Pediatr Emerg Med J.
2024 Oct;11(4):154-161. 10.22470/pemj.2024.01053.
Multilevel analysis of factors affecting the interhospital transfer of high-acuity pediatric patients: a focus on severe pediatric emergency patients
- Affiliations
-
- 1National Emergency Medical Center, National Medical Center, Seoul
- 2Department of Public Health Graduate School, Inje University, Busan
- KMID: 2559548
- DOI: http://doi.org/10.22470/pemj.2024.01053
Abstract
- Purpose
The authors aimed to identify the factors affecting interhospital transfer (“transfer”) of severe pediatric patients who visited to an emergency department (ED).
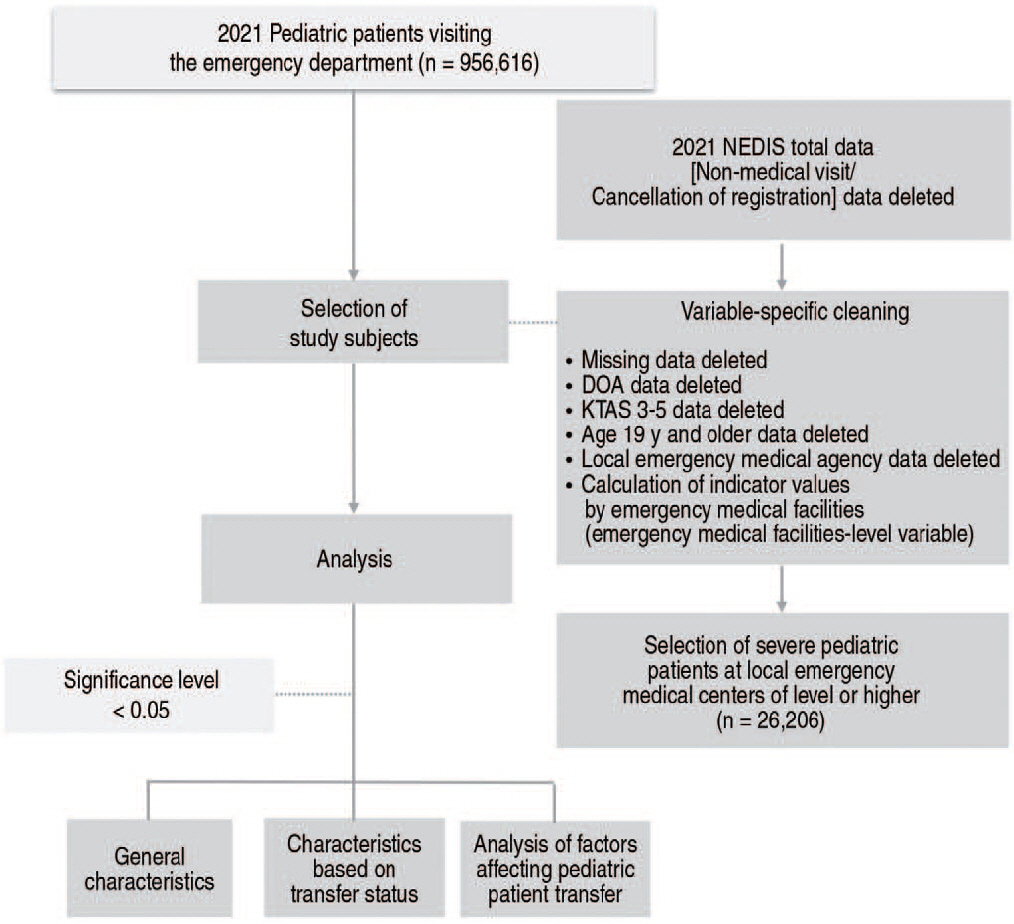
Methods
Using the Korean National ED Information System, we analyzed high-acuity patients aged 18 years or younger who visited EDs of local or regional emergency centers nationwide. The high acuity was defined as a Korean Triage and Acuity Scale 1-2. To investigate the factors associated with transfer, a multilevel modeling was selected, examining independent variables at both individual- and hospital-levels with transfer as a dependent variable.
Results
A model consisting of variables at individual- and hospital-levels showed the factors as follows: mode of arrival(self-transport: odds ratio, 0.48 [95% confidence interval, 0.38-0.61]; other ambulances: 0.41 [0.24-0.71]; compared with firehouse ambulance), visit at 18:00-07:59 (0.75 [0.64-0.88]), intentional injury (1.59 [1.03-2.47]; compared with non-injury), decreased level of consciousness (drowsy: 1.94 [1.33-2.84]; stupor: 4.08 [2.99-5.57]; coma: 1.81 [1.26-2.60]; compared with alert), severe illness diagnosis (1.49 [1.12-1.98]), the number of all beds in EDs (1.02 [1.01-1.04]), and acceptance for treatment (0.92 [0.87-0.98]; with increment of 1%).
Conclusion
This study confirms that both individual-level and hospital-level factors affect the transfer risk of severe pediatric patients in EDs. The study suggests the needs for direct transportation to specialized pediatric treatment facilities, and concentrated support for the pediatric emergency medical centers and pediatric trauma centers.
Figure
Reference
-
References
1. National Emergency Medical Center. 2021 Statistical yearbook of emergency medical service [Internet]. Seoul (Korea): National Emergency Medical Center; 2022 [cited 2024 Jul 30]. Available from: https://www.egen.or.kr/nemc/statistics_annual_report.do. Korean.2. National Emergency Medical Center. 2016 National Emergency Department Information System (NEDIS) statistical yearbook [Internet]. Seoul (Korea): National Emergency Medical Center; 2017 [cited 2024 Jul 30]. Available from: https://www.e-gen.or.kr/nemc/statistics_annual_report.do?brdclscd=02. Korean.3. Cho SJ, Hwang SY, Lee JH, Kim HH, Lee SH, Park MR, et al. Survey of Emergency-Related Physicians on Inter-hospital Transfers via 1339 in Busan. J Korean Soc Emerg Med. 2013; 24:131–41. Korean.4. Seo Y, Jung SY, Suh J. Factors associated with discharge of children from the emergency department after interfacility transfer. Pediatr Emerg Med J. 2017; 4:12–7. Korean.5. Richard KR, Glisson KL, Shah N, Aban I, Pruitt CM, Samuy N, et al. Predictors of potentially unnecessary transfers to pediatric emergency departments. Hosp Pediatr. 2020; 10:424–29.6. Li J, Monuteaux MC, Bachur RG. Interfacility transfers of noncritically ill children to academic pediatric emergency departments. Pediatrics. 2012; 130:83–92.7. Noh H. Prehospital transport of critically ill children via 119 emergency medical service providers: problems and improvement plan. Pediatr Emerg Med J. 2017; 4:34–7. Korean.8. Ministry of Health and Welfare. Pediatric emergency medical center selection indicator [Internet]. Ministry of Health and Welfare; 2023 [cited 2024 Sep 22]. Available from: https://portal.nemc.or.kr:444/init.do?systemauth=06&sytmidno=29&menuflag=&linkurl=.Korean.9. Oh WC, Noh H. Consideration in Korean Triage and Acuity Scale for febrile pediatric patients: symptom duration. J Korean Soc Emerg Med. 2019; 30:69–76. Korean.10. Kwak YH, Kim DK, Jang HY. Utilization of emergency department by children in Korea. J Korean Med Sci. 2012; 27:1222–8. Korean.11. Kim Y. Impact of regional emergency medical access on patients’prognosis and emergency medical expenditure [master’s thesis]. Seoul National University;2020. Korean.12. Ahn KO, Hong JY, Kim Y, Jung KY. Appropriate interhospital transfer of emergent patients. J Korean Soc Emerg Med. 2006; 17:138–45. Korean.13. National Emergency Medical Center. 2021-2022 Status report of emergency room visits by individuals attempting self-harm or suicide. National Emergency Medical Center: 2023. p. 2. Korean.14. Park JY, Kim YH, Lee JH, Lee DW, Ahn SJ, Keum KT, et al. Pediatric out-of-hospital cardiac arrest: incidence and outcomes in an urban city. J Korean Soc Emerg Med. 2022; 33:141–48. Korean.15. Roh H, Kang Y. The management of patient attempting suicide in the emergency room. J Med Life Sci. 2019; 16:60–3. Korean.16. Song X, Case AL, Carroll R, Abzug JM. Pediatric emergency room transfers: are they warranted? J Pediatr Orthop. 2019; 39:430–35.17. Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer’s effect on mortality. J Trauma. 2010; 69:595–601.18. Jung D, Jung JH, Kim JH, Jue JH, Park JW, Kim DK, et al. The association between interhospital transfers and the prognosis of pediatric injury in the emergency department. J Korean Med Sci. 2024; 39:e2.19. Johnson DL, Krishnamurthy S. Send severely head-injured children to a pediatric trauma center. Pediatr Neurosurg. 1996; 25:309–14.20. Moon BH, Lee SM, Oh M, Ryu HH, Heo T. Analysis of emergency department utilization rate by region, emergency medical center, and hospital type. J Korean Soc Emerg Med. 2016; 27:442–49. Korean.21. Lee MO, Wall J, Saynina O, Camargo CA Jr, Wang NE. Characteristics of pediatric patient transfers from general emergency departments in California from 2005 to 2018. Pediatr Emerg Care. 2023; 39:20–7.22. Dabija M, Aine M, Forsberg A. Caring for critically ill patients during interhospital transfers: a qualitative study. Nurs Crit Care. 2021; 26:333–40.23. Harish MM, Siddiqui SS, Prabu NR, Chaudhari HK, Divatia JV, Kulkarni AP. Benefits of and untoward events during intrahospital transport of pediatric intensive care unit patients. Indian J Crit Care Med. 2017; 21:46–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Factors Related to Delayed Answer in Interhospital Transfer Refer
- The Association Between InterHospital Transfers and the Prognosis of Pediatric Injury in the Emergency Department
- Assessment of interhospital transport care for pediatric patients
- Requests for Interhospital Transfer Received by An 1339 Emergency Medical Information Center
- Impact of Interhospital Transfer in Mortality of Critically Ill Patients