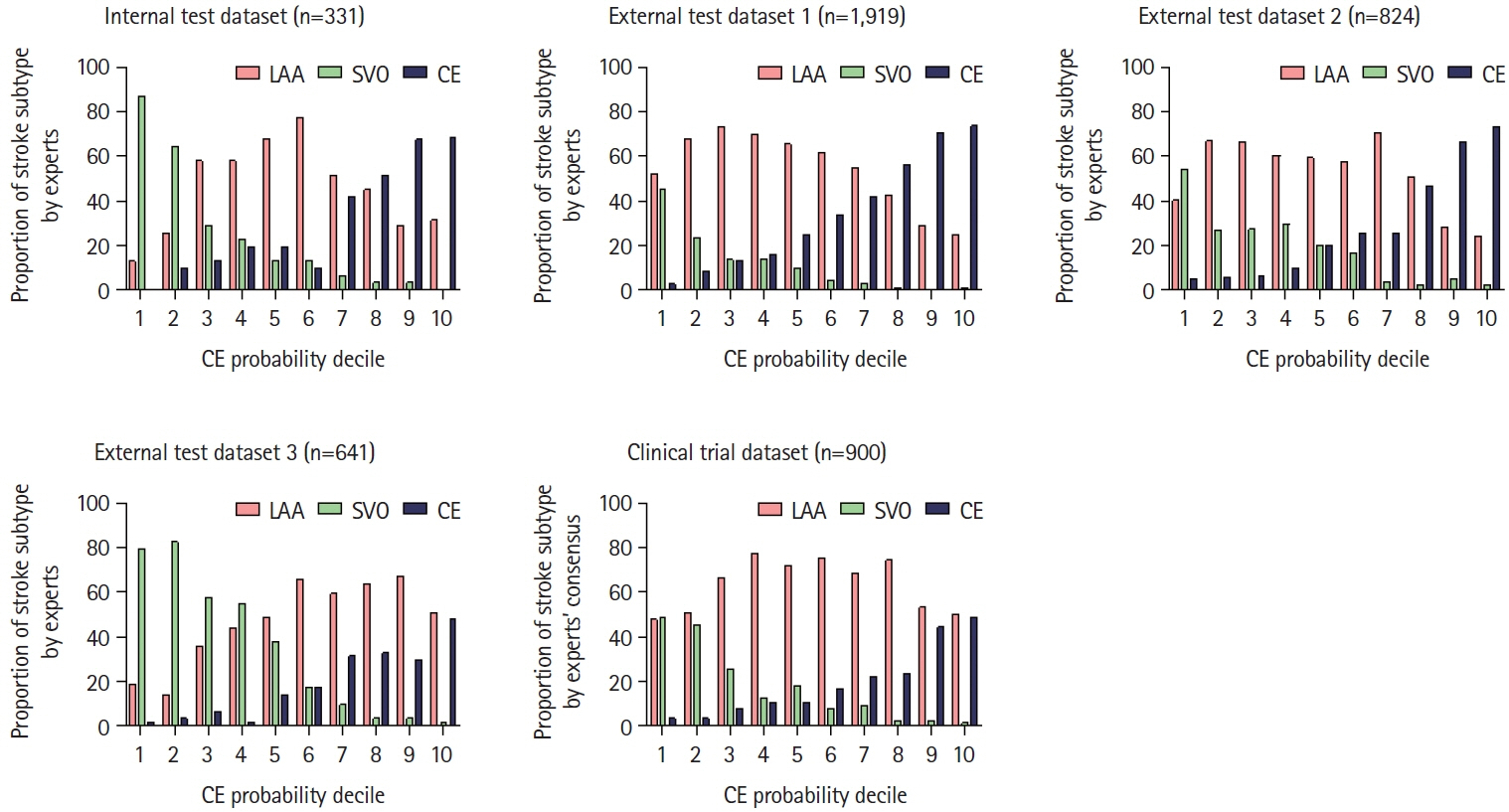
Model development was done in 2,988 patients with ischemic stroke from three centers by using U-net for infarct segmentation and EfficientNetV2 for subtype classification. Experienced neurologists (n=5) determined subtypes for external test datasets, while establishing a consensus for clinical trial datasets. Automatically segmented infarcts were fed into the model (DWI-only algorithm). Subsequently, another model was trained, with AF included as a categorical variable (DWI+AF algorithm). These models were tested: (1) internally against the opinion of the labeling experts, (2) against fresh external DWI data, and (3) against clinical trial dataset.
Results
In the training-and-validation datasets, the mean (±standard deviation) age was 68.0±12.5 (61.1% male). In internal testing, compared with the experts, the DWI-only and the DWI+AF algorithms respectively achieved moderate (65.3%) and near-strong (79.1%) agreement. In external testing, both algorithms again showed good agreements (59.3%–60.7% and 73.7%–74.0%, respectively). In the clinical trial dataset, compared with the expert consensus, percentage agreements and Cohen’s kappa were respectively 58.1% and 0.34 for the DWI-only vs. 72.9% and 0.57 for the DWI+AF algorithms. The corresponding values between experts were comparable (76.0% and 0.61) to the DWI+AF algorithm.
Conclusion
Our model trained on a large dataset of DWI (both with or without AF information) was able to classify ischemic stroke subtypes comparable to a consensus of stroke experts.
Keyword
Figure
Cited by 1 articles
-
Application of Artificial Intelligence in Acute Ischemic Stroke: A Scoping Review
JoonNyung Heo
Neurointervention. 2025;20(1):4-14. doi: 10.5469/neuroint.2025.00052.
Reference
-
References
1. Albers GW. Diffusion-weighted MRI for evaluation of acute stroke. Neurology. 1998; 51(3 Suppl 3):S47–S49.
Article2. Kang DW, Chalela JA, Ezzeddine MA, Warach S. Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol. 2003; 60:1730–1734.3. Chin YY, Sakinah H, Aryati A, Hassan BM. Prevalence, risk factors and secondary prevention of stroke recurrence in eight countries from South, East and Southeast Asia: a scoping review. Med J Malaysia. 2018; 73:90–99.4. Flach C, Muruet W, Wolfe CDA, Bhalla A, Douiri A. Risk and secondary prevention of stroke recurrence: a population-base cohort study. Stroke. 2020; 51:2435–2444.5. Ryu WS, Schellingerhout D, Hong KS, Jeong SW, Jang MU, Park MS, et al. White matter hyperintensity load on stroke recurrence and mortality at 1 year after ischemic stroke. Neurology. 2019; 93:e578–e589.
Article6. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article7. Ko Y, Lee S, Chung JW, Han MK, Park JM, Kang K, et al. MRI-based algorithm for acute ischemic stroke subtype classification. J Stroke. 2014; 16:161–172.8. Mamoli A, Censori B, Casto L, Sileo C, Cesana B, Camerlingo M. An analysis of the costs of ischemic stroke in an Italian stroke unit. Neurology. 1999; 53:112–116.
Article9. Jung WS, Seo KD, Suh SH. National trends in medical costs and prognosis of acute ischemic stroke patients in endovascular thrombectomy era: analysis using medical claim data in Korea. Neurointervention. 2022; 17:152–160.
Article10. Fang G, Xu P, Liu W. Automated ischemic stroke subtyping based on machine learning approach. IEEE Access. 2020; 8:18426–118432.
Article11. Zhang S, Wang J, Pei L, Liu K, Gao Y, Fang H, et al. Interpretable CNN for ischemic stroke subtype classification with active model adaptation. BMC Med Inform Decis Mak. 2022; 22:3.
Article12. Goldstein LB, Jones MR, Matchar DB, Edwards LJ, Hoff J, Chilukuri V, et al. Improving the reliability of stroke subgroup classification using the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) criteria. Stroke. 2001; 32:1091–1098.
Article13. Buck BH, Hill MD, Quinn FR, Butcher KS, Menon BK, Gulamhusein S, et al. Effect of implantable vs prolonged external electrocardiographic monitoring on atrial fibrillation detection in patients with ischemic stroke: the PER DIEM randomized clinical trial. JAMA. 2021; 325:2160–2168.
Article14. Sanna T, Diener HC, Passman RS, Di Lazzaro V, Bernstein RA, Morillo CA, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014; 370:2478–2486.
Article15. Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015; 17:38–53.
Article16. Noh YG, Ryu WS, Schellingerhout D, Park J, Chung J, Jeong SW, et al. Deep learning algorithms for automatic segmentation of acute cerebral infarcts on diffusion-weighted images: effects of training data sample size, transfer learning, and data features. medRxiv [Preprint]. 2023 [accessed July 2, 2023]. Available from: https://doi.org/10.1101/2023.07.02.23292150.
Article17. Ryu WS, Kang YR, Noh YG, Park JH, Kim D, Kim BC, et al. Acute infarct segmentation on diffusion-weighted imaging using deep learning algorithm and RAPID MRI. J Stroke. 2023; 25:425–429.18. Otsu N. A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern. 1979; 9:62–66.
Article19. Tan M, Le Q. EfficientNetV2: smaller models and faster training. In Lawrence N editor. Proceedings of Machine Learning Research. ICML 2021: Proceedings of the 38th International Conference on Machine Learning, 2021 Jul 18-24; Online. Norfolk, MA: Journal of Machine Learning Research; 2021. p. 10096-10106.20. He K, Zhang X, Ren S, Sun J. Deep residual learning for image recognition. Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR); 2016 Jun 27-30; Las Vegas, NV, USA. New York: IEEE; 2016. p.770-778.21. Howard AG, Zhu M, Chen B, Kalenichenko D, Wang W, Weyand T, et al. Mobilenets: efficient convolutional neural networks for mobile vision applications. arXiv [Preprint]. 2017 [accessed 2023 July 2]. Available from: https://arxiv.org/abs/1704.04861.22. Tan M, Le Q. EfficientNet: rethinking model scaling for convolutional neural networks. In Lawrence N editor. Proceedings of Machine Learning Research. ICML 2019: Proceedings of the 36th International Conference on Machine Learning, 2019 Jun 9-15; Long Beach, CA. Norfolk, MA: Journal of Machine Learning Research; 2019. p. 6105-6114.23. De Bruijn B. Revisiting the area under the ROC. In: Moen A, Andersen SK, Aarts J, Hurlen P. User centred networked health care (volume 169). Amsterdam: IOS Press;2011. p. 532–536.24. Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985; 4:87–90.
Article25. Garg R, Oh E, Naidech A, Kording K, Prabhakaran S. Automating ischemic stroke subtype classification using machine learning and natural language processing. J Stroke Cerebrovasc Dis. 2019; 28:2045–2051.26. Kim BK, Park S, Han MK, Hong JH, Lee DI, Yum KS. Deep learning for prediction of mechanism in acute ischemic stroke using brain diffusion magnetic resonance image. J Neurocrit Care. 2023; 16:85–93.
Article27. Cheng B, Knaack C, Forkert ND, Schnabel R, Gerloff C, Thomalla G. Stroke subtype classification by geometrical descriptors of lesion shape. PLoS One. 2017; 12:e0185063.
Article28. Kang DW, Kwon SU, Yoo SH, Kwon KY, Choi CG, Kim SJ, et al. Early recurrent ischemic lesions on diffusion-weighted imaging in symptomatic intracranial atherosclerosis. Arch Neurol. 2007; 64:50–54.
Article29. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/ American Stroke Association. Stroke. 2021; 52:e364–e467.30. Dawson J, Béjot Y, Christensen LM, De Marchis GM, Dichgans M, Hagberg G, et al. European Stroke Organisation (ESO) guideline on pharmacological interventions for long-term secondary prevention after ischaemic stroke or transient ischaemic attack. Eur Stroke J. 2022; 7:I–II.31. Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013; 382:507–515.
Article32. Jing J, Meng X, Zhao X, Liu L, Wang A, Pan Y, et al. Dual antiplatelet therapy in transient ischemic attack and minor stroke with different infarction patterns: subgroup analysis of the CHANCE randomized clinical trial. JAMA Neurol. 2018; 75:711–719.
Article33. Gao Y, Chen W, Pan Y, Jing J, Wang C, Johnston SC, et al. Dual antiplatelet treatment up to 72 hours after ischemic stroke. N Engl J Med. 2023; 389:2413–2424.
Article34. Lee M, Ovbiagele B, Saver JL. Intensive medical management to prevent large and small artery atherothrombotic stroke: time to expand the horizon. JAMA. 2021; 326:217–218.
Article35. Kim JS. Role of blood lipid levels and lipid-lowering therapy in stroke patients with different levels of cerebral artery diseases: reconsidering recent stroke guidelines. J Stroke. 2021; 23:149–161.
Article36. Sharma M, Cornelius VR, Patel JP, Davies JG, Molokhia M. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: systematic review and meta-analysis. Circulation. 2015; 132:194–204.
Article37. Hart RG, Catanese L, Perera KS, Ntaios G, Connolly SJ. Embolic stroke of undetermined source: a systematic review and clinical update. Stroke. 2017; 48:867–872.38. Poli S, Keller T, Martus P, Poli K, Ziemann U, Geisler T. The ATTICUS randomized controlled trial-subgroup analyses. Stroke. 2023; 54(Suppl 1):A31.39. Hart RG, Sharma M, Mundl H, Kasner SE, Bangdiwala SI, Berkowitz SD, et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med. 2018; 378:2191–2201.
Article40. Diener HC, Sacco RL, Easton JD, Granger CB, Bernstein RA, Uchiyama S, et al. Dabigatran for prevention of stroke after embolic stroke of undetermined source. N Engl J Med. 2019; 380:1906–1917.
Article41. Kamel H, Navi BB, Parikh NS, Merkler AE, Okin PM, Devereux RB, et al. Machine learning prediction of stroke mechanism in embolic strokes of undetermined source. Stroke. 2020; 51:e203–e210.
Article42. Veltkamp R, Pearce LA, Korompoki E, Sharma M, Kasner SE, Toni D, et al. Characteristics of recurrent ischemic stroke after embolic stroke of undetermined source: secondary analysis of a randomized clinical trial. JAMA Neurol. 2020; 77:1233–1240.
Article43. Kim AS, Kamel H, Bernstein RA, Manchanda M, Caprio FZ. Controversies in stroke: should patients with embolic stroke of undetermined source undergo intensive heart rhythm monitoring with an implantable loop recorder? Stroke. 2022; 53:3243–3247.
Article44. Hong KS. Non-vitamin K antagonist oral anticoagulants in medical conditions at high risk of thromboembolism beyond atrial fibrillation. J Stroke. 2019; 21:259–275.
Article45. Liu Z, Gu H, Wei M, Feng X, Yu F, Feng J, et al. Comparison between healthcare quality in primary stroke centers and comprehensive stroke centers for acute stroke patients: evidence from the Chinese Stroke Center Alliance. Lancet Reg Health West Pac. 2023; 38:100863.46. Kim J, Cho S, Lee H, Lee JY. [Nationwide acute stroke care quality and disparity in Korea: focusing on the type of healthcare facilities and the socioeconomic status of patients]. Public Health Aff. 2021; 5:e6. Korean.
Article47. Lee LJ, Kidwell CS, Alger J, Starkman S, Saver JL. Impact on stroke subtype diagnosis of early diffusion-weighted magnetic resonance imaging and magnetic resonance angiography. Stroke. 2000; 31:1081–1089.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deep learning for prediction of mechanism in acute ischemic stroke using brain diffusion magnetic resonance image
- Mechanisms of Recurrence in Subtypes of Ischemic Stroke: A Hospital-based Follow-up Study
- Exploiting the Vulnerability of Deep Learning-Based Artificial Intelligence Models in Medical Imaging: Adversarial Attacks
- The Usefulness of Diffusion: Weighted Magnetic Resonance Image in the Diagnosis of Neonatal Seizure
- Automatic Diagnosis of Attention Deficit Hyperactivity Disorder with Continuous Wavelet Transform and Convolutional Neural Network