J Korean Med Sci.
2024 Jan;39(1):e2. 10.3346/jkms.2024.39.e2.
The Association Between InterHospital Transfers and the Prognosis of Pediatric Injury in the Emergency Department
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Emergency Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 3Disaster Medicine Research Center, Seoul National University Medical Research Center, Seoul, Korea
- 4Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2550792
- DOI: http://doi.org/10.3346/jkms.2024.39.e2
Abstract
- Background
Inter-hospital transfers of severely injured patients are inevitable due to limited resources. We investigated the association between inter-hospital transfer and the prognosis of pediatric injury using the Korean multi-institutional injury registry.
Methods
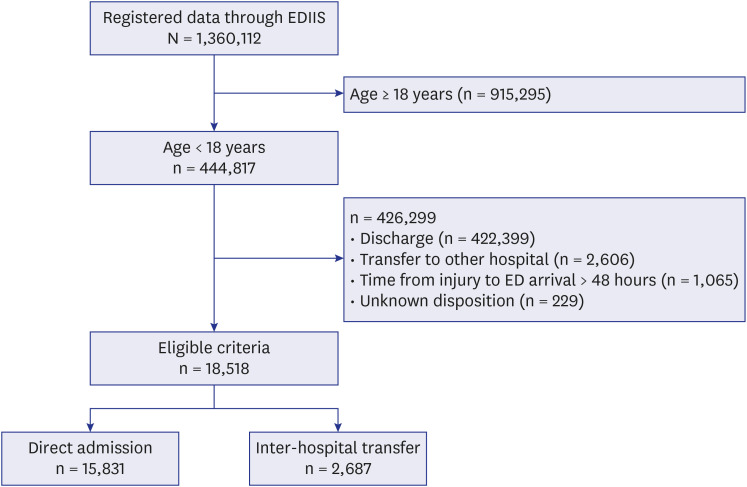
This retrospective observational study was conducted from January 2013 to December 2017; data for hospitalized subjects aged < 18 years were extracted from the Emergency Department-based Injury in Depth Surveillance database, in which 22 hospitals are participating as of 2022. The survival rates of the direct transfer group and the interhospital transfer group were compared, and risk factors affecting 30-day mortality and 72-hour mortality were analyzed.
Results
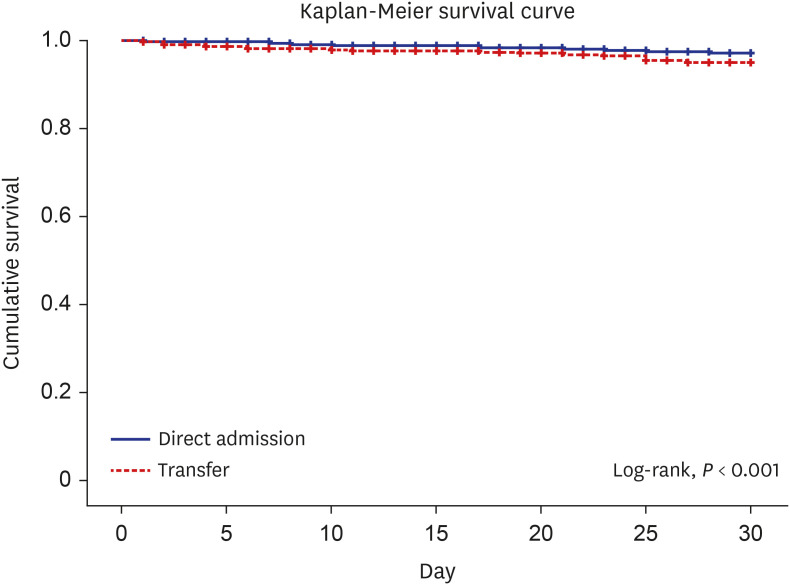
The total number of study subjects was 18,518, and the transfer rate between hospitals was 14.5%. The overall mortality rate was 2.3% (n = 422), the 72-hour mortality was 1.7% (n = 315) and the 30-day mortality rate was 2.2% (n = 407). The Kaplan-Meier survival curve revealed a lower survival rate in the inter-hospital transfer group than in the direct visit group (log-rank, P < 0.001). Cox proportional hazards regression analysis showed that interhospital transfer group had a higher 30-day mortality rate and 72-hour mortality (hazard ratio [HR], 1.681; 95% confidence interval [CI], 1.232–2.294 and HR, 1.951; 95% CI, 1.299–2.930) than direct visit group when adjusting for age, sex, injury severity, and head injury.
Conclusion
Among the pediatric injured patients requiring hospitalization, inter-hospital transfer in the emergency department was associated with the 30-day mortality rate and 72-hour mortality rate in Korea.
Keyword
Figure
Reference
-
1. Yeon GM, Hong YR, Kong SG. Nonfatal injuries in Korean children and adolescents, 2007-2018. Clin Exp Pediatr. 2022; 65(4):194–200. PMID: 34530522.2. Statistics Korea. Cause of death, number of deaths by age, mortality rate. Accessed February 28, 2023. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E01&conn_path=I2 .3. Korea Disease Control and Prevention Agency (KDCA). National Injury Fact Book (2018-2019). Accessed January 7, 2023. http://www.kdca.go.kr/contents.es?mid=a20601030600 .4. Kim H, Jung KY, Kim SP, Kim SH, Noh H, Jang HY, et al. Changes in preventable death rates and traumatic care systems in Korea. J Korean Soc Emerg Med. 2012; 23(2):189–197.5. Kwon J, Lee M, Moon J, Huh Y, Song S, Kim S, et al. National follow-up survey of preventable trauma death rate in Korea. J Korean Med Sci. 2022; 37(50):e349. PMID: 36573386.6. Jung K, Matsumoto S, Smith A, Hwang K, Lee JC, Coimbra R. Comparison of outcomes in severely injured patients between a South Korean trauma center and matched patients treated in the United States. Surgery. 2018; 164(3):482–488. PMID: 29884477.7. Kim YJ, Hong JS, Hong SI, Kim JS, Seo DW, Ahn R, et al. The prevalence and emergency department utilization of patients who underwent single and double inter-hospital transfers in the emergency department: a nationwide population-based study in Korea, 2016-2018. J Korean Med Sci. 2021; 36(25):e172. PMID: 34184436.8. Lee DJ, Ko SH, Kang J, Kim MC, Choi HZ. Survival benefit of direct transport to trauma centers among patients with unintentional injuries in Korea: a propensity score-matched analysis. Clin Exp Emerg Med. 2023; 10(1):37–43. PMID: 36174974.9. Locke T, Rekman J, Brennan M, Nasr A. The impact of transfer on pediatric trauma outcomes. J Pediatr Surg. 2016; 51(5):843–847. PMID: 26932250.10. Odetola FO, Mann NC, Hansen KW, Patrick S, Bratton SL. Source of admission and outcomes for critically injured children in the mountain states. Arch Pediatr Adolesc Med. 2010; 164(3):277–282. PMID: 20194263.11. Kim J, Shin SD, Im TH, Ko SB, Park JO, Ahn KO, et al. Kug Jong Lee. Development and validation of the excess mortality ratio-adjusted injury severity score using the International Classification of Diseases 10th Edition. Acad Emerg Med. 2009; 16(5):454–464. PMID: 19388920.12. Yohann A, Kratzke I, Williams B, Charles A. The effect of transfer status on trauma outcomes in low- and middle-income countries: a systematic review and meta-analysis. Injury. 2022; 53(3):885–894. PMID: 34689985.13. Hill AD, Fowler RA, Nathens AB. Impact of interhospital transfer on outcomes for trauma patients: a systematic review. J Trauma. 2011; 71(6):1885–1900. PMID: 22182900.14. Johnson DL, Krishnamurthy S. Send severely head-injured children to a pediatric trauma center. Pediatr Neurosurg. 1996; 25(6):309–314. PMID: 9348151.15. Larson JT, Dietrich AM, Abdessalam SF, Werman HA. Effective use of the air ambulance for pediatric trauma. J Trauma. 2004; 56(1):89–93. PMID: 14749572.16. Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc Bayl Univ Med Cent. 2010; 23(4):349–354. PMID: 20944754.17. Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer’s effect on mortality. J Trauma. 2010; 69(3):595–599. PMID: 20838131.18. Sampalis JS, Denis R, Fréchette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997; 43(2):288–295. PMID: 9291375.19. American College of Surgeons. Resources for the Optimal Care of the Injured Patient. Chicago, IL, USA: American College of Surgeons;2006.20. Bos N, Hendriks M, Booys M, Wets M. Spoed Moet Goed: Indicatoren en Normen voor zes Spoedzorgindicaties. Diemen, Netherlands: Zorginstituut Nederland;2015.21. Chaichotjinda K, Chantra M, Pandee U. Assessment of interhospital transport care for pediatric patients. Clin Exp Pediatr. 2020; 63(5):184–188. PMID: 31477679.22. Knight PH, Maheshwari N, Hussain J, Scholl M, Hughes M, Papadimos TJ, et al. Complications during intrahospital transport of critically ill patients: Focus on risk identification and prevention. Int J Crit Illn Inj Sci. 2015; 5(4):256–264. PMID: 26807395.23. Jouvet P, Lacroix J. Improving interhospital paediatric transport. Lancet. 2010; 376(9742):660–661. PMID: 20708257.24. Calhoun A, Keller M, Shi J, Brancato C, Donovan K, Kraus D, et al. Do pediatric teams affect outcomes of injured children requiring inter-hospital transport? Prehosp Emerg Care. 2017; 21(2):192–200. PMID: 27636186.25. Statistics Korea. Causes of death statistics in 2021. Updated 2022. Accessed January 7, 2023. http://www.kostat.go.kr .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Requests for Interhospital Transfer Received by An 1339 Emergency Medical Information Center
- Impact of Interhospital Transfer in Mortality of Critically Ill Patients
- Changes in Interhospital Transfer Patterns of Acute Ischemic Stroke Patients in the Regional Stroke Care System After Designation of a Cerebrovascular-specified Center
- Analysis of Factors Related to Delayed Answer in Interhospital Transfer Refer
- Multilevel analysis of factors affecting the interhospital transfer of high-acuity pediatric patients: a focus on severe pediatric emergency patients