Korean J Orthod.
2024 Jan;54(1):59-68. 10.4041/kjod23.090.
Long-term effects of maxillary skeletal expander treatment on functional breathing
- Affiliations
-
- 1Center for Health Science, Section of Orthodontics, UCLA School of Dentistry, Los Angeles, CA, USA
- 2Private Practice, Houston, TX, USA
- 3Department of Orthodontics, Rey Juan Carlos University, Madrid, Spain
- 4Department of Orthodontics, State University of New York, Buffalo, NY, USA
- 5Orthodontic and Craniofacial Development Research, Forsyth Institute, Cambridge, MA, USA
- 6Department of Orthodontics, Ajou University, School of Medicine, Suwon, Korea
- KMID: 2551475
- DOI: http://doi.org/10.4041/kjod23.090
Abstract
Objective
To investigate the long-term effects of maxillary skeletal expander (MSE) treatment on functional breathing.
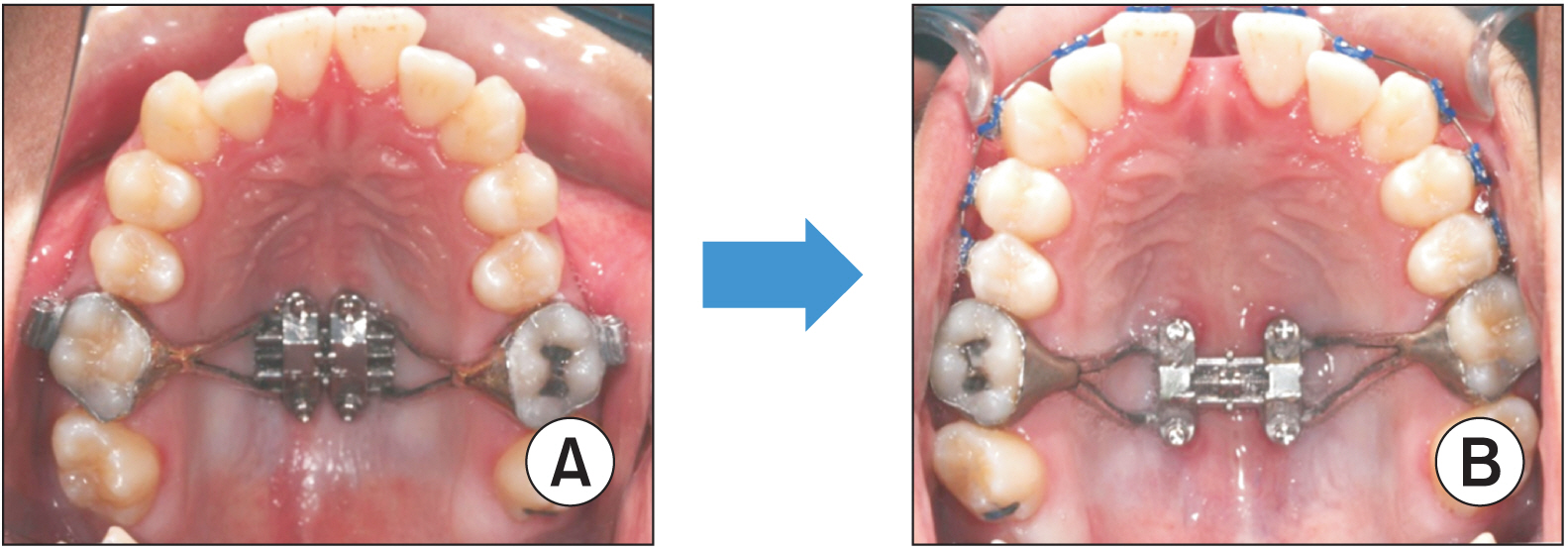
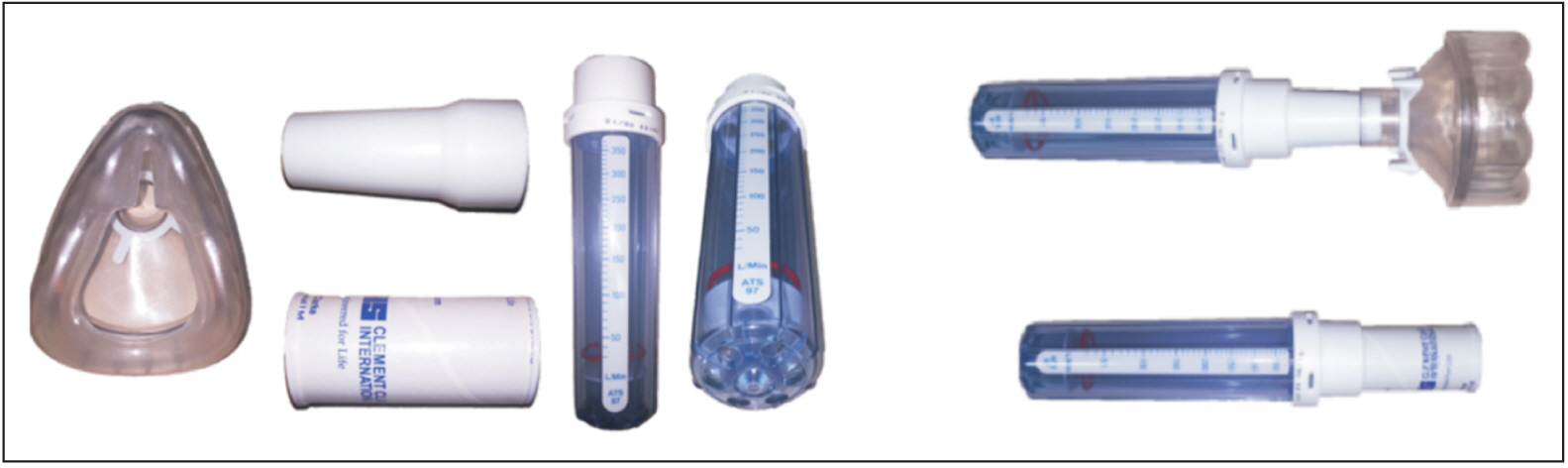
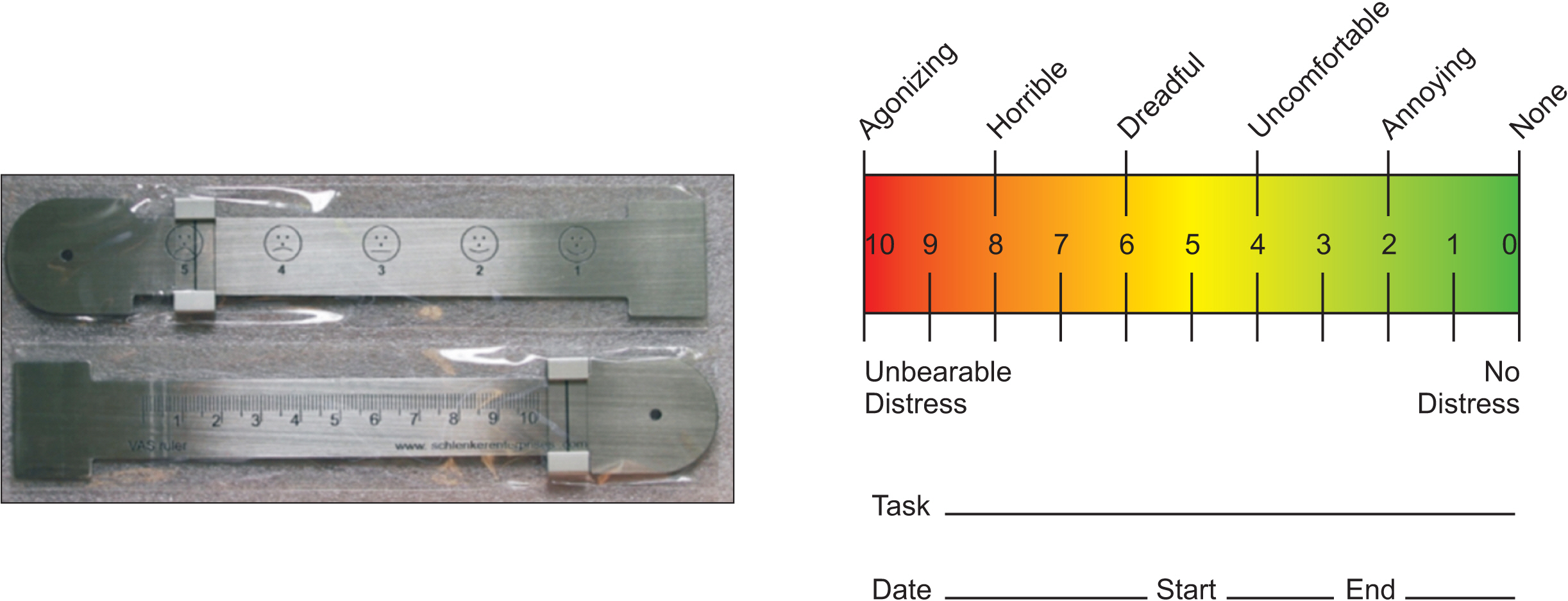
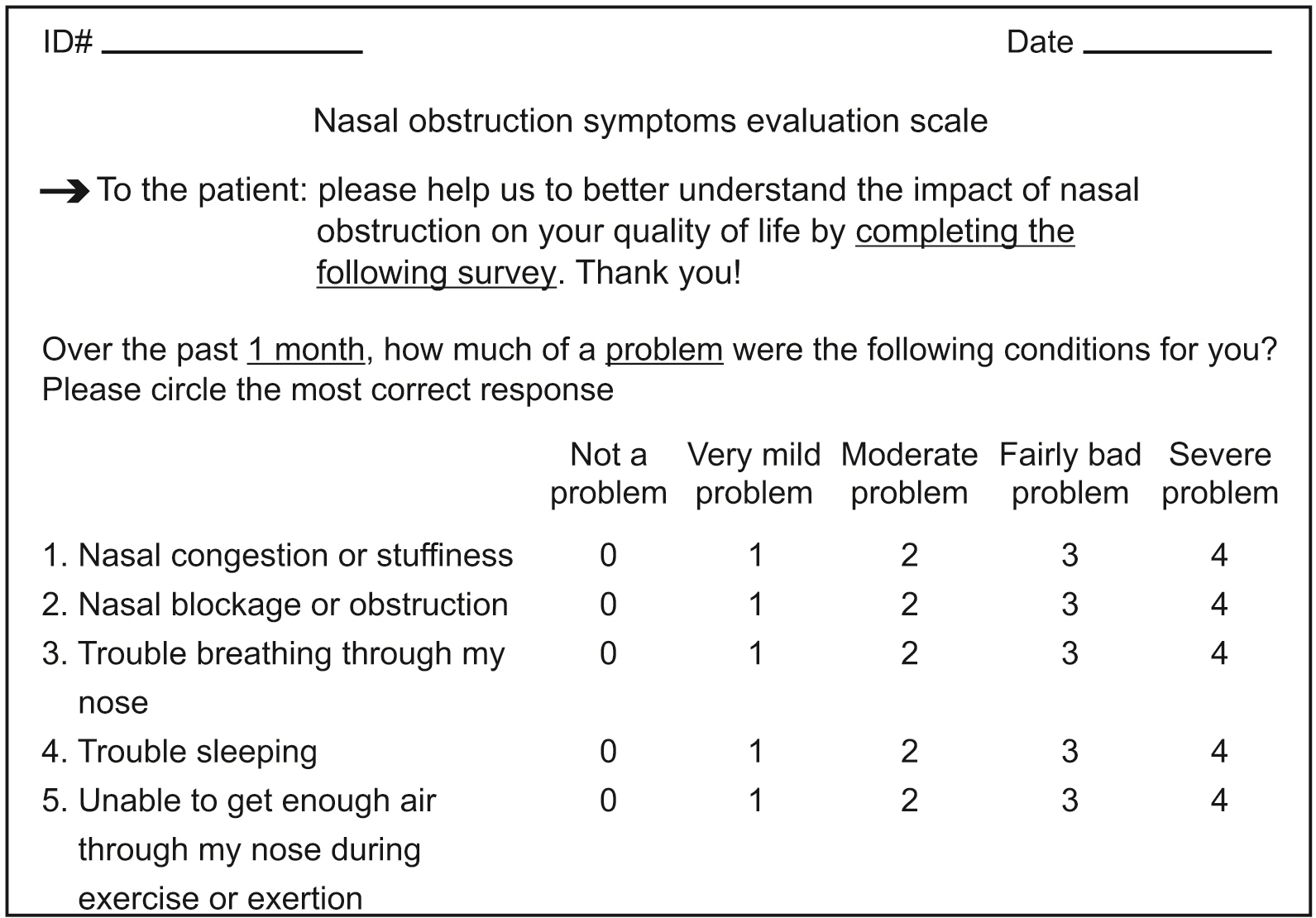
Methods
Objective measures of breathing, the peak nasal inspiratory flow (PNIF), and peak oral inspiratory flow (POIF), and subjective measures of breathing, the visual analog scale (VAS) and nasal obstruction symptom evaluation (NOSE) survey, were used to investigate the long-term effects of MSE in functional breathing. Seventeen patients, mean age 19.4 ± 3.9 years treated at the UCLA Orthodontics Clinic were assessed on their functional breathing at 3 timepoints: pre-expansion (T0), post-expansion (T1), and post-orthodontic treatment (T2). Results: Immediately after expansion (T1), all the objective functional breathing values were significantly increased in comparison to T0 (P < 0.05). The VAS total, VAS right and VAS left were significantly lower at T1 in comparison to T0 (P < 0.05). At 26.8 ± 3.9 months after MSE expansion (T2), PNIF total, PNIF right, PNIF left, and POIF were significantly higher when compared to T0 (P < 0.05). Also, VAS total, VAS right and VAS left were significantly lower at T2 when compared to T0 (P < 0.05). Additionally, there was a positive correlation between PNIF and the magnitude of expansion at anterior nasal spine and zygomaticomaxillary point (ZMA). There was a positive correlation between total VAS and the magnitude of expansion at the ZMA. There were no significant changes for the NOSE subjective breathing measurement at all time comparisons. Conclusions: Overall, MSE treatment produces an increased objective and subjective airway improvement that continues to remain stable in the long-term post expansion.
Keyword
Figure
Reference
-
1. Betts NJ, Vanarsdall RL, Barber HD, Higgins-Barber K, Fonseca RJ. 1995; Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 10:75–96. https://pubmed.ncbi.nlm.nih.gov/9082002/.2. Brunetto DP, Sant'Anna EF, Machado AW, Moon W. 2017; Non-surgical treatment of transverse deficiency in adults using Microimplant-assisted Rapid Palatal Expansion (MARPE). Dental Press J Orthod. 22:110–25. https://doi.org/10.1590/2177-6709.22.1.110-125.sar. DOI: 10.1590/2177-6709.22.1.110-125.sar. PMID: 28444019. PMCID: PMC5398849.3. da Silva Filho OG, Santamaria M Jr, Capelozza Filho L. 2007; Epidemiology of posterior crossbite in the primary dentition. J Clin Pediatr Dent. 32:73–8. https://doi.org/10.17796/jcpd.32.1.h53g027713432102. DOI: 10.17796/jcpd.32.1.h53g027713432102. PMID: 18274476.4. McNamara JA Jr, Lione R, Franchi L, Angelieri F, Cevidanes LH, Darendeliler MA, et al. 2015; The role of rapid maxillary expansion in the promotion of oral and general health. Prog Orthod. 16:33. https://doi.org/10.1186/s40510-015-0105-x. DOI: 10.1186/s40510-015-0105-x. PMID: 26446931. PMCID: PMC4596248.5. Pereira-Filho VA, Monnazzi MS, Gabrielli MA, Spin-Neto R, Watanabe ER, Gimenez CM, et al. 2014; Volumetric upper airway assessment in patients with transverse maxillary deficiency after surgically assisted rapid maxillary expansion. Int J Oral Maxillofac Surg. 43:581–6. https://doi.org/10.1016/j.ijom.2013.11.002. DOI: 10.1016/j.ijom.2013.11.002. PMID: 24361243.6. Franklin KA, Lindberg E. 2015; Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. 7:1311–22. https://doi.org/10.3978/j.issn.2072-1439.2015.06.11. DOI: 10.3390/books978-3-03936-079-6.7. Tarasiuk A, Reuveni H. 2013; The economic impact of obstructive sleep apnea. Curr Opin Pulm Med. 19:639–44. 13e3283659e1e. DOI: 10.1097/MCP.0b013e3283659e1e. PMID: 24060978.8. Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. 2000; Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 283:1829–36. https://doi.org/10.1001/jama.283.14.1829. Erratum in: JAMA 2002;288: 1985. DOI: 10.1001/jama.283.14.1829. PMID: 10770144.9. Drager LF, Bortolotto LA, Lorenzi MC, Figueiredo AC, Krieger EM, Lorenzi-Filho G. 2005; Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med. 172:613–8. https://doi.org/10.1164/rccm.200503-340OC. DOI: 10.1164/rccm.200503-340OC. PMID: 15901608.10. Drager LF, Lopes HF, Maki-Nunes C, Trombetta IC, Toschi-Dias E, Alves MJ, et al. 2010; The impact of obstructive sleep apnea on metabolic and inflammatory markers in consecutive patients with metabolic syndrome. PLoS One. 5:e12065. https://doi.org/10.1371/journal.pone.0012065. DOI: 10.1371/journal.pone.0012065. PMID: 20711453. PMCID: PMC2920316. PMID: 83cf703e42cf4ea38688fa95447f960c.11. Almuzian M, Ju X, Almukhtar A, Ayoub A, Al-Muzian L, McDonald JP. 2018; Does rapid maxillary expansion affect nasopharyngeal airway? A prospective Cone Beam Computerised Tomography (CBCT) based study. Surgeon. 16:1–11. https://doi.org/10.1016/j.surge.2015.12.006. DOI: 10.1016/j.surge.2015.12.006. PMID: 26827275.12. Michels Dde S, Rodrigues Ada M, Nakanishi M, Sampaio AL, Venosa AR. 2014; Nasal involvement in obstructive sleep apnea syndrome. Int J Otolaryngol. 2014:717419. https://doi.org/10.1155/2014/717419. DOI: 10.1155/2014/717419. PMID: 25548569. PMCID: PMC4273597. PMID: cdb1d3937afd49da9b372389767f6aec.13. Douglas NJ, White DP, Weil JV, Zwillich CW. 1983; Effect of breathing route on ventilation and ventilatory drive. Respir Physiol. 51:209–18. https://doi.org/10.1016/0034-5687(83)90041-5. DOI: 10.1016/0034-5687(83)90041-5. PMID: 6844756.14. Fastuca R, Meneghel M, Zecca PA, Mangano F, Antonello M, Nucera R, et al. 2015; Multimodal airway evaluation in growing patients after rapid maxillary expansion. Eur J Paediatr Dent. 16:129–34. https://pubmed.ncbi.nlm.nih.gov/26147819/.15. Fastuca R, Perinetti G, Zecca PA, Nucera R, Caprioglio A. 2015; Airway compartments volume and oxygen saturation changes after rapid maxillary expansion: a longitudinal correlation study. Angle Orthod. 85:955–61. https://doi.org/10.2319/072014-504.1. DOI: 10.2319/072014-504.1. PMID: 26516709. PMCID: PMC8612044.16. Iwasaki T, Saitoh I, Takemoto Y, Inada E, Kanomi R, Hayasaki H, et al. 2012; Improvement of nasal airway ventilation after rapid maxillary expansion evaluated with computational fluid dynamics. Am J Orthod Dentofacial Orthop. 141:269–78. https://doi.org/10.1016/j.ajodo.2011.08.025. DOI: 10.1016/j.ajodo.2011.08.025. PMID: 22381487.17. Gurel HG, Memili B, Erkan M, Sukurica Y. 2010; Long-term effects of rapid maxillary expansion followed by fixed appliances. Angle Orthod. 80:5–9. https://doi.org/10.2319/011209-22.1. DOI: 10.2319/011209-22.1. PMID: 19852633. PMCID: PMC8978752.18. Haas AJ. 1965; The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 35:200–17. https://pubmed.ncbi.nlm.nih.gov/14331020/.19. Buck LM, Dalci O, Darendeliler MA, Papadopoulou AK. 2016; Effect of surgically assisted rapid maxillary expansion on upper airway volume: a systematic review. J Oral Maxillofac Surg. 74:1025–43. https://doi.org/10.1016/j.joms.2015.11.035. DOI: 10.1016/j.joms.2015.11.035. PMID: 26778518.20. Vinha PP, Faria AC, Xavier SP, Christino M, de Mello-Filho FV. 2016; Enlargement of the pharynx resulting from surgically assisted rapid maxillary expansion. J Oral Maxillofac Surg. 74:369–79. https://doi.org/10.1016/j.joms.2015.06.157. DOI: 10.1016/j.joms.2015.06.157. PMID: 26164086.21. Zambon CE, Ceccheti MM, Utumi ER, Pinna FR, Machado GG, Peres MP, et al. 2012; Orthodontic measurements and nasal respiratory function after surgically assisted rapid maxillary expansion: an acoustic rhinometry and rhinomanometry study. Int J Oral Maxillofac Surg. 41:1120–6. https://doi.org/10.1016/j.ijom.2011.12.037. DOI: 10.1016/j.ijom.2011.12.037. PMID: 22520723.22. Paredes N, Colak O, Sfogliano L, Elkenawy I, Fijany L, Fraser A, et al. 2020; Differential assessment of skeletal, alveolar, and dental components induced by microimplant-supported midfacial skeletal expander (MSE), utilizing novel angular measurements from the fulcrum. Prog Orthod. 21:18. https://doi.org/10.1186/s40510-020-00320-w. DOI: 10.1186/s40510-020-00320-w. PMID: 32656601. PMCID: PMC7355053. PMID: 3f36d2bd852c4ec9aa3cacd7ca6825e4.23. Cantarella D, Dominguez-Mompell R, Moschik C, Mallya SM, Pan HC, Alkahtani MR, et al. 2018; Midfacial changes in the coronal plane induced by microimplant-supported skeletal expander, studied with cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 154:337–45. https://doi.org/10.1016/j.ajodo.2017.11.033. DOI: 10.1016/j.ajodo.2017.11.033. PMID: 30173836.24. Colak O, Paredes NA, Elkenawy I, Torres M, Bui J, Jahangiri S, et al. 2020; Tomographic assessment of palatal suture opening pattern and pterygopalatine suture disarticulation in the axial plane after midfacial skeletal expansion. Prog Orthod. 21:21. https://doi.org/10.1186/s40510-020-00321-9. DOI: 10.1186/s40510-020-00321-9. PMID: 32686018. PMCID: PMC7370251. PMID: d48b855ae99f48ea93dcefe40cb63710.25. MacGinnis M, Chu H, Youssef G, Wu KW, Machado AW, Moon W. 2014; The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex--a finite element method (FEM) analysis. Prog Orthod. 15:52. https://doi.org/10.1186/s40510-014-0052-y. DOI: 10.1186/s40510-014-0052-y. PMID: 25242527. PMCID: PMC4148550.26. Kabalan O, Gordon J, Heo G, Lagravère MO. 2015; Nasal airway changes in bone-borne and tooth-borne rapid maxillary expansion treatments. Int Orthod. 13:1–15. https://doi.org/10.1016/j.ortho.2014.12.011. DOI: 10.1016/j.ortho.2014.12.011. PMID: 25665908.27. Jose J, Ell SR. 2003; The association of subjective nasal patency with peak inspiratory nasal flow in a large healthy population. Clin Otolaryngol Allied Sci. 28:352–4. https://doi.org/10.1046/j.1365-2273.2003.00722.x. DOI: 10.1046/j.1365-2273.2003.00722.x. PMID: 12871251.28. Teixeira RUF, Zappelini CEM, Alves FS, da Costa EA. 2011; Peak nasal inspiratory flow evaluation as an objective method of measuring nasal airflow. Braz J Otorhinolaryngol. 77:473–80. https://doi.org/10.1590/S1808-86942011000400011. DOI: 10.1590/S1808-86942011000400011. PMID: 21860974. PMCID: PMC9450779. PMID: 717c9069290d47ed969676d1e965a4e8.29. Ishii L, Godoy A, Ishman SL, Gourin CG, Ishii M. 2011; The nasal obstruction symptom evaluation survey as a screening tool for obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 137:119–23. https://doi.org/10.1001/archoto.2010.251. DOI: 10.1001/archoto.2010.251. PMID: 21339396.30. 2005. Visual analog scale VAS rulers [Internet]. HugeDomains;Colorado: Available from: http://www.schlenkerenterprises.com/vas_medical_rulers.htm. cited 2023 Dec 21.31. Singh AP. 2012. Visual analog scale and color analog scale for pain [Internet]. Bone and Spine;Punjab: Available from: http://boneandspine.com/visual-analog-scale-for-pain. cited 2023 Oct 30.32. Lipan MJ, Most SP. 2013; Development of a severity classification system for subjective nasal obstruction. JAMA Facial Plast Surg. 15:358–61. https://doi.org/10.1001/jamafacial.2013.344. DOI: 10.1001/jamafacial.2013.344. PMID: 23846399.33. Elkenawy I, Fijany L, Colak O, Paredes NA, Gargoum A, Abedini S, et al. 2020; An assessment of the magnitude, parallelism, and asymmetry of micro-implant-assisted rapid maxillary expansion in non-growing patients. Prog Orthod. 21:42. https://doi.org/10.1186/s40510-020-00342-4. DOI: 10.1186/s40510-020-00342-4. PMID: 33225406. PMCID: PMC7680816.34. Kara M, Erdoğan H, Güçlü O, Sahin H, Dereköy FS. 2016; Evaluation of sleep quality in patients with nasal septal deviation via the Pittsburgh Sleep Quality Index. J Craniofac Surg. 27:1738–40. https://doi.org/10.1097/SCS.0000000000003008. DOI: 10.1097/SCS.0000000000003008. PMID: 27536915.35. Zhang B. 2018. Functional breathing improvement following treatment with maxillary skeletal expander [Master's thesis]. University of California, Los Angeles;Los Angeles: https://escholarship.org/uc/item/2c05r669.36. Cistulli PA, Palmisano RG, Poole MD. 1998; Treatment of obstructive sleep apnea syndrome by rapid maxillary expansion. Sleep. 21:831–5. https://doi.org/10.1093/sleep/21.8.831. DOI: 10.1093/sleep/21.8.831. PMID: 9871945.37. Tome W, Moon W. 2021; The prevalence of posterior tongue tie in patients with transverse maxillary deficiency. Aust Orthod J. 37:294–300. https://doi.org/10.21307/aoj-2021.033. DOI: 10.21307/aoj-2021.033. PMID: 49f4419692e34a479c03eebf7a216e2b.
- Full Text Links
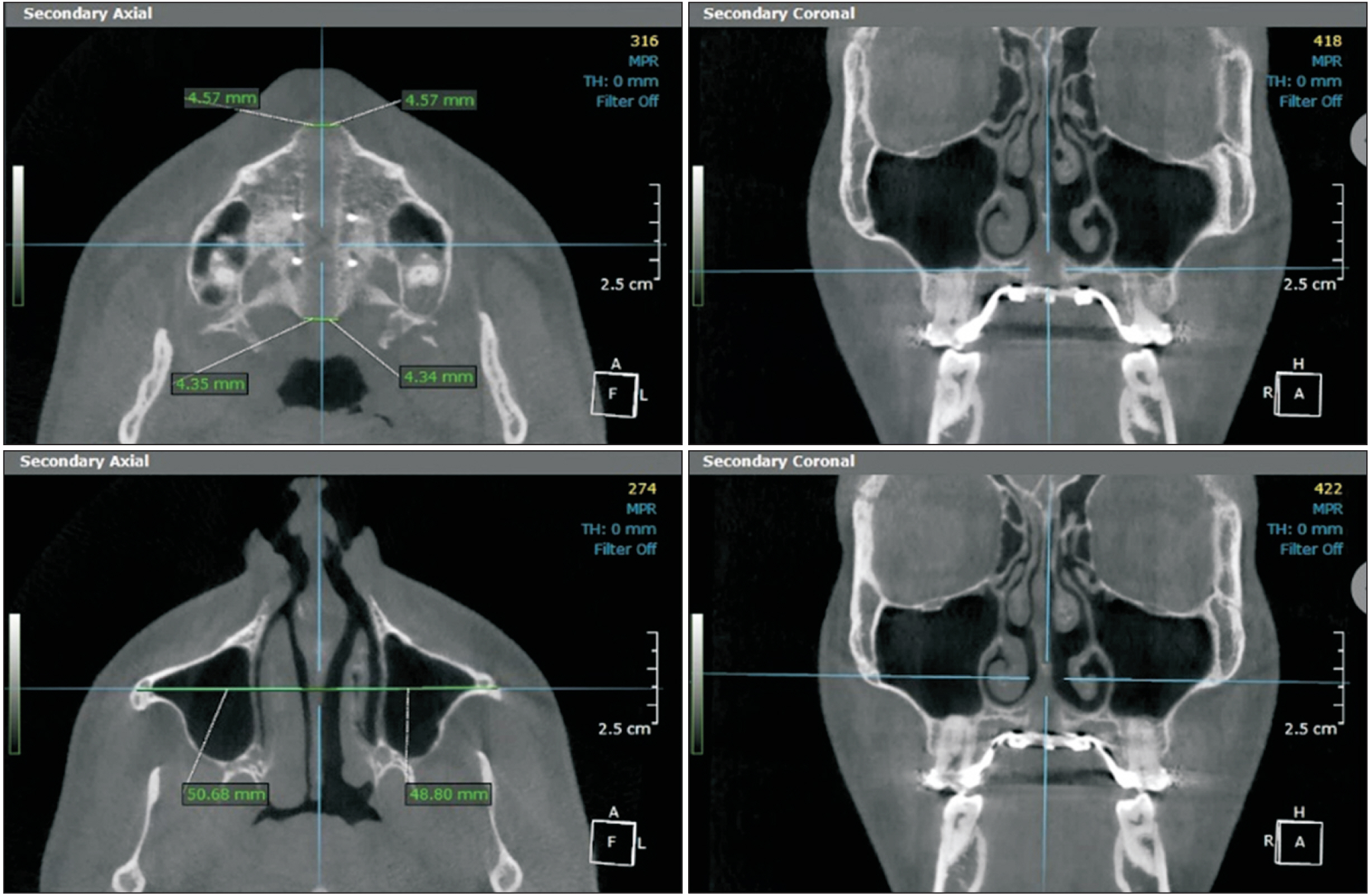
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of bone-borne maxillary skeletal expanders on cranial and circummaxillary sutures: A cone-beam computed tomography study
- Long-term structural and functional nasomaxillary evolution of children with mouth-breathing after rapid maxillary expansion: An 8-year follow-up study
- Does surgically assisted maxillary protraction with skeletal anchorage and Class III elastics affect the pharyngeal airway? A retrospective, long-term study
- Pattern of microimplant displacement during maxillary skeletal expander treatment: A cone-beam computed tomography study
- Clinical application of maxillary tissue bone-borne expander and biocreative reverse curve system in the orthodontic retreatment of severe anterior open bite with transverse discrepancy: A case report