Ann Lab Med.
2024 Mar;44(2):144-154. 10.3343/alm.2023.0083.
Predictive Performance of Neutrophil Gelatinase Associated Lipocalin, Liver Type Fatty Acid Binding Protein, and Cystatin C for Acute Kidney Injury and Mortality in Severely Ill Patients
- Affiliations
-
- 1INSERM UMR-S 942, Cardiovascular Markers in Stress Condition (MASCOT), Université de Paris Cité, Paris, France
- 2Department of Cardiovascular Medicine, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan
- 3Department of Anesthesiology, Critical Care and Burn Unit, University Hospitals Saint-Louis—Lariboisière, AP-HP, Paris, France
- 4Department of UFR de Médecine, Université de Paris Cité, Paris, France
- 5FHU PROMICE, Paris, France
- 6Department of Nephrology and Hypertension, St. Marianna University School of Medicine, Kanagawa, Japan
- 7Department of Cardiovascular Medicine, Kawaguchi Cardiovascular and Respiratory Hospital, Kawaguchi, Japan
- KMID: 2553381
- DOI: http://doi.org/10.3343/alm.2023.0083
Abstract
- Background
Acute kidney injury (AKI) is a common condition in severely ill patients associated with poor outcomes. We assessed the associations between urinary neutrophil gelatinase-associated lipocalin (uNGAL), urinary liver-type fatty acid-binding protein (uLFABP), and urinary cystatin C (uCysC) concentrations and patient outcomes.
Methods
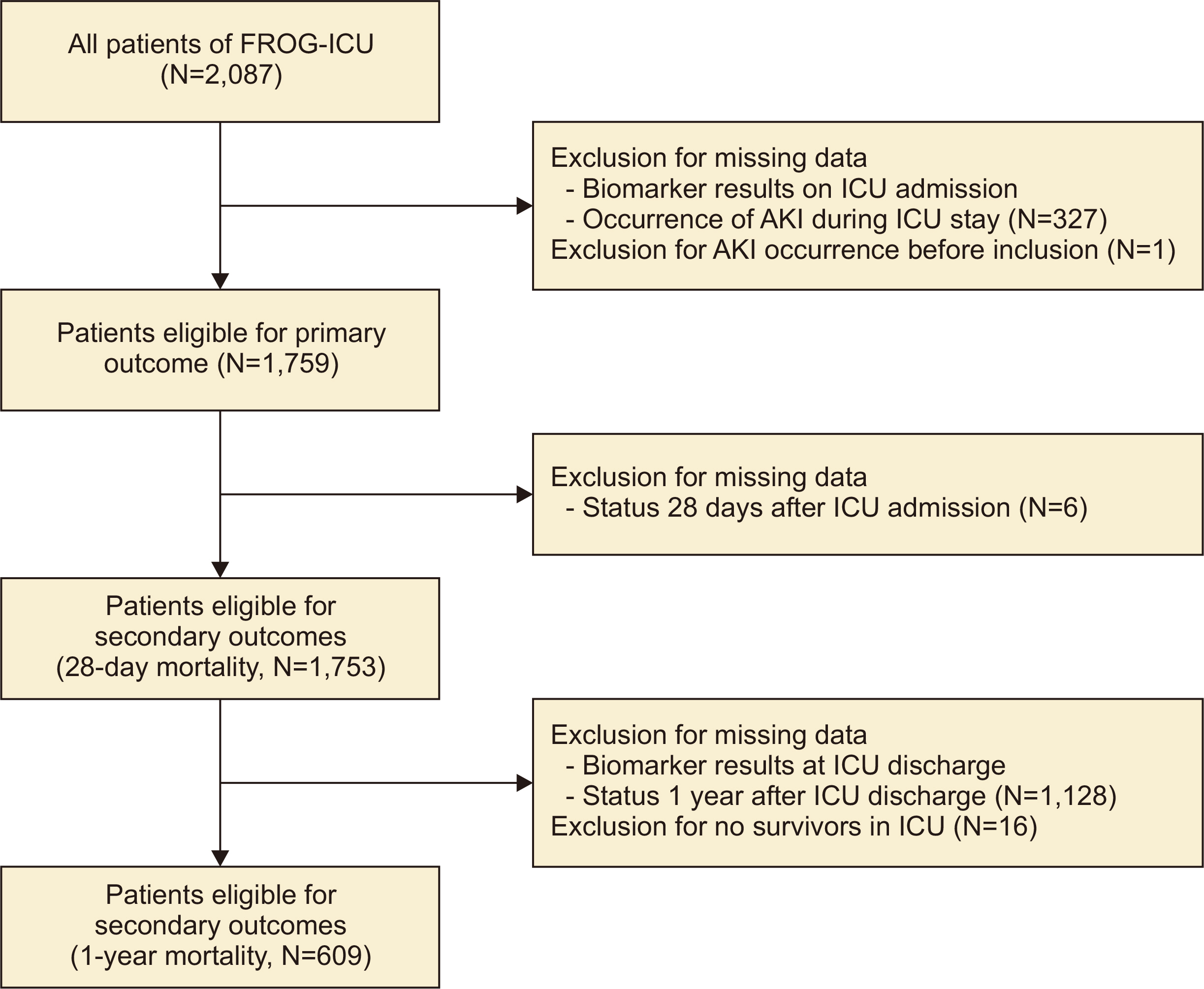
We assessed the predictive performances of uNGAL, uLFABP, and uCysC measured in the early phase of intensive care unit (ICU) management and at discharge from the ICU in severely ill patients for short- and long-term outcomes. The primary outcome was the occurrence of AKI during ICU stay; secondary outcomes were 28-day and 1-yr allcause mortality.
Results
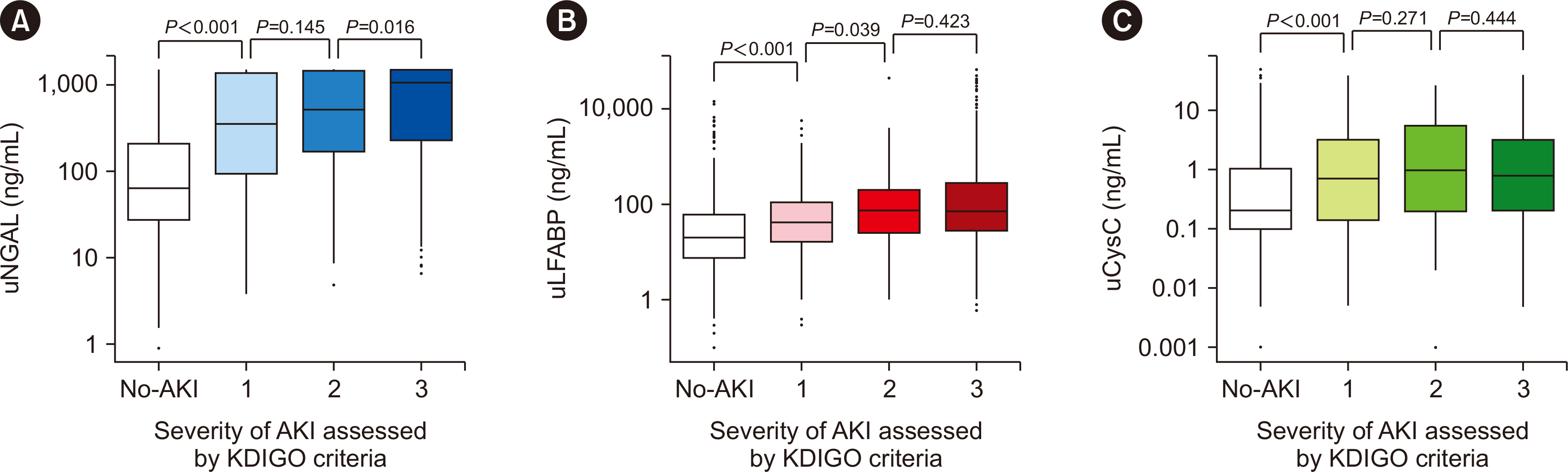
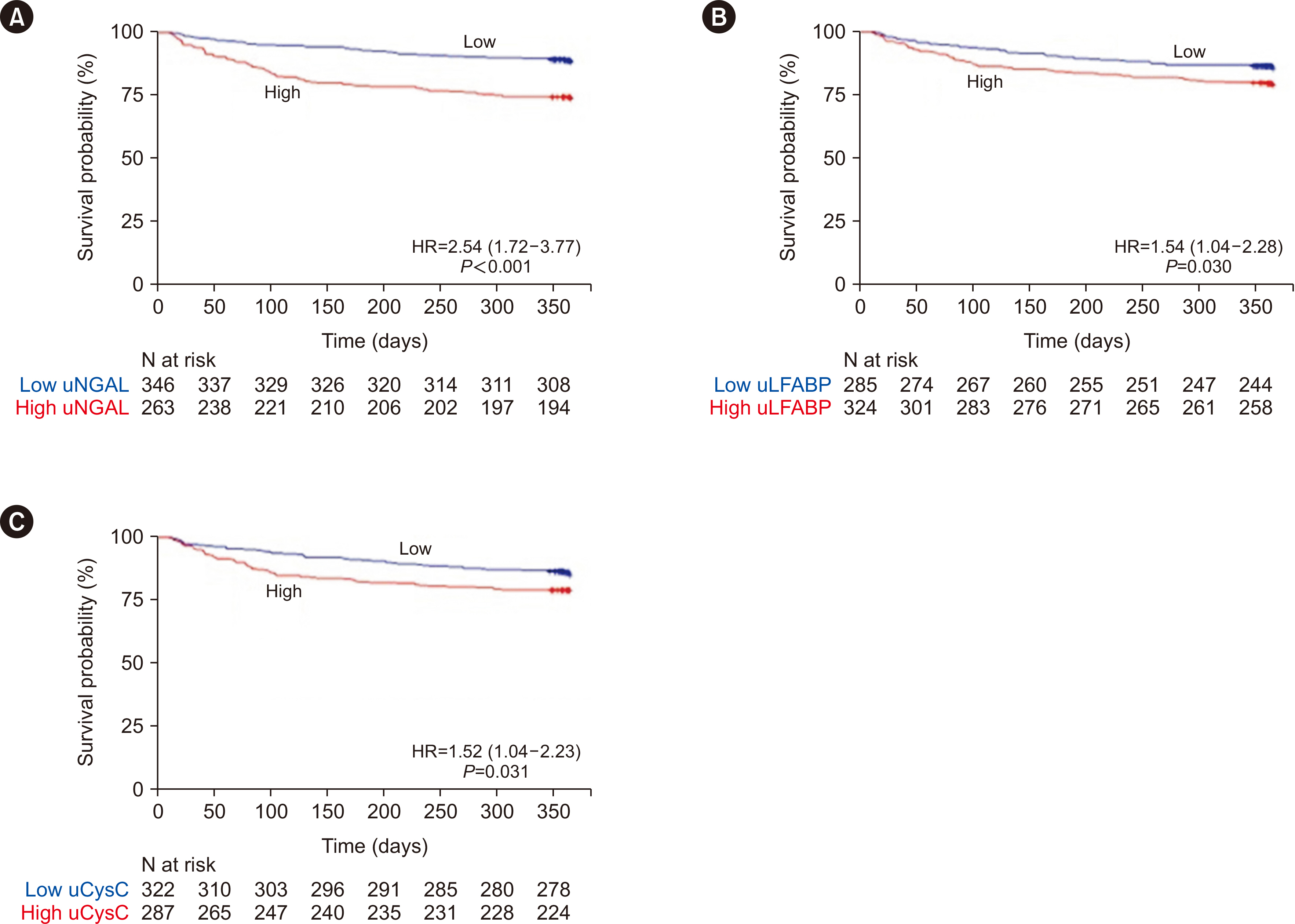
In total, 1,759 patients were admitted to the ICU, and 728 (41.4%) developed AKI. Median (interquartile range, IQR) uNGAL, uLFABP, and uCysC concentrations on admission were 147.6 (39.9–827.7) ng/mL, 32.4 (10.5–96.0) ng/mL, and 0.33 (0.12–2.05) mg/L, respectively. Biomarker concentrations on admission were higher in patients who developed AKI and associated with AKI severity. Three hundred fifty-six (20.3%) and 647 (37.9%) patients had died by 28 days and 1-yr, respectively. Urinary biomarker concentrations at ICU discharge were higher in non-survivors than in survivors. The areas under the ROC curve (95% confidence interval) of uLFABP for the prediction of AKI, 28-day mortality, and 1-yr mortality (0.70 [0.67–0.72], 0.63 [0.59–0.66], and 0.57 [0.51–0.63], respectively) were inferior to those of the other biomarkers.
Conclusions
uNGAL, uLFABP, and uCysC concentrations on admission were associated with poor outcomes. However, their predictive performance, individually and in combination, was limited. Further studies are required to confirm our results.
Keyword
Figure
Reference
-
1. Bagshaw SM, George C, Dinu I, Bellomo R. 2008; A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant. 23:1203–10. DOI: 10.1093/ndt/gfm744. PMID: 17962378.
Article2. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. 2005; Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 16:3365–70. DOI: 10.1681/ASN.2004090740. PMID: 16177006.
Article3. Ricci Z, Cruz D, Ronco C. 2008; The RIFLE criteria and mortality in acute kidney injury: A systematic review. Kidney Int. 73:538–46. DOI: 10.1038/sj.ki.5002743. PMID: 18160961.
Article4. Khwaja A. 2012; KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 120:c179–84. DOI: 10.1159/000339789. PMID: 22890468.
Article5. Star RA. 1998; Treatment of acute renal failure. Kidney Int. 54:1817–31. DOI: 10.1046/j.1523-1755.1998.00210.x. PMID: 9853246.
Article6. Moran SM, Myers BD. 1985; Course of acute renal failure studied by a model of creatinine kinetics. Kidney Int. 27:928–37. DOI: 10.1038/ki.1985.101. PMID: 4021321.
Article7. Schmidt-Ott KM, Mori K, Li JY, Kalandadze A, Cohen DJ, Devarajan P, et al. 2007; Dual action of neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol. 18:407–13. DOI: 10.1681/ASN.2006080882. PMID: 17229907.
Article8. Slocum JL, Heung M, Pennathur S. 2012; Marking renal injury: can we move beyond serum creatinine? Transl Res. 159:277–89. DOI: 10.1016/j.trsl.2012.01.014. PMID: 22424431. PMCID: PMC3308350.9. Thongprayoon C, Cheungpasitporn W, Srivali N, Ungprasert P, Kittanamongkolchai W, Kashani K. 2016; The impact of fluid balance on diagnosis, staging and prediction of mortality in critically ill patients with acute kidney injury. J Nephrol. 29:221–7. DOI: 10.1007/s40620-015-0211-3. PMID: 26012379.
Article10. Oh DJ. 2020; A long journey for acute kidney injury biomarkers. Ren Fail. 42:154–65. DOI: 10.1080/0886022X.2020.1721300. PMID: 32050834. PMCID: PMC7034110.
Article11. Albert C, Zapf A, Haase M, Röver C, Pickering JW, Albert A, et al. 2020; Neutrophil gelatinase-associated lipocalin measured on clinical laboratory platforms for the prediction of acute kidney injury and the associated need for dialysis therapy: a systematic review and meta-analysis. Am J Kidney Dis. 76:826–41.e1. DOI: 10.1053/j.ajkd.2020.05.015. PMID: 32679151. PMCID: PMC8283708.
Article12. Chen YT, Jenq CC, Hsu CK, Yu YC, Chang CH, Fan PC, et al. 2020; Acute kidney disease and acute kidney injury biomarkers in coronary care unit patients. BMC Nephrol. 21:207. DOI: 10.1186/s12882-020-01872-z. PMID: 32487168. PMCID: PMC7268535.
Article13. Griffin BR, Faubel S, Edelstein CL. 2019; Biomarkers of drug-induced kidney toxicity. Ther Drug Monit. 41:213–26. DOI: 10.1097/FTD.0000000000000589. PMID: 30883514. PMCID: PMC6436396.
Article14. Wołyniec W, Ratkowski W, Renke J, Renke M. 2020; Changes in novel AKI biomarkers after exercise. A systematic review. Int J Mol Sci. 21:1–20. DOI: 10.3390/ijms21165673. PMID: 32784748. PMCID: PMC7461060.
Article15. Chiang TH, Yo CH, Lee GH, Mathew A, Sugaya T, Li WY, et al. 2022; Accuracy of liver-type fatty acid-binding protein in predicting acute kidney injury: a meta-analysis. J Appl Lab Med. 7:421–36. DOI: 10.1093/jalm/jfab092. PMID: 34499739.16. Naruse H, Ishii J, Takahashi H, Kitagawa F, Nishimura H, Kawai H, et al. 2018; Predicting acute kidney injury using urinary liver-type fatty-acid binding protein and serum N-terminal pro-B-type natriuretic peptide levels in patients treated at medical cardiac intensive care units. Crit Care. 22:197. DOI: 10.1186/s13054-018-2120-z. PMID: 30119691. PMCID: PMC6098639.
Article17. Shimoyama T, Sato T, Sakamoto Y, Nagai K, Aoki J, Suda S, et al. 2020; Urinary biomarkers of kidney tubule injury, risk of acute kidney injury, and mortality in patients with acute ischaemic stroke treated at a stroke care unit. Eur J Neurol. 27:2463–72. DOI: 10.1111/ene.14448. PMID: 32697875.
Article18. Duff S, Irwin R, Cote JM, Redahan L, McMahon BA, Marsh B, et al. 2022; Urinary biomarkers predict progression and adverse outcomes of acute kidney injury in critical illness. Nephrol Dial Transplant. 37:1668–78. DOI: 10.1093/ndt/gfab263. PMID: 34491355.
Article19. Schrezenmeier EV, Barasch J, Budde K, Westhoff T, Schmidt-Ott KM. 2017; Biomarkers in acute kidney injury - pathophysiological basis and clinical performance. Acta Physiol (Oxf). 219:554–72. DOI: 10.1111/apha.12764. PMID: 27474473. PMCID: PMC5575831.
Article20. Mebazaa A, Casadio MC, Azoulay E, Guidet B, Jaber S, Levy B, et al. 2015; Post-ICU discharge and outcome: rationale and methods of the French and euRopean Outcome reGistry in Intensive Care Units (FROG-ICU) observational study. BMC Anesthesiol. 15:143. DOI: 10.1186/s12871-015-0129-2. PMID: 26459405. PMCID: PMC4603975.21. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. 1999; A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 130:461–70. DOI: 10.7326/0003-4819-130-6-199903160-00002. PMID: 10075613.
Article22. Ympa YP, Sakr Y, Reinhart K, Vincent JL. 2005; Has mortality from acute renal failure decreased? A systematic review of the literature. Am J Med. 118:827–32. DOI: 10.1016/j.amjmed.2005.01.069. PMID: 16084171.
Article23. Doi K, Negishi K, Ishizu T, Katagiri D, Fujita T, Matsubara T, et al. 2011; Evaluation of new acute kidney injury biomarkers in a mixed intensive care unit. Crit Care Med. 39:2464–9. DOI: 10.1097/CCM.0b013e318225761a. PMID: 21705884.
Article24. Ho J, Tangri N, Komenda P, Kaushal A, Sood M, Brar R, et al. 2015; Urinary, plasma, and serum biomarkers' utility for predicting acute kidney injury associated with cardiac surgery in adults: a meta-analysis. Am J Kidney Dis. 66:993–1005. DOI: 10.1053/j.ajkd.2015.06.018. PMID: 26253993.
Article25. Siew ED, Ware LB, Bian A, Shintani A, Eden SK, Wickersham N, et al. 2013; Distinct injury markers for the early detection and prognosis of incident acute kidney injury in critically ill adults with preserved kidney function. Kidney Int. 84:786–94. DOI: 10.1038/ki.2013.174. PMID: 23698227. PMCID: PMC3788840.
Article26. Nickolas TL, Schmidt-Ott KM, Canetta P, Forster C, Singer E, Sise M, et al. 2012; Diagnostic and prognostic stratification in the emergency department using urinary biomarkers of nephron damage: a multicenter prospective cohort study. J Am Coll Cardiol. 59:246–55. DOI: 10.1016/j.jacc.2011.10.854. PMID: 22240130. PMCID: PMC3487165.27. Hall IE, Coca SG, Perazella MA, Eko UU, Luciano RL, Peter PR, et al. 2011; Risk of poor outcomes with novel and traditional biomarkers at clinical AKI diagnosis. Clin J Am Soc Nephrol. 6:2740–9. DOI: 10.2215/CJN.04960511. PMID: 22034509. PMCID: PMC3255362.
Article28. Singer E, Elger A, Elitok S, Kettritz R, Nickolas TL, Barasch J, et al. 2011; Urinary neutrophil gelatinase-associated lipocalin distinguishes pre-renal from intrinsic renal failure and predicts outcomes. Kidney Int. 80:405–14. DOI: 10.1038/ki.2011.41. PMID: 21412214. PMCID: PMC3870593.
Article29. Ralib AM, Pickering JW, Shaw GM, Devarajan P, Edelstein CL, Bonventre J V, et al. 2012; Test characteristics of urinary biomarkers depend on quantitation method in acute kidney injury. J Am Soc Nephrol. 23:322–33. DOI: 10.1681/ASN.2011040325. PMID: 22095948. PMCID: PMC3269182.
Article30. Coca SG, Garg AX, Thiessen-Philbrook H, Koyner JL, Patel UD, Krumholz HM, et al. 2014; Urinary biomarkers of AKI and mortality 3 years after cardiac surgery. J Am Soc Nephrol. 25:1063–71. DOI: 10.1681/ASN.2013070742. PMID: 24357673. PMCID: PMC4005309.
Article31. Pan HC, Huang TTM, Huang CT, Sun CY, Chen YM, Wu VC. 2022; Urinary biomarkers can predict weaning from acute dialysis therapy in critically ill patients. Arch Pathol Lab Med. 146:1353–63. DOI: 10.5858/arpa.2021-0411-OA. PMID: 35311928.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Urinary Liver-Type Fatty Acid-Binding Protein in Critically Ill Patients
- The associations of Urinary Neutrophil Gelatinaseassociated Lipocalin (NGAL) and Liver-type Fatty Acidbinding Protein (L-FABP) Levels with Hematuria in Children and Adolescents
- New Biomarkers of Acute Kidney Injury and the Cardio-renal Syndrome
- Intra-abdominal hypertension does not predict renal recovery or in-hospital mortality in critically ill patients with acute kidney injury
- Acute Kidney Injury after Using Contrast during Cardiac Catheterization in Children with Heart Disease