J Korean Med Sci.
2024 Apr;39(13):e131. 10.3346/jkms.2024.39.e131.
Association Between Individual Air Pollution (PM 10 , PM2.5) Exposure and Adverse Pregnancy Outcomes in Korea: A Multicenter Prospective Cohort, Air Pollution on Pregnancy Outcome (APPO) Study
- Affiliations
-
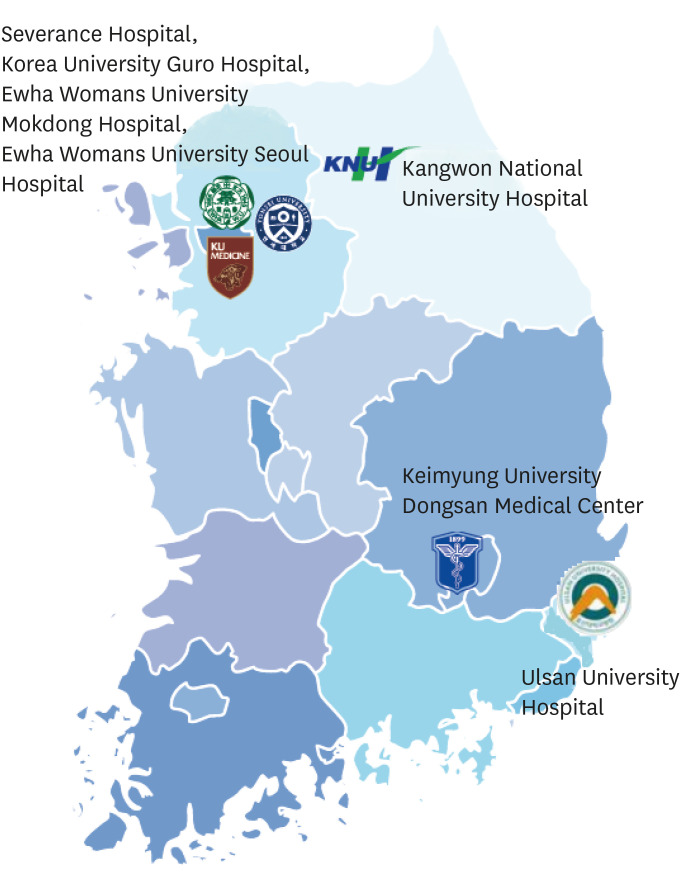
- 1Department of Obstetrics and Gynecology, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Department of Obstetrics and Gynecology, Ewha Womans University Mokdong Hospital, Ewha Medical Research Institute College of Medicine, Seoul, Korea
- 3Graduate Program in System Health Science and Engineering, Ewha Womans University, Seoul, Korea
- 4Department of Obstetrics and Gynecology, College of Medicine, Ewha Womans University, Seoul, Korea
- 5Division of Artificial Intelligence and Software/Artificial Intelligence Convergence, Ewha Womans University, Seoul, Korea
- 6Department of Obstetrics and Gynecology, Ewha Womans University Seoul Hospital, Seoul, Korea
- 7Department of Obstetrics and Gynecology, School of Medicine, Keimyung University, Dongsan Medical Center, Daegu, Korea
- 8Department of Obstetrics and Gynecology, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea
- 9Department of Obstetrics and Gynecology, Severance Hospital, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2554581
- DOI: http://doi.org/10.3346/jkms.2024.39.e131
Abstract
- Background
Prenatal exposure to ambient air pollution is linked to a higher risk of unfavorable pregnancy outcomes. However, the association between pregnancy complications and exposure to indoor air pollution remains unclear. The Air Pollution on Pregnancy Outcomes research is a hospital-based prospective cohort research created to look into the effects of aerodynamically exposed particulate matter (PM) 10 and PM 2.5 on pregnancy outcomes.
Methods
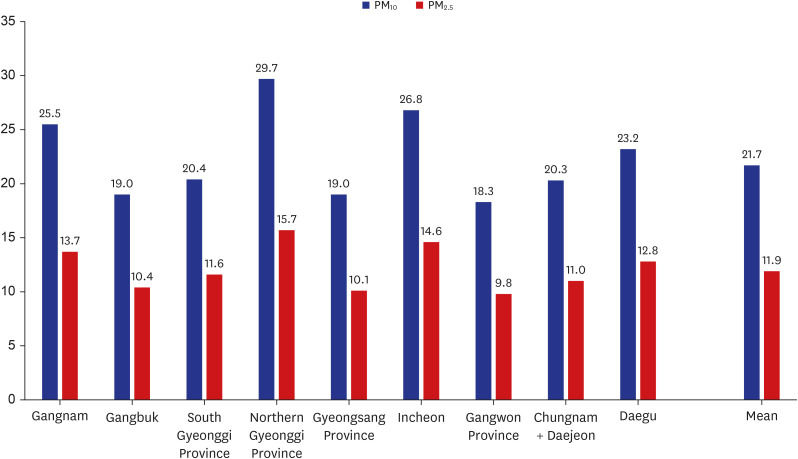
This prospective multicenter observational cohort study was conducted from January 2021 to June 2023. A total of 662 women with singleton pregnancies enrolled in this study. An AirguardK ® air sensor was installed inside the homes of the participants to measure the individual PM 10 and PM 2.5 levels in the living environment. The time–activity patterns and PM 100 and PM 2.5 , determined as concentrations from the time-weighted average model, were applied to determine the anticipated exposure levels to air pollution of each pregnant woman. The relationship between air pollution exposure and pregnancy outcomes was assessed using logistic and linear regression analyses.
Results
Exposure to elevated levels of PM 10 throughout the first, second, and third trimesters as well as throughout pregnancy was strongly correlated with the risk of pregnancy problems according to multiple logistic regression models adjusted for variables. Except for in the third trimester of pregnancy, women exposed to high levels of PM 2.5 had a high risk of pregnancy complications. During the second trimester and entire pregnancy, the risk of preterm birth (PTB) increased by 24% and 27%, respectively, for each 10 μg/m 3 increase in PM 10. Exposure to high PM 10 levels during the second trimester increased the risk of gestational diabetes mellitus (GDM) by 30%. The risk of GDM increased by 15% for each 5 μg/m 3 increase in PM2.5 during the second trimester and overall pregnancy, respectively. Exposure to high PM 10 and PM 2.5 during the first trimester of pregnancy increased the risk of delivering small for gestational age (SGA) infants by 96% and 26%, respectively.
Conclusion
Exposure to high concentrations of PM 10 and PM 2.5 is strongly correlated with the risk of adverse pregnancy outcomes. Exposure to high levels of PM10 and PM2.5 during the second trimester and entire pregnancy, respectively, significantly increased the risk of PTB and GDM. Exposure to high levels of PM 10 and PM2.5 during the first trimester of pregnancy considerably increased the risk of having SGA infants. Our findings highlight the need to measure individual particulate levels during pregnancy and the importance of managing air quality in residential environment.
Keyword
Figure
Reference
-
1. He MZ, Zeng X, Zhang K, Kinney PL. Fine particulate matter concentrations in urban Chinese cities, 2005–2016: a systematic review. Int J Environ Res Public Health. 2017; 14(2):191. PMID: 28216601.2. Kim KH, Kabir E, Kabir S. A review on the human health impact of airborne particulate matter. Environ Int. 2015; 74:136–143. PMID: 25454230.3. Morales-Ancajima VC, Tapia V, Vu BN, Liu Y, Alarcón-Yaquetto DE, Gonzales GF. Increased outdoor PM2.5 concentration is associated with moderate/severe anemia in children aged 6–59 months in Lima, Peru. J Environ Public Health. 2019; 2019:6127845. PMID: 31428166.4. Ten threats to global health in 2019. Updated 2020. Accessed April 29, 2020. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 .5. de Melo JO, Soto SF, Katayama IA, Wenceslau CF, Pires AG, Veras MM, et al. Inhalation of fine particulate matter during pregnancy increased IL-4 cytokine levels in the fetal portion of the placenta. Toxicol Lett. 2015; 232(2):475–480. PMID: 25481569.6. Fussell JC, Jauniaux E, Smith RB, Burton GJ. Ambient air pollution and adverse birth outcomes: A review of underlying mechanisms. BJOG. 2024; 131(5):538–550. PMID: 38037459.7. Liu Y, Wang L, Wang F, Li C. Effect of fine particulate matter (PM2.5) on rat placenta pathology and perinatal outcomes. Med Sci Monit. 2016; 22:3274–3280. PMID: 27629830.8. Dockery DW. Epidemiologic evidence of cardiovascular effects of particulate air pollution. Environ Health Perspect. 2001; 109:Suppl 4. (Suppl 4):483–486. PMID: 11544151.9. Peters A. Particulate matter and heart disease: evidence from epidemiological studies. Toxicol Appl Pharmacol. 2005; 207(2):Suppl. 477–482. PMID: 15990137.10. Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010; 121(21):2331–2378. PMID: 20458016.11. Sun Q, Hong X, Wold LE. Cardiovascular effects of ambient particulate air pollution exposure. Circulation. 2010; 121(25):2755–2765. PMID: 20585020.12. Stieb DM, Chen L, Eshoul M, Judek S. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ Res. 2012; 117:100–111. PMID: 22726801.13. Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen AM, Ballester F, et al. Ambient air pollution and low birthweight: a European cohort study (ESCAPE). Lancet Respir Med. 2013; 1(9):695–704. PMID: 24429273.14. Hur YM, Park S, Kwon E, You YA, Ansari A, Kim SM, et al. The introduction to air pollution on pregnancy outcome (APPO) study: a multicenter cohort study. Obstet Gynecol Sci. 2023; 66(3):169–180. PMID: 36973177.15. Gestational hypertension and preeclampsia: ACOG practice bulletin, number 222. Obstet Gynecol. 2020; 135(6):e237–e260. PMID: 32443079.16. Cole TJ, Williams AF, Wright CM. RCPCH Growth Chart Expert Group. Revised birth centiles for weight, length and head circumference in the UK-WHO growth charts. Ann Hum Biol. 2011; 38(1):7–11. PMID: 21175302.17. Cunningham FG, Leveno KJ, Dashe JS, Hoffman BL, Spong CY, Casey BM. Williams Obstetrics, 26e. New York, NY: McGraw Hill;2022.18. AirKorea website by the Korean Ministry of Environment. Updated 2022. Accessed October 17, 2022. http://www.airkorea.or.kr/web .19. Del Rio D, Stewart AJ, Pellegrini N. A review of recent studies on malondialdehyde as toxic molecule and biological marker of oxidative stress. Nutr Metab Cardiovasc Dis. 2005; 15(4):316–328. PMID: 16054557.20. Kirchstetter TW, Novakov T. Controlled generation of black carbon particles from a diffusion flame and applications in evaluating black carbon measurement methods. Atmos Environ. 2007; 41(9):1874–1888.21. iCReaT web-based clinical research management system. Updated 2017. Accessed October 17, 2022. http://icreat.nih.go.kr/icreat/webapps/com/hismainweb/jsp/guide_n2.jsp?sel=03 .22. World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Geneva, Switzerland: World Health Organization;2021.23. Qian Z, Liang S, Yang S, Trevathan E, Huang Z, Yang R, et al. Ambient air pollution and preterm birth: a prospective birth cohort study in Wuhan, China. Int J Hyg Environ Health. 2016; 219(2):195–203. PMID: 26639560.24. Hansen C, Neller A, Williams G, Simpson R. Maternal exposure to low levels of ambient air pollution and preterm birth in Brisbane, Australia. BJOG. 2006; 113(8):935–941. PMID: 16907939.25. Balsa AI, Caffera M, Bloomfield J. Exposures to particulate matter from the eruptions of the Puyehue volcano and birth outcomes in Montevideo, Uruguay. Environ Health Perspect. 2016; 124(11):1816–1822. PMID: 27152597.26. Suh YJ, Kim H, Seo JH, Park H, Kim YJ, Hong YC, et al. Different effects of PM10 exposure on preterm birth by gestational period estimated from time-dependent survival analyses. Int Arch Occup Environ Health. 2009; 82(5):613–621. PMID: 18998152.27. Hu H, Ha S, Henderson BH, Warner TD, Roth J, Kan H, et al. Association of atmospheric particulate matter and ozone with gestational diabetes mellitus. Environ Health Perspect. 2015; 123(9):853–859. PMID: 25794412.28. Choe SA, Kauderer S, Eliot MN, Glazer KB, Kingsley SL, Carlson L, et al. Air pollution, land use, and complications of pregnancy. Sci Total Environ. 2018; 645:1057–1064. PMID: 30248831.29. Shen HN, Hua SY, Chiu CT, Li CY. Maternal exposure to air pollutants and risk of gestational diabetes mellitus in Taiwan. Int J Environ Res Public Health. 2017; 14(12):1604. PMID: 29261145.30. Ha S, Zhu Y, Liu D, Sherman S, Mendola P. Ambient temperature and air quality in relation to small for gestational age and term low birthweight. Environ Res. 2017; 155:394–400. PMID: 28258738.31. Hansen C, Neller A, Williams G, Simpson R. Low levels of ambient air pollution during pregnancy and fetal growth among term neonates in Brisbane, Australia. Environ Res. 2007; 103(3):383–389. PMID: 16890220.32. Le HQ, Batterman SA, Wirth JJ, Wahl RL, Hoggatt KJ, Sadeghnejad A, et al. Air pollutant exposure and preterm and term small-for-gestational-age births in Detroit, Michigan: long-term trends and associations. Environ Int. 2012; 44:7–17. PMID: 22314199.33. Mannes T, Jalaludin B, Morgan G, Lincoln D, Sheppeard V, Corbett S. Impact of ambient air pollution on birth weight in Sydney, Australia. Occup Environ Med. 2005; 62(8):524–530. PMID: 16046604.34. Percy Z, DeFranco E, Xu F, Hall ES, Haynes EN, Jones D, et al. Trimester specific PM2.5 exposure and fetal growth in Ohio, 2007–2010. Environ Res. 2019; 171:111–118. PMID: 30660917.35. Ritz B, Wilhelm M, Hoggatt KJ, Ghosh JK. Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am J Epidemiol. 2007; 166(9):1045–1052. PMID: 17675655.36. Stieb DM, Chen L, Hystad P, Beckerman BS, Jerrett M, Tjepkema M, et al. A national study of the association between traffic-related air pollution and adverse pregnancy outcomes in Canada, 1999–2008. Environ Res. 2016; 148:513–526. PMID: 27155984.37. Vinikoor-Imler LC, Gray SC, Edwards SE, Miranda ML. The effects of exposure to particulate matter and neighbourhood deprivation on gestational hypertension. Paediatr Perinat Epidemiol. 2012; 26(2):91–100.38. Lee PC, Roberts JM, Catov JM, Talbott EO, Ritz B. First trimester exposure to ambient air pollution, pregnancy complications and adverse birth outcomes in Allegheny County, PA. Matern Child Health J. 2013; 17(3):545–555. PMID: 22544506.39. Dadvand P, Figueras F, Basagaña X, Beelen R, Martinez D, Cirach M, et al. Ambient air pollution and preeclampsia: a spatiotemporal analysis. Environ Health Perspect. 2013; 121(11-12):1365–1371. PMID: 24021707.40. Choe SA, Eliot MN, Savitz DA, Wellenius GA. Ambient air pollution during pregnancy and risk of gestational diabetes in New York City. Environ Res. 2019; 175:414–420. PMID: 31154231.41. Fleisch AF, Gold DR, Rifas-Shiman SL, Koutrakis P, Schwartz JD, Kloog I, et al. Air pollution exposure and abnormal glucose tolerance during pregnancy: the project Viva cohort. Environ Health Perspect. 2014; 122(4):378–383. PMID: 24508979.42. Fleisch AF, Kloog I, Luttmann-Gibson H, Gold DR, Oken E, Schwartz JD. Air pollution exposure and gestational diabetes mellitus among pregnant women in Massachusetts: a cohort study. Environ Health. 2016; 15(1):40. PMID: 26911579.43. Brauer M, Lencar C, Tamburic L, Koehoorn M, Demers P, Karr C. A cohort study of traffic-related air pollution impacts on birth outcomes. Environ Health Perspect. 2008; 116(5):680–686. PMID: 18470315.44. Capobussi M, Tettamanti R, Marcolin L, Piovesan L, Bronzin S, Gattoni ME, et al. Air pollution impact on pregnancy outcomes in Como, Italy. J Occup Environ Med. 2016; 58(1):47–52. PMID: 26716849.45. Hannam K, McNamee R, Baker P, Sibley C, Agius R. Air pollution exposure and adverse pregnancy outcomes in a large UK birth cohort: use of a novel spatio-temporal modelling technique. Scand J Work Environ Health. 2014; 40(5):518–530. PMID: 24647593.46. Madsen C, Gehring U, Walker SE, Brunekreef B, Stigum H, Naess O, et al. Ambient air pollution exposure, residential mobility and term birth weight in Oslo, Norway. Environ Res. 2010; 110(4):363–371. PMID: 20227069.47. Wang Q, Benmarhnia T, Li C, Knibbs LD, Bao J, Ren M, et al. Seasonal analyses of the association between prenatal ambient air pollution exposure and birth weight for gestational age in Guangzhou, China. Sci Total Environ. 2019; 649:526–534. PMID: 30179811.48. Stieb DM, Chen L, Beckerman BS, Jerrett M, Crouse DL, Omariba DW, et al. Associations of Pregnancy Outcomes and PM2.5 in a National Canadian Study. Environ Health Perspect. 2016; 124(2):243–249. PMID: 26090691.49. Hao H, Chang HH, Holmes HA, Mulholland JA, Klein M, Darrow LA, et al. Air pollution and preterm birth in the US State of Georgia (2002–2006): associations with concentrations of 11 ambient air pollutants estimated by combining Community Multiscale Air Quality Model (CMAQ) simulations with stationary monitor measurements. Environ Health Perspect. 2016; 124(6):87526485731.50. Hyder A, Lee HJ, Ebisu K, Koutrakis P, Belanger K, Bell ML. PM2.5 exposure and birth outcomes: use of satellite- and monitor-based data. Epidemiology. 2014; 25(1):58–67. PMID: 24240652.51. Wu H, Jiang B, Geng X, Zhu P, Liu Z, Cui L, et al. Exposure to fine particulate matter during pregnancy and risk of term low birth weight in Jinan, China, 2014–2016. Int J Hyg Environ Health. 2018; 221(2):183–190. PMID: 29097084.52. Xiao Q, Chen H, Strickland MJ, Kan H, Chang HH, Klein M, et al. Associations between birth outcomes and maternal PM2.5 exposure in Shanghai: a comparison of three exposure assessment approaches. Environ Int. 2018; 117:226–236. PMID: 29763818.53. Rich DQ, Demissie K, Lu SE, Kamat L, Wartenberg D, Rhoads GG. Ambient air pollutant concentrations during pregnancy and the risk of fetal growth restriction. J Epidemiol Community Health. 2009; a. 63(6):488–496. PMID: 19359274.54. Bell ML, Belanger K, Ebisu K, Gent JF, Lee HJ, Koutrakis P, et al. Prenatal exposure to fine particulate matter and birth weight: variations by particulate constituents and sources. Epidemiology. 2010; 21(6):884–891. PMID: 20811286.55. Guo C, Lv S, Liu Y, Li Y. Biomarkers for the adverse effects on respiratory system health associated with atmospheric particulate matter exposure. J Hazard Mater. 2022; 421:126760. PMID: 34396970.56. Slama R, Darrow L, Parker J, Woodruff TJ, Strickland M, Nieuwenhuijsen M, et al. Meeting report: atmospheric pollution and human reproduction. Environ Health Perspect. 2008; 116(6):791–798. PMID: 18560536.57. Janssen BG, Godderis L, Pieters N, Poels K, Kiciński M, Cuypers A, et al. Placental DNA hypomethylation in association with particulate air pollution in early life. Part Fibre Toxicol. 2013; 10(1):22. PMID: 23742113.58. Nachman RM, Mao G, Zhang X, Hong X, Chen Z, Soria CS, et al. Intrauterine inflammation and maternal exposure to ambient PM2.5 during preconception and specific periods of pregnancy: the Boston birth cohort. Environ Health Perspect. 2016; 124(10):1608–1615. PMID: 27120296.59. Park S, Kwon E, Lee G, You YA, Kim SM, Hur YM, et al. Effect of particulate matter 2.5 on fetal growth in male and preterm infants through oxidative stress. Antioxidants. 2023; 12(11):1916. PMID: 38001768.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The introduction to air pollution on pregnancy outcome (APPO) study: a multicenter cohort study
- Update in Association between Lung Cancer and Air Pollution
- Health Effects of Air Pollution on Fetus
- PM(2.5) and pediatric asthma
- Review of epidemiological studies on air pollution and health effects in children