Korean J Gastroenterol.
2024 Feb;83(2):65-68. 10.4166/kjg.2023.147.
A Giant Gastric Perforation Occurring in the Normal Mucosa during Endoscopy in a Patient with Advanced Gastric Cancer
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2553437
- DOI: http://doi.org/10.4166/kjg.2023.147
Abstract
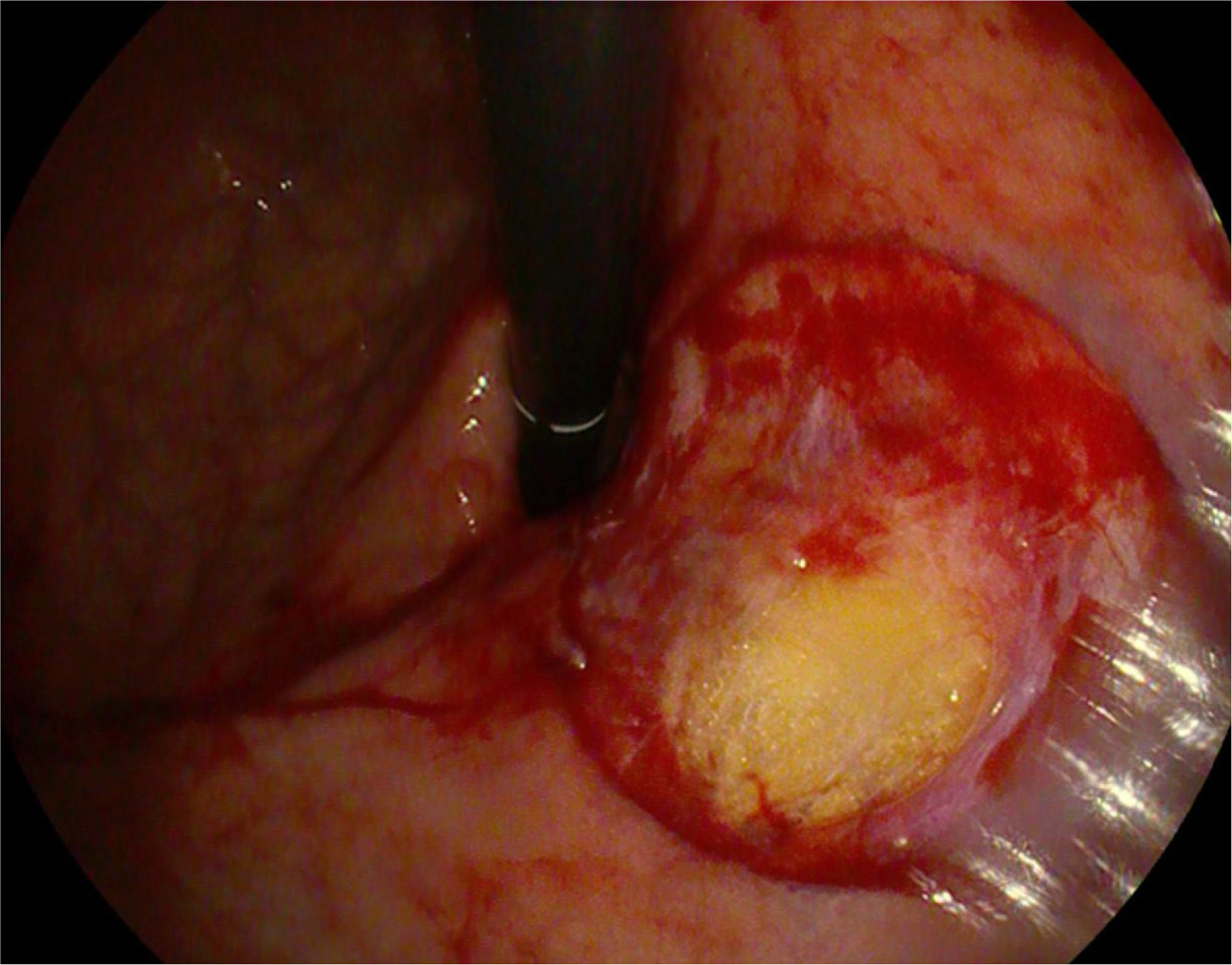
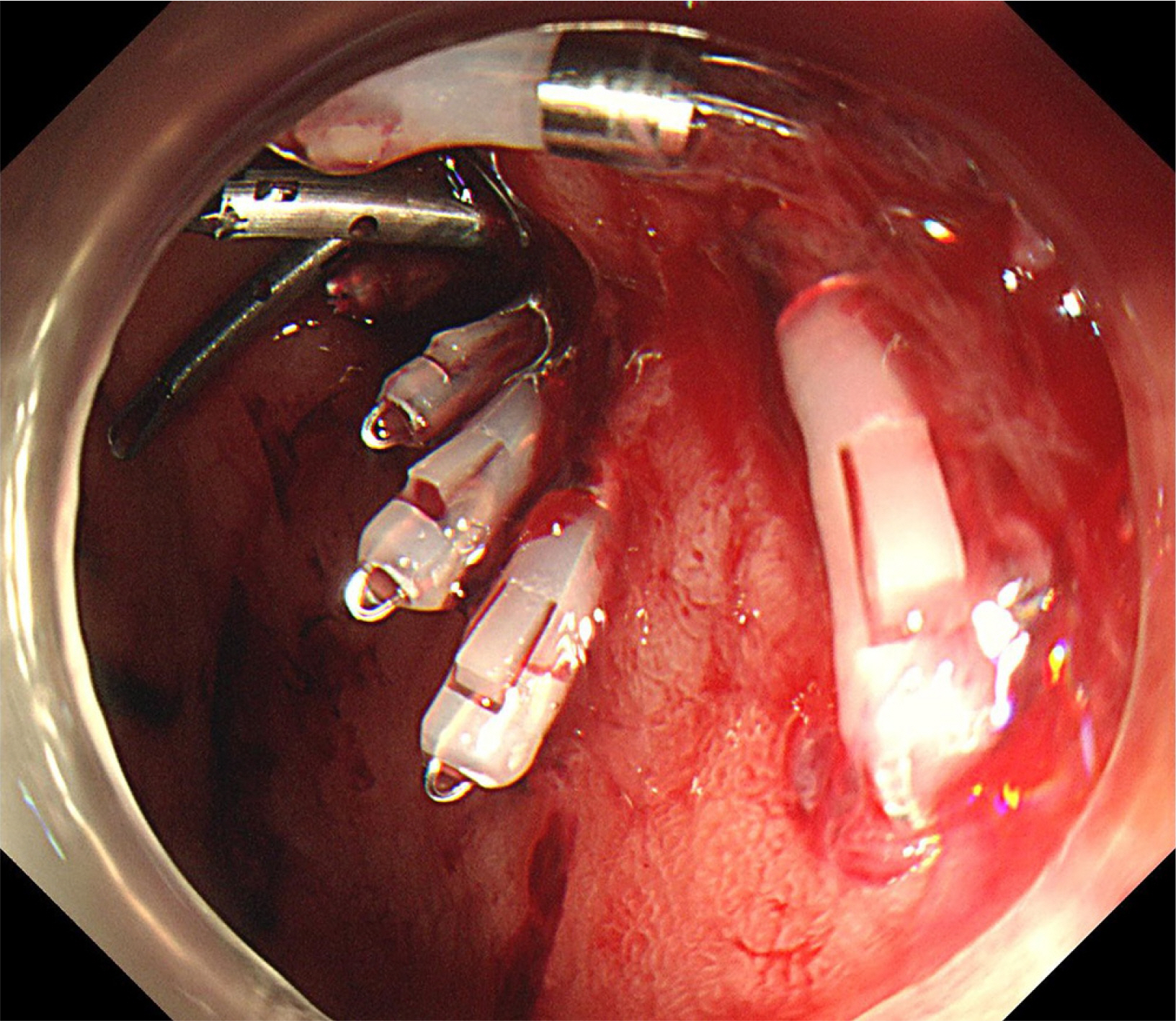
- The incidence of giant gastric perforation occurring during upper gastrointestinal endoscopy is exceedingly rare. Gastric perforation can arise from excessive air insufflation and is more prevalent in elderly patients with atrophic gastritis. Although giant gastric mucosal lacerations during diagnostic endoscopy have occasionally been reported, there are few reports of giant gastric perforation. The authors experienced a giant gastric perforation occurring in the normal mucosa during endoscopy in an 81-year-old woman with advanced gastric cancer. The patient had reduced gastric extensibility due to the advanced gastric cancer surrounding the entire lower part of her stomach. During continuous air insufflation, only the upper part of the stomach became overdistended, resulting in mucosal rupture and perforation. In addition, old age and the presence of atrophic gastritis contributed to the increased risk of mucosal rupture. The patient was treated successfully with endoscopic clips. This paper reports this case with a review of the relevant literature.
Keyword
Figure
Reference
-
1. Sieg A, Hachmoeller-Eisenbach U, Eisenbach T. 2001; Prospective evaluation of complications in outpatient GI endoscopy: a survey among German gastroenterologists. Gastrointest Endosc. 53:620–627. DOI: 10.1067/mge.2001.114422. PMID: 11323588.
Article2. Levy I, Gralnek IM. 2016; Complications of diagnostic colonoscopy, upper endoscopy, and enteroscopy. Best Pract Res Clin Gastroenterol. 30:705–718. DOI: 10.1016/j.bpg.2016.09.005. PMID: 27931631.
Article3. Park YS. 2023; A case of gastric perforation caused by excessive insufflation during upper gastrointestinal endoscopy: nonoperative management. Case Rep Gastroenterol. 17:327–332. DOI: 10.1159/000534866. PMID: 38020464. PMCID: PMC10651181.
Article4. Wurm Johansson G, Nemeth A, Nielsen J, et al. Gastric rupture as a rare complication in diagnostic upper gastrointestinal endoscopy. Endoscopy. 2013; 45 Suppl 2 UCTN:E391. DOI: 10.1055/s-0033-1344873. PMID: 24285064.
Article5. Sigmon DF, Tuma F, Kamel BG, Cassaro S. 2022. Gastric perforation. StatPearls. StatPearls Publishing;Treasure Island (FL):
Article6. Lee CH. 1999; Causes and incidence of each gastrointestinal tract perforation from 484 cases. J Korean Soc Emerg Med. 10:615–627.7. Decker JP, Zamcheck N, Mallory GK. 1953; Mallory-Weiss syndrome: hemorrhage from gastroesophageal lacerations at the cardiac orifice of the stomach. N Engl J Med. 249:957–963. DOI: 10.1056/NEJM195312102492401. PMID: 13111391.8. Myung SJ, Kim HR, Moon YS. 2000; Severe Mallory-Weiss tear after endoscopy treated by endoscopic band ligation. Gastrointest Endosc. 52:99–101. DOI: 10.1067/mge.2000.105071. PMID: 10882973.
Article9. Spoormans I, Van Hoorenbeeck K, Balliu L, Jorens PG. 2010; Gastric perforation after cardiopulmonary resuscitation: review of the literature. Resuscitation. 81:272–280. DOI: 10.1016/j.resuscitation.2009.11.023. PMID: 20064683.
Article10. Lee BS, Lee SH, Jang DK, et al. 2016; Belching during gastroscopy and its association with gastroesophageal reflux disease. Dis Esophagus. 29:342–349. DOI: 10.1111/dote.12326. PMID: 25708811.
Article11. Rayner CK, MacIntosh CG, Chapman IM, Morley JE, Horowitz M. 2000; Effects of age on proximal gastric motor and sensory function. Scand J Gastroenterol. 35:1041–1047. DOI: 10.1080/003655200451153. PMID: 11099056.
Article12. Lee SH, Nam SJ, Lee SJ, et al. 2022; Factors associated with belching and retching during esophagogastroduodenoscopy and their effects on Z-line appearance. Korean J Helicobacter Up Gastrointest Res. 22:295–302. DOI: 10.7704/kjhugr.2022.0035.
Article13. Minami S, Gotoda T, Ono H, Oda I, Hamanaka H. 2006; Complete endoscopic closure of gastric perforation induced by endoscopic resection of early gastric cancer using endoclips can prevent surgery (with video). Gastrointest Endosc. 63:596–601. DOI: 10.1016/j.gie.2005.07.029. PMID: 16564858.
Article14. Mangiavillano B, Viaggi P, Masci E. 2010; Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis. 11:12–18. DOI: 10.1111/j.1751-2980.2009.00414.x. PMID: 20132426.
Article15. Fujishiro M, Yahagi N, Kakushima N, et al. 2006; Successful nonsurgical management of perforation complicating endoscopic submucosal dissection of gastrointestinal epithelial neoplasms. Endoscopy. 38:1001–1006. DOI: 10.1055/s-2006-944775. PMID: 17058165.
Article16. Pasricha PJ, Fleischer DE, Kalloo AN. 1994; Endoscopic perforations of the upper digestive tract: a review of their pathogenesis, prevention, and management. Gastroenterology. 106:787–802. DOI: 10.1016/0016-5085(94)90717-X. PMID: 8119550.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Advanced Gastric Cancer, Developed from Endoscopic Diagnosis of Early Gastric Cancer
- Two Cases of Huge Polypoid Early Gastric Cancer
- Early gastric cancer arising from heterotopic gastric mucosa in the gastric submucosa
- A Case of Gastritis Cystica Profunda Associated with Gastric Perforation and Hypertrophic Gastric Folds
- Microbial Profile of the Stomach: Comparison between Normal Mucosa and Cancer Tissue in the Same Patient