Ann Rehabil Med.
2024 Feb;48(1):50-56. 10.5535/arm.23127.
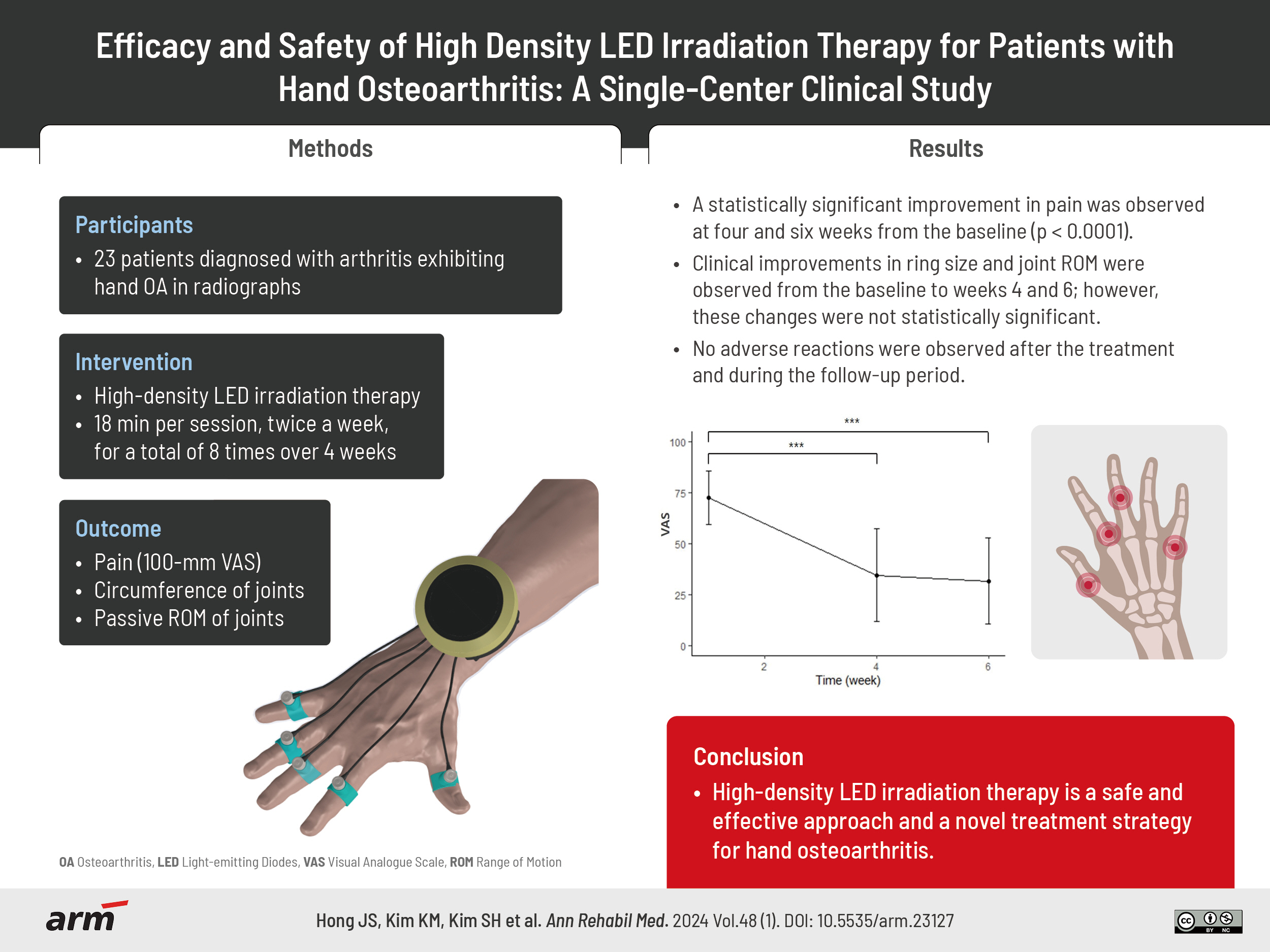
Efficacy and Safety of High Density LED Irradiation Therapy for Patients With Hand Osteoarthritis: A Single-Center Clinical Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Yonsei Joon Rehabilitation Clinic, Wonju, Korea
- 3Department of Medical Informatics and Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Department of Precision Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2553161
- DOI: http://doi.org/10.5535/arm.23127
Abstract
Objective
To assess the safety and effectiveness of high-density light-emitting diode (LED) irradiation therapy in patients with hand osteoarthritis (OA) and compare the pre- and post-intervention symptoms.
Methods
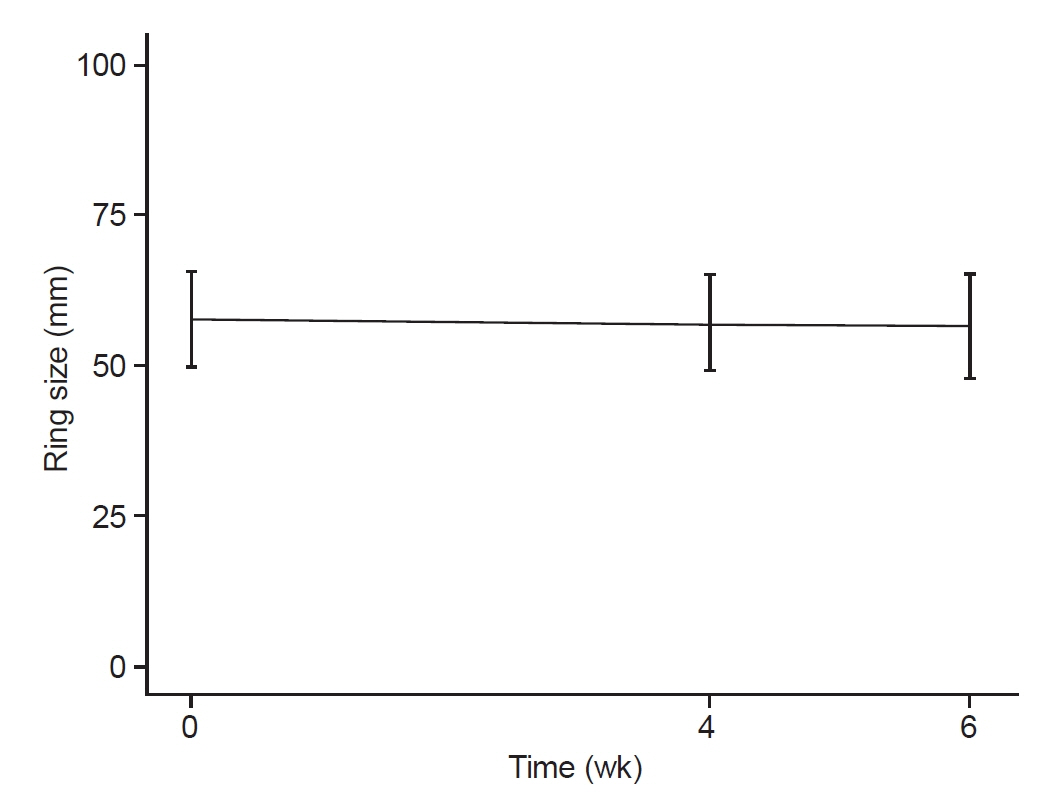
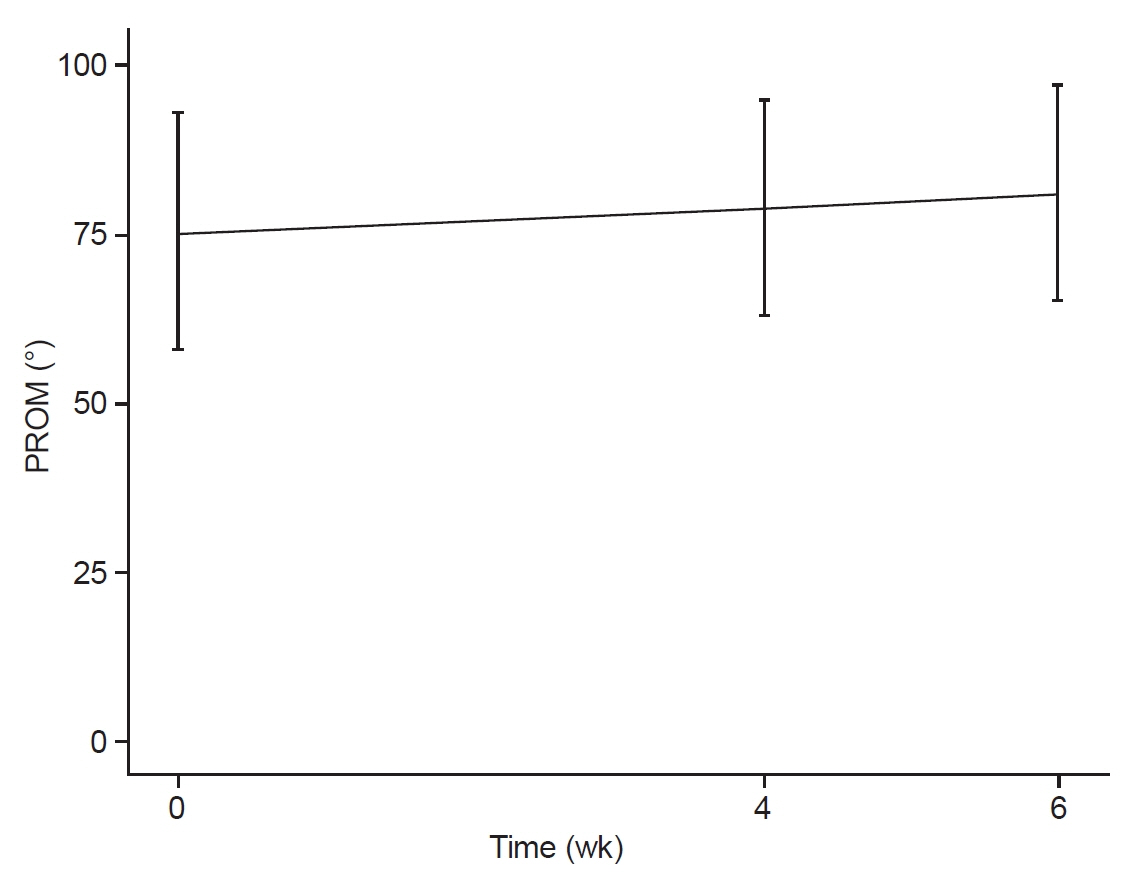
Twenty-three patients with hand OA underwent eight sessions of high-density LED irradiation therapy directed at the five most painful areas in the finger joints. Each session lasted for 18 minutes; and the sessions were conducted twice a week, for 4 weeks. We evaluated the degree of pain using the visual analogue scale, ring size, and passive range of motion (flexion+extension) for two most painful joints from the baseline to post-therapy (weeks 4 and 6).
Results
High-density LED irradiation therapy significantly reduced the pain posttreatment compared with that observed at the baseline (p<0.001). Although improvements were observed in ring size and joint range of motion at 4 and 6 weeks, they were not statistically significant (p>0.05). No adverse events were observed.
Conclusion
We examined the safety and effectiveness of high-density LED irradiation therapy in reducing pain and hand swelling and improving joint mobility in patients with hand OA. These results suggest that high-density LED irradiation therapy has the potential to be an important strategy for managing hand OA.
Keyword
Figure
Cited by 2 articles
-
Letter to the Editor: Efficacy and Safety of High Density LED Irradiation Therapy for Patients With Hand Osteoarthritis: A Single-Center Clinical Study
Vanshika Agarwal, Jeyanthi. S, Adarsh Sharma
Ann Rehabil Med. 2025;49(1):1-2. doi: 10.5535/arm.240063.Response: Efficacy and Safety of High Density LED Irradiation Therapy for Patients With Hand Osteoarthritis: A Single-Center Clinical Study (
Ann Rehabil Med 2024;48:50-6)
Jiseon Hong
Ann Rehabil Med. 2025;49(1):3-4. doi: 10.5535/arm.240082.
Reference
-
1. Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage. 2022; 30:184–95.2. Martel-Pelletier J, Barr AJ, Cicuttini FM, Conaghan PG, Cooper C, Goldring MB, et al. Osteoarthritis. Nat Rev Dis Primers. 2016; 2:16072.3. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019; 393:1745–59.4. Xia B, Di Chen, Zhang J, Hu S, Jin H, Tong P. Osteoarthritis pathogenesis: a review of molecular mechanisms. Calcif Tissue Int. 2014; 95:495–505.5. Yu H, Huang T, Lu WW, Tong L, Chen D. Osteoarthritis pain. Int J Mol Sci. 2022; 23:4642.6. Abramoff B, Caldera FE. Osteoarthritis: pathology, diagnosis, and treatment options. Med Clin North Am. 2020; 104:293–311.7. Martel-Pelletier J, Boileau C, Pelletier JP, Roughley PJ. Cartilage in normal and osteoarthritis conditions. Best Pract Res Clin Rheumatol. 2008; 22:351–84.8. Plotz B, Bomfim F, Sohail MA, Samuels J. Current epidemiology and risk factors for the development of hand osteoarthritis. Curr Rheumatol Rep. 2021; 23:61.9. Baltzer AW, Ostapczuk MS, Stosch D. Positive effects of low level laser therapy (LLLT) on Bouchard’s and Heberden’s osteoarthritis. Lasers Surg Med. 2016; 48:498–504.10. Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. J Hand Ther. 2010; 23:334–50; quiz 51.11. Kroon FP, Rubio R, Schoones JW, Kloppenburg M. Intra-articular therapies in the treatment of hand osteoarthritis: a systematic literature review. Drugs Aging. 2016; 33:119–33.12. Zhang W, Doherty M, Leeb BF, Alekseeva L, Arden NK, Bijlsma JW, et al. EULAR evidence based recommendations for the management of hand osteoarthritis: report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis. 2007; 66:377–88.13. Bindu S, Mazumder S, Bandyopadhyay U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: a current perspective. Biochem Pharmacol. 2020; 180:114147.14. Debono DJ, Hoeksema LJ, Hobbs RD. Caring for patients with chronic pain: pearls and pitfalls. J Am Osteopath Assoc. 2013; 113:620–7.15. Grillet B, Dequeker J. Intra-articular steroid injection. A risk-benefit assessment. Drug Saf. 1990; 5:205–11.16. Kim H, Sung YK. Pharmacological treatment of osteoarthritis. J Korean Med Assoc. 2018; 61:623–9.17. Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012; 64:465–74.18. Adams JE. Surgical management of osteoarthritis of the hand and wrist. J Hand Ther. 2022; 35:418–27.19. Kloppenburg M, Kroon FP, Blanco FJ, Doherty M, Dziedzic KS, Greibrokk E, et al. 2018 update of the EULAR recommendations for the management of hand osteoarthritis. Ann Rheum Dis. 2019; 78:16–24.20. DE Oliveira MF, Johnson DS, Demchak T, Tomazoni SS, Leal-Junior EC. Low-intensity LASER and LED (photobiomodulation therapy) for pain control of the most common musculoskeletal conditions. Eur J Phys Rehabil Med. 2022; 58:282–9.21. Opel DR, Hagstrom E, Pace AK, Sisto K, Hirano-Ali SA, Desai S, et al. Light-emitting diodes: a brief review and clinical experience. J Clin Aesthet Dermatol. 2015; 8:36–44.22. Goldberg DJ, Amin S, Russell BA, Phelps R, Kellett N, Reilly LA. Combined 633-nm and 830-nm led treatment of photoaging skin. J Drugs Dermatol. 2006; 5:748–53.23. Russell BA, Kellett N, Reilly LR. A study to determine the efficacy of combination LED light therapy (633 nm and 830 nm) in facial skin rejuvenation. J Cosmet Laser Ther. 2005; 7:196–200.24. Hansen EH. [Measurement and description of joint mobility by the neutral zero method]. Ugeskr Laeger. 1975; 137:2822–5. Danish.25. Kurtti A, Nguyen JK, Weedon J, Mamalis A, Lai Y, Masub N, et al. Light emitting diode-red light for reduction of post-surgical scarring: results from a dose-ranging, split-face, randomized controlled trial. J Biophotonics. 2021; 14:e202100073.26. Ablon G. Phototherapy with light emitting diodes: treating a broad range of medical and aesthetic conditions in dermatology. J Clin Aesthet Dermatol. 2018; 11:21–7.27. Goldberg DJ, Russell BA. Combination blue (415 nm) and red (633 nm) LED phototherapy in the treatment of mild to severe acne vulgaris. J Cosmet Laser Ther. 2006; 8:71–5.28. Barolet D. Light-emitting diodes (LEDs) in dermatology. Semin Cutan Med Surg. 2008; 27:227–38.29. Mester E, Spiry T, Szende B, Tota JG. Effect of laser rays on wound healing. Am J Surg. 1971; 122:532–5.30. Xu GZ, Jia J, Jin L, Li JH, Wang ZY, Cao DY. Low-level laser therapy for temporomandibular disorders: a systematic review with meta-analysis. Pain Res Manag. 2018; 2018:4230583.31. Baxter GD, Liu L, Petrich S, Gisselman AS, Chapple C, Anders JJ, et al. Low level laser therapy (Photobiomodulation therapy) for breast cancer-related lymphedema: a systematic review. BMC Cancer. 2017; 17:833.32. Chen FR, Manzi JE, Mehta N, Gulati A, Jones M. A review of laser therapy and low-intensity ultrasound for chronic pain states. Curr Pain Headache Rep. 2022; 26:57–63.33. Heiskanen V, Hamblin MR. Photobiomodulation: lasers vs. light emitting diodes? Photochem Photobiol Sci 2018;17:1003-17. Erratum in: Photochem Photobiol Sci. 2018; 18:259.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor: Efficacy and Safety of High Density LED Irradiation Therapy for Patients With Hand Osteoarthritis: A Single-Center Clinical Study
- Response: Efficacy and Safety of High Density LED Irradiation Therapy for Patients With Hand Osteoarthritis: A Single-Center Clinical Study (Ann Rehabil Med 2024;48:50-6)
- Exploring the Safety and Efficacy of Organic Light-Emitting Diode in Skin Rejuvenation and Wound Healing
- In vitro investigation of the antibacterial and anti-inflammatory effects of LED irradiation
- Prevention of Heterotopic Bone Formation after Total Hip Arthroplasty in High Risk Patient with Radiation Therapy