Obstet Gynecol Sci.
2023 May;66(3):169-180. 10.5468/ogs.22278.
The introduction to air pollution on pregnancy outcome (APPO) study: a multicenter cohort study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ewha Womans University Mokdong Hospital, Ewha Medical Research Institute College of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Ewha Womans University Seoul Hospital, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Yonsei University, Seoul, Korea
- 4Department of Obstetrics and Gynecology, Yonsei University Gangnam Severance Hospital, Seoul, Korea
- 5Department of Obstetrics and Gynecology, Korea University Guro Hospital, Seoul, Korea
- 6Department of Obstetrics and Gynecology, Kangwon National University Hospital, Chuncheon, Korea
- 7Department of Obstetrics and Gynecology, Keimyung University Dongsan Medical Center, Daegu, Korea
- 8Department of Obstetrics and Gynecology, Ulsan University Hospital, Ulsan, Korea
- 9Department of Environmental Science and Engineering, College of Medicine, Ewha Medical Research Institute, Ewha Womans University, Seoul, Korea
- 10Department of Preventive Medicine, College of Medicine, Ewha Medical Research Institute, Ewha Womans University, Seoul, Korea
- KMID: 2542223
- DOI: http://doi.org/10.5468/ogs.22278
Abstract
Objective
The air pollution on pregnancy outcome (APPO) study is a prospective hospital-based cohort study designed to investigate the maternal and fetal effects of a particulate matter with an aerodynamic below 10 μm (PM10) and PM2.5 (below 2.5 μm) exposure. This study aims to analyze a relationship between particulate matter and adverse pregnancy outcomes and to find related biomarkers and develop management guidelines.
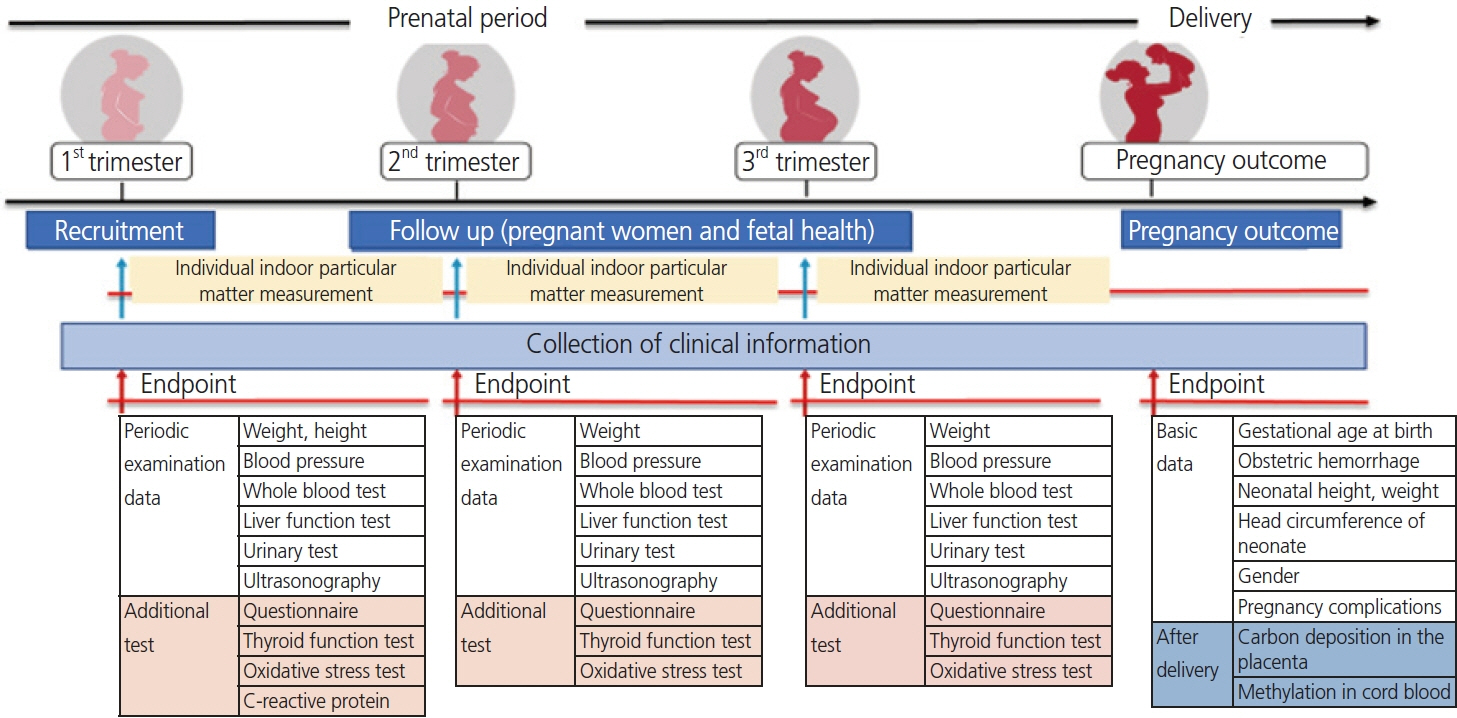
Methods
About 1,200 pregnant women are recruited for 3 years (from January 2021 to December 2023) from seven university hospitals to investigate the effects of particulate matter on pregnancy complications and adverse pregnancy outcomes. We collect biological samples by 5 mL of maternal venous blood and 15 mL of urine in each trimester of pregnancy, and 5 mL of umbilical cord blood and 2×2×2 cm of placental tissue are collected after delivery. In addition, by applying PM10 and PM2.5 concentration values and time-activity patterns from the time weighted average model, the individual predicted exposure of air pollution for the pregnant women are obtained.
Results
The average exposure of PM10 and PM2.5 of the participants in the entire period of pregnancy, was exceeded the World Health Organization air quality guidelines (an annual level, PM10 >15 μg/m3, PM2.5 >5 μg/m3). Moreover, it was revealed that the PM concentration was increasing toward the 3rd trimester of pregnancy.
Conclusion
The APPO study will be able to identify the degree of exposure to air pollution in pregnant women and use it as basic data for estimating individual exposure to particulate matter. And the results of the APPO study will facilitate in the development of health management for pregnant women against air pollution.
Keyword
Figure
Reference
-
References
1. Salam MT, Millstein J, Li YF, Lurmann FW, Margolis HG, Gilliland FD. Birth outcomes and prenatal exposure to ozone, carbon monoxide, and particulate matter: results from the children’s health study. Environ Health Perspect. 2005; 113:1638–44.
Article2. Kloog I, Melly SJ, Ridgway WL, Coull BA, Schwartz J. Using new satellite based exposure methods to study the association between pregnancy PM2.5 exposure, premature birth and birth weight in Massachusetts. Environ Health. 2012; 11:40.3. Perera FP, Rauh V, Whyatt RM, Tsai WY, Tang D, Diaz D, et al. Effect of prenatal exposure to airborne polycyclic aromatic hydrocarbons on neurodevelopment in the first 3 years of life among inner-city children. Environ Health Perspect. 2006; 114:1287–92.
Article4. van den Hooven EH, Pierik FH, de Kluizenaar Y, Willemsen SP, Hofman A, van Ratingen SW, et al. Air pollution exposure during pregnancy, ultrasound measures of fetal growth, and adverse birth outcomes: a prospective cohort study. Environ Health Perspect. 2012; 120:150–6.
Article5. Williams L, Spence A, Tideman SC. Implications of the observed effects of air pollution on birth weight. Soc Biol. 1977; 24:1–9.6. Parker JD, Woodruff TJ, Basu R, Schoendorf KC. Air pollution and birth weight among term infants in California. Pediatrics. 2005; 115:121–8.
Article7. Liu S, Krewski D, Shi Y, Chen Y, Burnett RT. Association between gaseous ambient air pollutants and adverse pregnancy outcomes in Vancouver, Canada. Environ Health Perspect. 2003; 111:1773–8.
Article8. Bobak M. Outdoor air pollution, low birth weight, and prematurity. Environ Health Perspect. 2000; 108:173–6.
Article9. Wang X, Ding H, Ryan L, Xu X. Association between air pollution and low birth weight: a community-based study. Environ Health Perspect. 1997; 105:514–20.
Article10. Ha EH, Hong YC, Lee BE, Woo BH, Schwartz J, Christiani DC. Is air pollution a risk factor for low birth weight in Seoul? Epidemiology. 2001; 12:643–8.
Article11. Lee BE, Ha EH, Park HS, Kim YJ, Hong YC, Kim H, et al. Exposure to air pollution during different gestational phases contributes to risks of low birth weight. Hum Reprod. 2003; 18:638–43.
Article12. Seo JH, Leem JH, Ha EH, Kim OJ, Kim BM, Lee JY, et al. Population-attributable risk of low birthweight related to PM10 pollution in seven Korean cities. Paediatr Perinat Epidemiol. 2010; 24:140–8.13. Ha EH, Lee BE, Park HS, Kim YS, Kim H, Kim YJ, et al. Prenatal exposure to PM10 and preterm birth between 1998 and 2000 in Seoul, Korea. J Prev Med Public Health. 2004; 37:300–5.14. Kang J, Lee JY, Song H, Shin SJ, Kim J. Association between in vitro fertilization success rate and ambient air pollution: a possible explanation of within-year variation of in vitro fertilization success rate. Obstet Gynecol Sci. 2020; 63:72–9.
Article15. Dadvand P, Parker J, Bell ML, Bonzini M, Brauer M, Darrow LA, et al. Maternal exposure to particulate air pollution and term birth weight: a multi-country evaluation of effect and heterogeneity. Environ Health Perspect. 2013; 121:267–373.
Article16. Statistics KOREA Government Official Work Conference. Air pollution in major cities [Internet]. Daejeon: Statistics KOREA Government Official Work Conference;c2022. [cited 2022 Oct 17]. Available from: https://www.index.go.kr/unity/potal/main/EachDtlPageDetail.do?idx_cd=2789 .17. Bell ML, Belanger K, Ebisu K, Gent JF, Lee HJ, Koutrakis P, et al. Prenatal exposure to fine particulate matter and birth weight: variations by particulate constituents and sources. Epidemiology. 2010; 21:884–91.18. Basu R, Harris M, Sie L, Malig B, Broadwin R, Green R. Effects of fine particulate matter and its constituents on low birth weight among full-term infants in California. Environ Res. 2014; 128:42–51.
Article19. Fattorini D, Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ Pollut. 2020; 264:114732.
Article20. Comunian S, Dongo D, Milani C, Palestini P. Air pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19’s morbidity and mortality. Int J Environ Res Public Health. 2020; 17:4487.
Article21. Ahn KH, Kim HI, Lee KS, Heo JS, Kim HY, Cho GJ, et al. COVID-19 and vaccination during pregnancy: a systematic analysis using Korea National Health Insurance claims data. Obstet Gynecol Sci. 2022; 65:487–501.
Article22. Akbar MIA, Gumilar KE, Andriya R, Wardhana MP, Mulawardhana P, Anas JY, et al. Clinical manifestations and pregnancy outcomes of COVID-19 in indonesian referral hospital in central pandemic area. Obstet Gynecol Sci. 2022; 65:29–36.
Article23. Peters A, Döring A, Wichmann HE, Koenig W. Increased plasma viscosity during an air pollution episode: a link to mortality? Lancet. 1997; 349:1582–7.
Article24. Kim BM, Ha M, Park HS, Lee BE, Kim YJ, Hong YC, et al. The mothers and children’s environmental health (MOCEH) study. Eur J Epidemiol. 2009; 24:573–83.
Article25. Wu LL, Chiou CC, Chang PY, Wu JT. Urinary 8-OHdG: a marker of oxidative stress to DNA and a risk factor for cancer, atherosclerosis and diabetics. Clin Chim Acta. 2004; 339:1–9.
Article26. Del Rio D, Stewart AJ, Pellegrini N. A review of recent studies on malondialdehyde as toxic molecule and biological marker of oxidative stress. Nutr Metab Cardiovasc Dis. 2005; 15:316–28.
Article27. Kirchstetter TW, Novakov T. Controlled generation of black carbon particles from a diffusion flame and applications in evaluating black carbon measurement methods. Atmospheric Environ. 2007; 41:1874–88.
Article28. Korea National Institute of Health. iCReaT web-based clnical research management system [Internet]. Cheongju: Korea National Institute of Health;c2022. [cited 2022 Oct 17]. Available from: http://icreat.nih.go.kr/icreat/webapps/com/hismainweb/jsp/guide_n2.jsp?sel=03Updated 2017.29. Korea Environment Corporation. AirKorea website by the Korean Ministry of Environment [Internet]. Incheon: Korea Environment Corporation;c2022. [cited 2022 Oct 17]. Available from: airkorea.or.kr/web/.30. World Health Organization. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide [Internet]. Geneva: WHO;c2021. [cited 2022 Dec 19]. Available from: https://apps.who.int/iris/handle/10665/345329 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association Between Individual Air Pollution (PM 10 , PM2.5) Exposure and Adverse Pregnancy Outcomes in Korea: A Multicenter Prospective Cohort, Air Pollution on Pregnancy Outcome (APPO) Study
- Health Effects of Air Pollution on Fetus
- Integrated dataset of the Korean Genome and Epidemiology Study cohort with estimated air pollution data
- Adverse health effects of climate change and air pollution in people with disabilities: a systematic review
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea