Acute Crit Care.
2024 Feb;39(1):70-77. 10.4266/acc.2023.00654.
Prevalence of extracorporeal blood purification techniques in critically ill patients before and during the COVID-19 pandemic in Egypt
- Affiliations
-
- 1Department of Pediatrics, Faculty of Medicine, Cairo University, Cairo, Egypt
- 2Pediatric Intensive Care Unit, Cairo University Children Hospital, Cairo, Egypt
- KMID: 2555225
- DOI: http://doi.org/10.4266/acc.2023.00654
Abstract
- Background
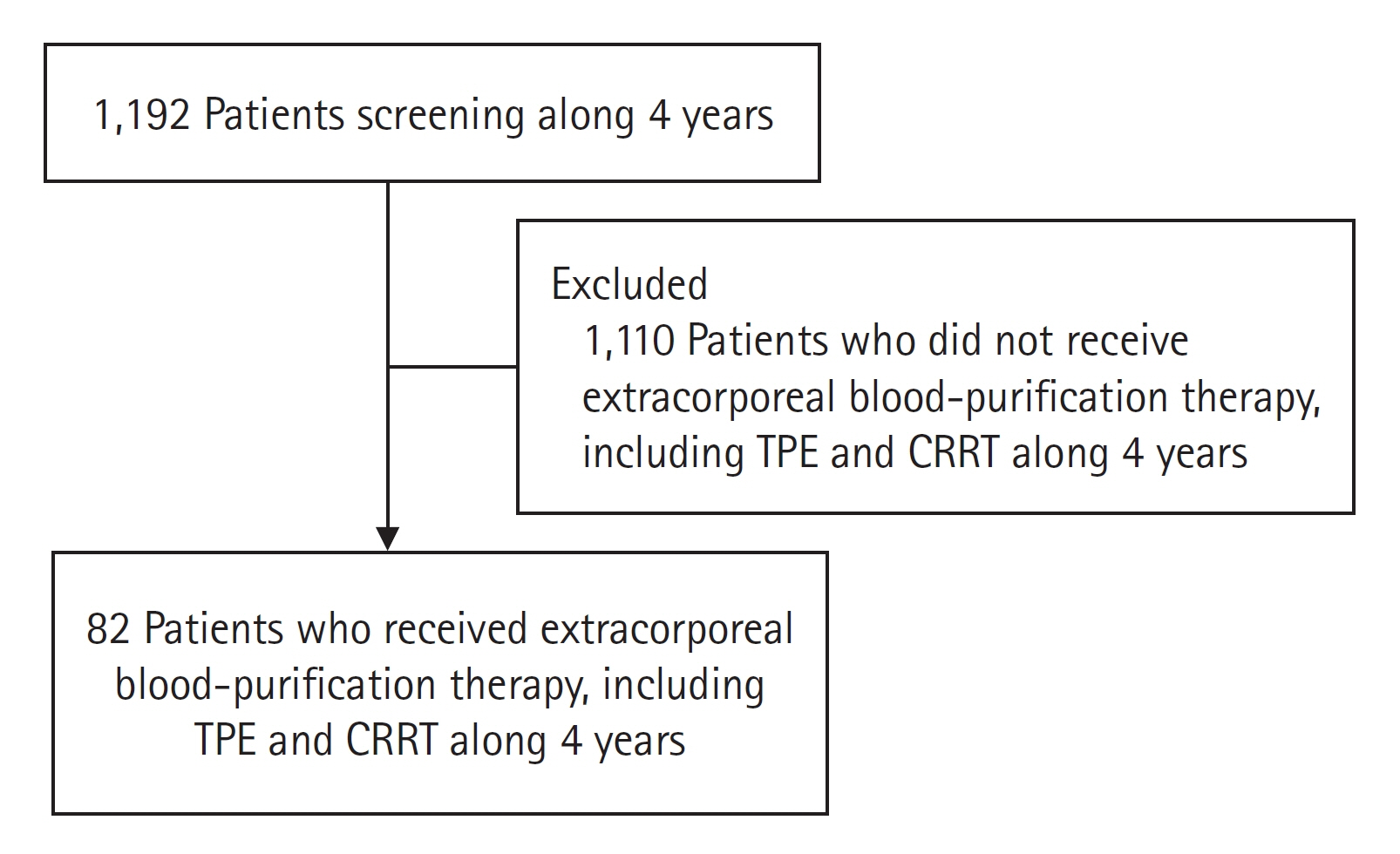
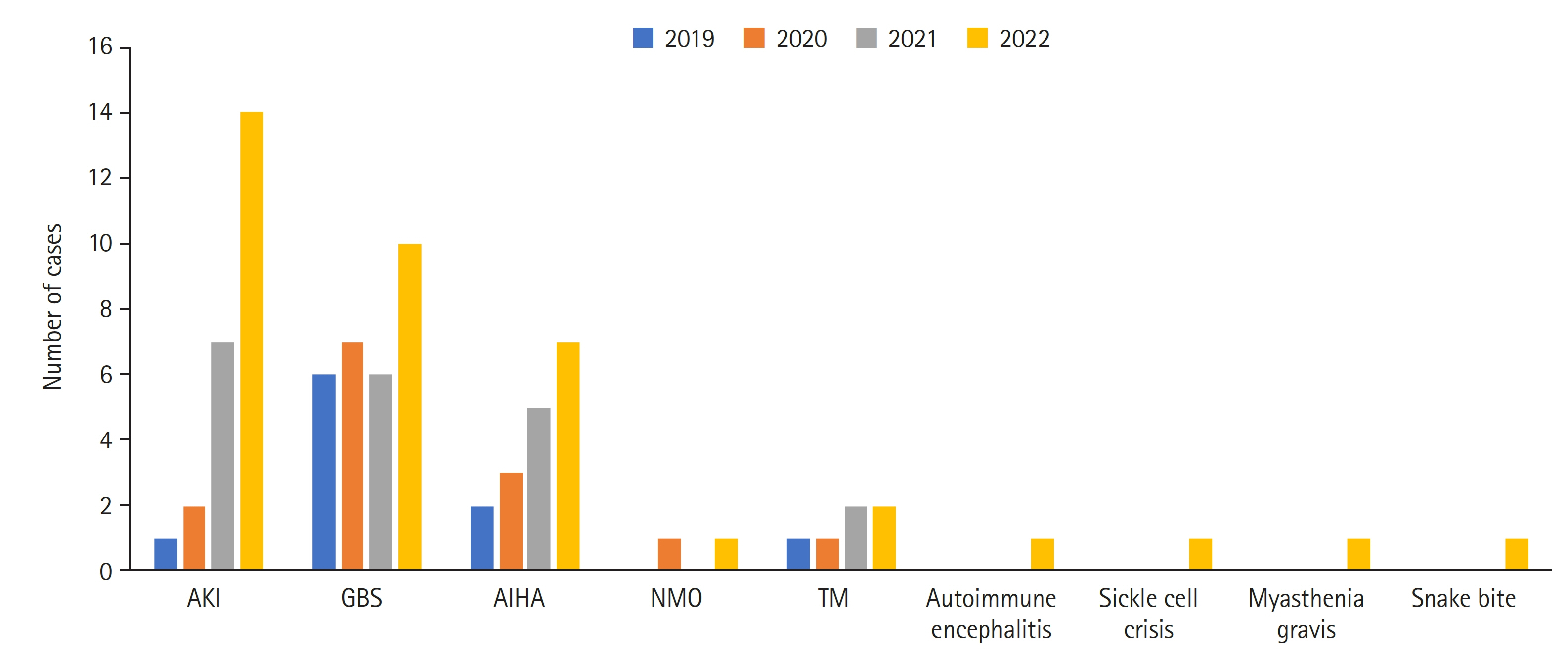
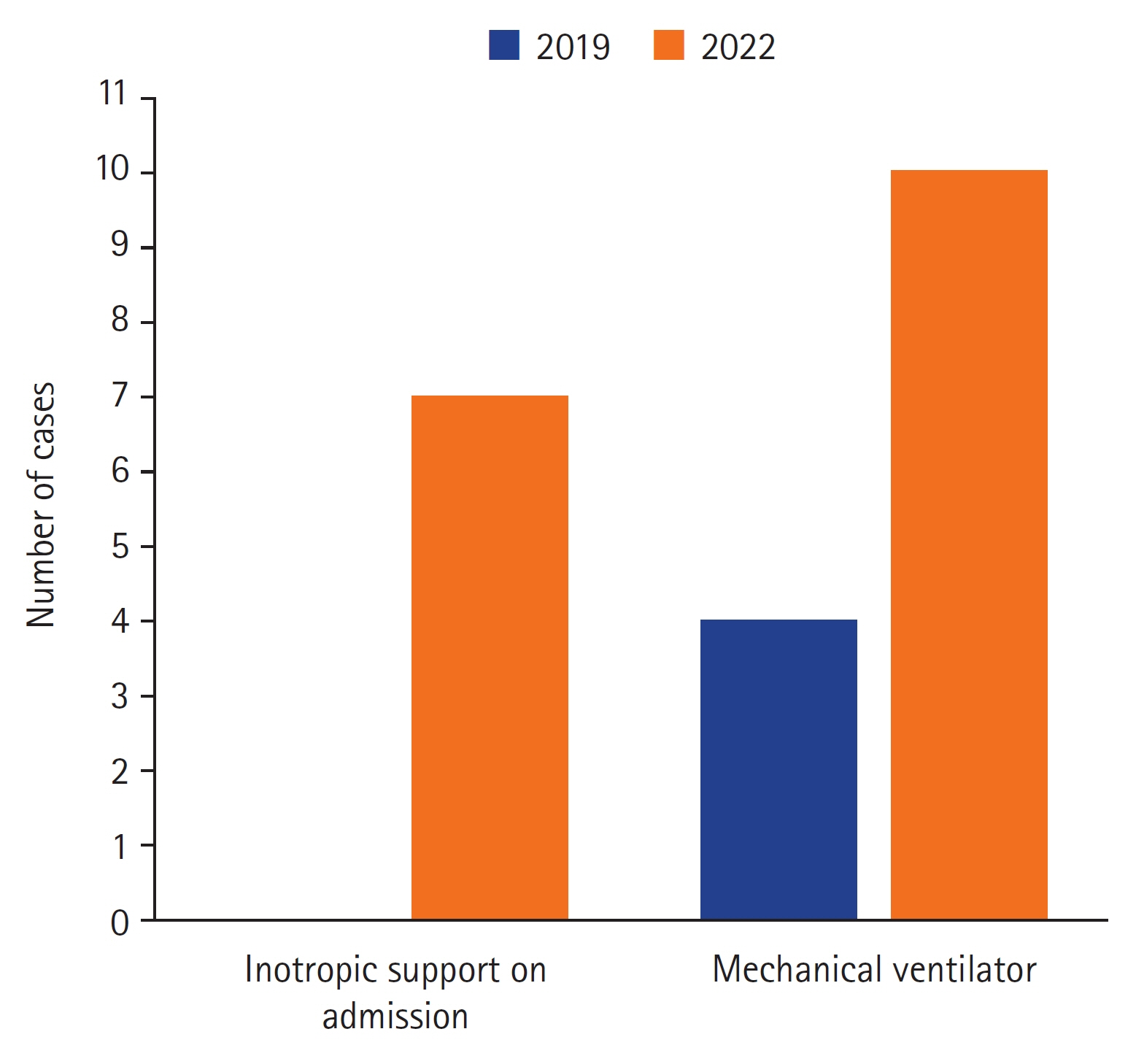
Extracorporeal blood-purification techniques are frequently needed in the pediatric intensive care unit (PICU), yet data on their clinical application are lacking. This study aims to review the indications, rate of application, clinical characteristics, complications, and outcomes of patients undergoing extracorporeal blood purification (i.e., by continuous renal replacement therapy [CRRT] or therapeutic plasma exchange [TPE]) in our PICU, including before the coronavirus disease 2019 (COVID-19) pandemic in 2019 and during the pandemic from 2020 to 2022. Methods: This study included children admitted for extracorporeal blood-purification therapy in the PICU. The indications for TPE were analyzed and compared to the American Society for Apheresis categories. Results: In 82 children, 380 TPE sessions and 37 CRRT sessions were carried out children, with 65 patients (79%) receiving TPE, 17 (20.7%) receiving CRRT, and four (4.8%) receiving both therapies. The most common indications for TPE were neurological diseases (39/82, 47.5%), followed by hematological diseases (18/82, 21.9%). CRRT was mainly performed for patients suffering from acute kidney injury. Patients with neurological diseases received the greatest number of TPE sessions (295, 77.6%). Also, the year 2022 contained the greatest number of patients receiving extracorporeal blood-purification therapy (either CRRT or TPE). Conclusions: The use of extracorporeal blood-purification techniques increased from 2019 through 2022 due to mainly autoimmune dysregulation among affected patients. TPE can be safely used in an experienced PICU. No serious adverse events were observed in the patients that received TPE, and overall survival over the 4 years was 86.5%.
Keyword
Figure
Reference
-
1. Haque A, Bano S. Clinical profile and outcome in a paediatric intensive care unit in Pakistan. J Coll Physicians Surg Pak. 2009; 19:534–5.2. Aygün F, Varol F, Durak C, Talip Petmezci M, Kacar A, Dursun H, et al. Evaluation of continuous renal replacement therapy and therapeutic plasma exchange, in severe sepsis or septic shock in critically ill children. Medicina (Kaunas). 2019; 55:350.
Article3. Cortina G, McRae R, Hoq M, Donath S, Chiletti R, Arvandi M, et al. Mortality of critically ill children requiring continuous renal replacement therapy: effect of fluid overload, underlying disease, and timing of initiation. Pediatr Crit Care Med. 2019; 20:314–22.
Article4. Han F, Sun R, Ni Y, Hu X, Chen X, Jiang L, et al. Early initiation of continuous renal replacement therapy improves clinical outcomes in patients with acute respiratory distress syndrome. Am J Med Sci. 2015; 349:199–205.
Article5. Raina R, Chakraborty R, Sethi SK, Bunchman T. Kidney replacement therapy in COVID-19 Induced kidney failure and septic shock: a pediatric continuous renal replacement therapy [PCRRT] position on emergency preparedness with resource allocation. Front Pediatr. 2020; 8:413.
Article6. Daverio M, Cortina G, Jones A, Ricci Z, Demirkol D, Raymakers-Janssen P, et al. Continuous kidney replacement therapy practices in pediatric intensive care units across Europe. JAMA Netw Open. 2022; 5:e2246901.
Article7. Sanchez AP, Ward DM, Cunard R. Therapeutic plasma exchange in the intensive care unit: rationale, special considerations, and techniques for combined circuits. Ther Apher Dial. 2022; 26 Suppl 1:41–52.
Article8. Özsoylu S, Dursun A, Çelik B. Therapeutic plasma exchange in pediatric intensive care unit: a single-center experience. Indian J Crit Care Med. 2021; 25:1189–92.
Article9. Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, et al. Guidelines on the use of therapeutic apheresis in clinical practice: evidence-based approach from the Writing Committee of the American Society for Apheresis: the eighth special issue. J Clin Apher. 2019; 34:171–354.
Article10. Cao JS, He J, Zhang XP, Zhou X, Xiao ZH. Therapeutic plasma exchange in the pediatric intensive care unit: a single-center retrospective study. Zhongguo Dang Dai Er Ke Za Zhi. 2022; 24:1149–53.11. Abate BB, Kassie AM, Kassaw MW, Aragie TG, Masresha SA. Sex difference in coronavirus disease (COVID-19): a systematic review and meta-analysis. BMJ Open. 2020; 10:e040129.
Article12. Kocivnik N, Velnar T. A review pertaining to SARS-CoV-2 and autoimmune diseases: what is the connection? Life (Basel). 2022; 12:1918.
Article13. Chan YH. Biostatistics 103: qualitative data: tests of independence. Singapore Med J. 2003; 44:498–503.14. Bustos B R, Hickmann O L, Cruces R P, Díaz F. Therapeutic plasma exchange in critically ill children: experience of the pediatric intensive care unit of two centers in Chile. Transfus Apher Sci. 2021; 60:103181.
Article15. Tufan Pekkucuksen N, Sigler KE, Akcan Arikan A, Srivaths P. Tandem plasmapheresis and continuous kidney replacement treatment in pediatric patients. Pediatr Nephrol. 2021; 36:1273–8.
Article16. Zee-Cheng JE, McCluskey CK, Klein MJ, Scanlon MC, Rotta AT, Shein SL, et al. Changes in pediatric ICU utilization and clinical trends during the coronavirus pandemic. Chest. 2021; 160:529–37.
Article17. Kanthimathinathan HK, Buckley H, Davis PJ, Feltbower RG, Lamming C, Norman L, et al. In the eye of the storm: impact of COVID-19 pandemic on admission patterns to paediatric intensive care units in the UK and Eire. Crit Care. 2021; 25:399.
Article18. Osamor VC, Ikeakanam E, Bishung JU, Abiodun TN, Ekpo RH. COVID-19 vaccines: computational tools and development. Inform Med Unlocked. 2023; 37:101164.
Article19. Gigli GL, Bax F, Marini A, Pellitteri G, Scalise A, Surcinelli A, et al. Guillain-Barré syndrome in the COVID-19 era: just an occasional cluster? J Neurol. 2021; 268:1195–7.
Article20. Goel N, Mehndiratta S, Singh A. Post COVID-19 Guillain Barre syndrome in immunocompromised children: a report of two cases and review of literature. Research Square [Preprint]. 2021 [cited 2023 Dec 12]. https://doi.org/10.21203/rs.3.rs-922503/v1.
Article21. Taherifard E, Taherifard E, Movahed H, Mousavi MR. Hematologic autoimmune disorders in the course of COVID-19: a systematic review of reported cases. Hematology. 2021; 26:225–39.
Article22. Zama D, Pancaldi L, Baccelli F, Guida F, Gottardi F, Dentale N, et al. Autoimmune hemolytic anemia in children with COVID-19. Pediatr Blood Cancer. 2022; 69:e29330.
Article23. Mittal A, Nadig P, Singh K. Renal manifestations of COVID 19 in children. J Family Med Prim Care. 2022; 11:2302–10.
Article24. Chang YM, Chou YT, Kan WC, Shiao CC. Sepsis and acute kidney injury: a review focusing on the bidirectional interplay. Int J Mol Sci. 2022; 23:9159.
Article25. Buccione E, Guzzi F, Colosimo D, Tedesco B, Romagnoli S, Ricci Z, et al. Continuous renal replacement therapy in critically ill children in the pediatric intensive care unit: a retrospective analysis of real-life prescriptions, complications, and outcomes. Front Pediatr. 2021; 9:696798.
Article26. Öztürk AG, Küçük ZE, Özcan S, Havan M, Gün E, Botan E, et al. Use of therapeutic plasma exchange in the pediatric intensive care unit. Turk Arch Pediatr. 2022; 57:186–92.27. Cortina G, McRae R, Chiletti R, Butt W. Therapeutic plasma exchange in critically ill children requiring intensive care. Pediatr Crit Care Med. 2018; 19:e97–104.
Article28. Miklaszewska M, Korohoda P, Zachwieja K, Sobczak A, Kobylarz K, Stefanidis CJ, et al. Factors affecting mortality in children requiring continuous renal replacement therapy in pediatric intensive care unit. Adv Clin Exp Med. 2019; 28:615–23.
Article29. Haga T, Ide K, Tani M. Characteristics of pediatric continuous renal replacement therapies in hospitals with pediatric intensive care units in Japan. Ther Apher Dial. 2023; 27:562–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience of Treating Critically Ill COVID-19 Patients in Daegu, South Korea
- How We Have Treated Severe to Critically Ill Patients With Coronavirus Disease 2019 in Korea
- New York City Vascular Surgeons during the COVID-19 Pandemic
- Risk factors associated with development of coinfection in critically Ill patients with COVID-19
- Treatment of Critically Ill Patients with Coronavirus Disease 2019