J Dent Rehabil Appl Sci.
2023 Dec;39(4):267-275. 10.14368/jdras.2023.39.4.267.
Digital immediate implantation and aesthetic immediate loading on maxillary incisor displaced due to root fracture: a case report
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Chonnam National University, Gwangju, Republic of Korea
- KMID: 2550436
- DOI: http://doi.org/10.14368/jdras.2023.39.4.267
Abstract
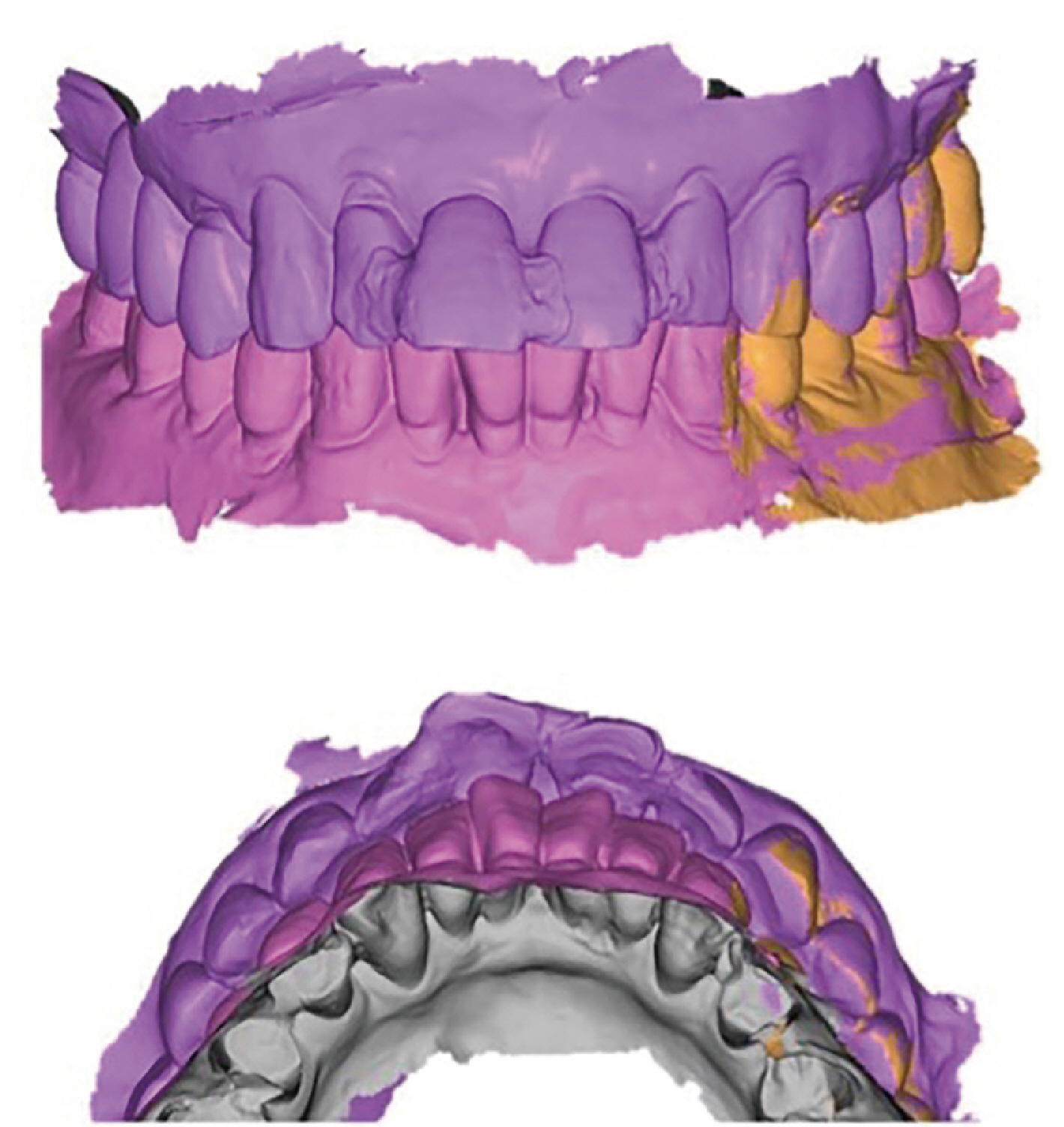
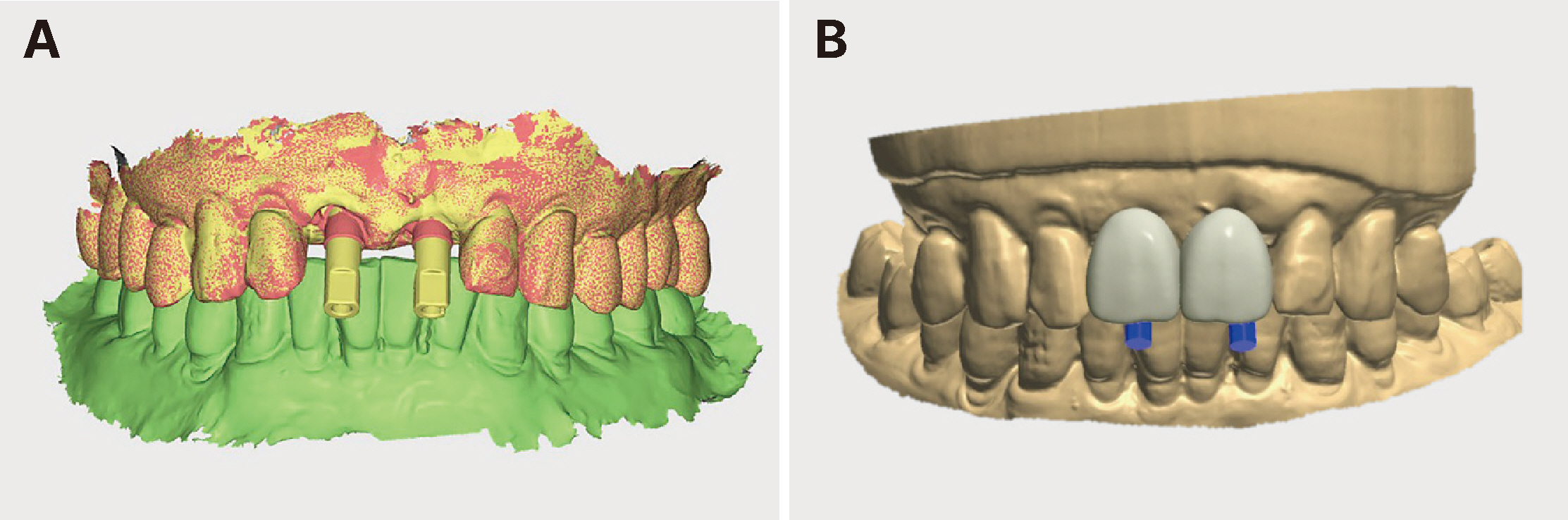
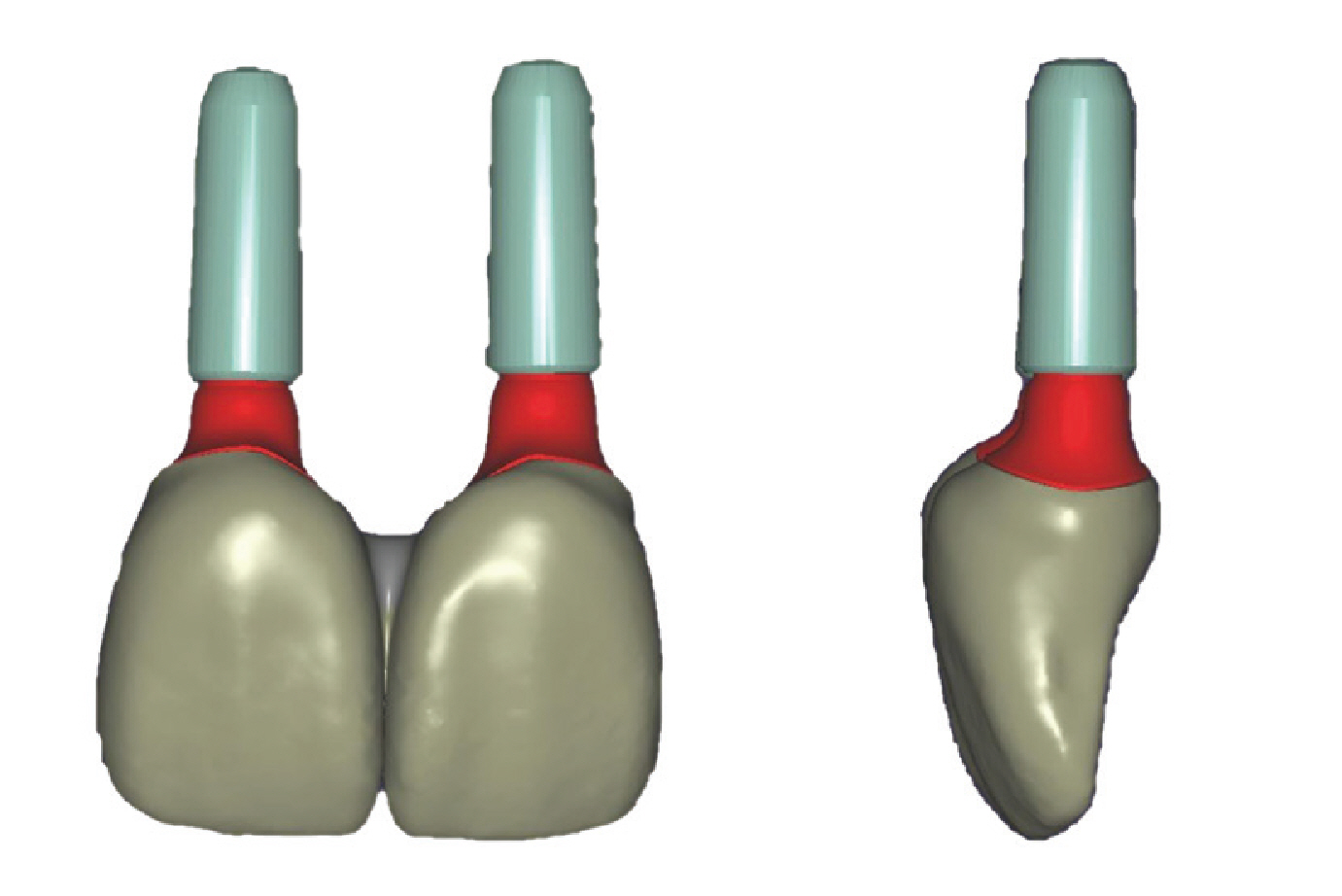
- To obtain better esthetic results when immediately placing a dental implant, the soft tissue surrounding the implant must be conditioned during healing of the extraction socket. To this end, the emergence profile can be customized through immediate restoration of the provisional prosthesis, and good clinical results can be obtained at the time of definitive restoration in the future, resulting in high patient satisfaction. In this case, horizontal root fracture occurred after trauma to both maxillary central incisors. Immediate implant placement and loading was planned considering aesthetics and alveolar bone condition. By taking an impression using a digital intraoral scanner, a digital diagnostic wax-up was performed to make a more aesthetic prosthesis without applying external force to the traumatized teeth. Based on this, the ideal placement location was determined and immediate implant placement was performed using a 3D printed surgical guide. The provisional prosthesis was restored 5 days after placement, and the definitive zirconia crown was restored through soft tissue conditioning and customization using the shape of the provisional prosthesis for 3 months.
Keyword
Figure
Reference
-
References
1. Fuentealba R, Jofré J. 2015; Esthetic failure in implant dentistry. Dent Clin North Am. 59:227–46. DOI: 10.1016/j.cden.2014.08.006. PMID: 25434568.2. Scotti R, Pellegrino G, Marchetti C, Corinaldesi G, Ciocca L. 2010; Diagnostic value of NobelGuide to minimize the need for reconstructive surgery of jaws before implant placement: a review. Quintessence Int. 41:809–14. PMID: 20927416.3. Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, Orsini M. 1997; A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. J Periodontol. 68:563–70. DOI: 10.1902/jop.1997.68.6.563. PMID: 9203100.4. Koutrach M, Nimmo A. 2010; Preservation of existing soft-tissue contours in the transition from a tooth to an implant restoration in the esthetic zone using a flapless approach: a clinical report. J Prosthodont. 19:391–6. DOI: 10.1111/j.1532-849X.2010.00581.x. PMID: 20345743.5. Gomez-Meda R, Esquivel J, Blatz MB. 2021; The esthetic biological contour concept for implant restoration emergence profile design. J Esthet Restor Dent. 33:173–84. DOI: 10.1111/jerd.12714. PMID: 33470498.6. Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hämmerle CH, Tahmaseb A. 2009; Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 24 Suppl:92–109.7. Spray JR, Black CG, Morris HF, Ochi S. 2000; The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 5:119–28. DOI: 10.1902/annals.2000.5.1.119. PMID: 11885170.8. Park YH, Ahn SG, Kim KA, Seo JM. 2021; Esthetic considerations for anterior implant-supported prostheses: focus on surgical and prosthetic treatment. J Dent Rehabil Appl Sci. 37:186–98. DOI: 10.14368/jdras.2021.37.4.186.9. Bhola M, Neely AL, Kolhatkar S. 2008; Immediate implant placement: clinical decisions, advantages, and disadvantages. J Prosthodont. 17:576–81. DOI: 10.1111/j.1532-849X.2008.00359.x. PMID: 18761580.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral maxillary central incisor root resorption after orthodontic treatment for Angle Class II, division 1 malocclusion with significant maxillary midline deviation: A possible correlation with root proximity to the incisive canal
- Use of mineral trioxide aggregate in the treatment of horizontal root fracture with a 4-year follow-up: case report
- Orthodontic treatment of an impacted maxillary central incisor with dilacerations
- Interdisciplinary rehabilitation of a root-fractured maxillary central incisor: A 12-year follow-up case report
- Usage of digital technique to facilitate communication between dentist, dental lab technician, and patients in diagnosis and restoration for maxillary anterior implant: a case report