Chonnam Med J.
2012 Dec;48(3):169-173. 10.4068/cmj.2012.48.3.169.
Changes in Interhospital Transfer Patterns of Acute Ischemic Stroke Patients in the Regional Stroke Care System After Designation of a Cerebrovascular-specified Center
- Affiliations
-
- 1Department of Emergency Medicine, Pusan National University Hospital, Busan, Korea.
- 2Stroke Center, Biomedical Research Institute, Department of Neurology, Pusan National University Hospital, Busan, Korea. aminoff@hanmail.net
- 3Department of Laboratory Medicine and Biomedical Informatics Unit, Pusan National University Hospital, Busan, Korea.
- 4Department of Emergency Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Korea.
- 5Busan Emergency Medical Information Center, Busan, Korea.
- KMID: 2048807
- DOI: http://doi.org/10.4068/cmj.2012.48.3.169
Abstract
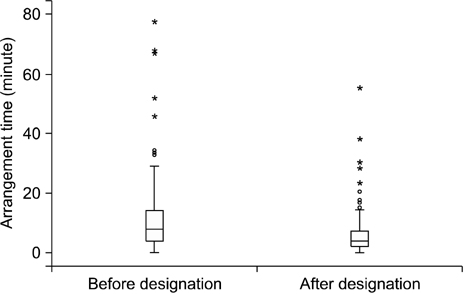
- The Ministry of Health and Welfare of Korea recently designated cerebrovascularspecified centers (CSCs) to improve the regional stroke care system for acute ischemic stroke (AIS) patients. This study was performed to evaluate the changes in the flow of AIS patients between hospitals and to describe the role of the Emergency Medical Information Center (EMIC) after the designation of the CSCs. Data for coordination of interhospital transfers by the EMIC were reviewed for 6 months before and after designation of the CSCs. The data included the success or failure rate, the time used for coordination of interhospital transfer, and the changes in the interhospital transfer pattern between transfer-requesting and transfer-accepting hospitals. The total number of requests for interhospital transfer increased from 198 to 244 after designation of the CSCs. The median time used for coordination decreased from 8.0 minutes to 4.0 minutes (p<0.001). The success rate of coordination increased from 88.9% to 96.7% (p<0.001). The proportion of requests by CSCs decreased from 3.5% to 0.4% (p=0.017). However, the proportion of acceptance by non-CSC hospitals increased from 15.9% to 25.8% (p=0.015). With the designation of CSCs, the EMIC could coordinate interhospital transfers more quickly. However, AIS patients are more dispersed to CSC and non-CSC hospitals, which might be because the CSCs still do not have sufficient resources to cover the increasing volume of AIS patients and non-CSC hospitals have changed their policies. Further studies based on patients' outcome are needed to determine the adequate type of interhospital transfer for AIS patients.
Keyword
Figure
Reference
-
1. Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, et al. Brain Attack Coalition. Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke. 2005. 36:1597–1616.2. Boyd DR, Cowley RA. Comprehensive regional trauma/emergency medical services (EMS) delivery systems: the United States experience. World J Surg. 1983. 7:149–157.
Article3. Harrington DT, Connolly M, Biffl WL, Majercik SD, Cioffi WG. Transfer times to definitive care facilities are too long: a consequence of an immature trauma system. Ann Surg. 2005. 241:961–966.
Article4. Glickman SW, Kit Delgado M, Hirshon JM, Hollander JE, Iwashyna TJ, Jacobs AK, et al. 2010 Academic Emergency Medicine Consensus Conference Beyond Regionalization: Intergrated Networks of Emergency Care. Defining and measuring successful emergency care networks: a research agenda. Acad Emerg Med. 2010. 17:1297–1305.
Article5. West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979. 114:455–460.
Article6. LaMonte MP, Bahouth MN, Magder LS, Alcorta RL, Bass RR, Browne BJ, et al. Emergency Medicine Network of the Maryland Brain Attack Center. A regional system of stroke care provides thrombolytic outcomes comparable with the NINDS stroke trial. Ann Emerg Med. 2009. 54:319–327.
Article7. Gropen TI, Gagliano PJ, Blake CA, Sacco RL, Kwiatkowski T, Richmond NJ, et al. NYSDOH Stroke Center Designation Project Workgroup. Quality improvement in acute stroke: the New York State Stroke Center Designation Project. Neurology. 2006. 67:88–93.
Article8. Stradling D, Yu W, Langdorf ML, Tsai F, Kostanian V, Hasso AN, et al. Stroke care delivery before vs after JCAHO stroke center certification. Neurology. 2007. 68:469–470.9. LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the "Get With The Guidelines" program. Arch Intern Med. 2008. 168:411–417.10. Stoeckle-Roberts S, Reeves MJ, Jacobs BS, Maddox K, Choate L, Wehner S, et al. Closing gaps between evidence-based stroke care guidelines and practices with a collaborative quality improvement project. Jt Comm J Qual Patient Saf. 2006. 32:517–527.11. Leifer D, Bravata DM, Connors JJ 3rd, Hinchey JA, Jauch EC, Johnston SC, et al. American Heart Association Special Writing Group of the Stroke Council. Atherosclerotic Peripheral Vascular Disease Working Group. Council on Cardiovascular Surgery and Anesthesia. Council on Cardiovascular Nursing. Metrics for measuring quality of care in comprehensive stroke centers: detailed follow-up to Brain Attack Coalition comprehensive stroke center recommendations: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011. 42:849–877.12. Guidelines for Field Triage of Injured Patients. Recommendations of the national expert panel on field triage. 2011. 06. Available at: http://www.cdc.gov/mmwr/pdf/rr/rr5801.pdf.13. Epley EE, Stewart RM, Love P, Jenkins D, Siegworth GM, Baskin TW, et al. A regional medical operations center improves disaster response and inter-hospital trauma transfers. Am J Surg. 2006. 192:853–859.14. Esposito TJ, Crandall M, Reed RL, Gamelli RL, Luchette FA. Socioeconomic factors, medicolegal issues, and trauma patient transfer trends: Is there a connection? J Trauma. 2006. 61:1380–1386.
Article15. Parks J, Gentilello LM, Shafi S. Financial triage in transfer of trauma patients: a myth or a reality? Am J Surg. 2009. 198:e35–e38.
Article16. Position paper on trauma care systems. Third National Injury Control Conference April 22-25, 1991, Denver, Colorado. J Trauma. 1992. 32:127–129.
Article17. US Department of Health and Human Services, Health Resources and Services Administration. Model trauma system planning and evaluation. 2006. cited 2011 July 1. Washington DC: US Department of Health and Human Services;Available from: http://www.kstrauma.org/download/ModelTraumaSystem-PlanningandEvaluation.pdf.
Article18. Schwamm LH, Pancioli A, Acker JE 3rd, Goldstein LB, Zorowitz RD, Shephard TJ, et al. American Stroke Association's Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Stroke. 2005. 36:690–703.
Article19. Ting HH, Rihal CS, Gersh BJ, Haro LH, Bjerke CM, Lennon RJ, et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007. 116:729–736.
Article20. Henry TD, Unger BT, Sharkey SW, Lips DL, Pedersen WR, Madison JD, et al. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. Am Heart J. 2005. 150:373–384.
Article21. Kim SK, Lee SY, Bae HJ, Lee YS, Kim SY, Kang MJ, et al. Pre-hospital notification reduced the door-to-needle time for iv t-PA in acute ischaemic stroke. Eur J Neurol. 2009. 16:1331–1335.
Article22. Lossius HM, Kristiansen T, Ringdal KG, Rehn M. Inter-hospital transfer: the crux of the trauma system, a curse for trauma registries. Scand J Trauma Resusc Emerg Med. 2010. 18:15.
Article23. Ringdal KG, Coats TJ, Lefering R, Di Bartolomeo S, Steen PA, Røise O, et al. Utstein TCD Expert Panel. The Utstein template for uniform reporting of data following major trauma: a joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008. 16:7.
Article