J Dent Rehabil Appl Sci.
2023 Dec;39(4):260-266. 10.14368/jdras.2023.39.4.260.
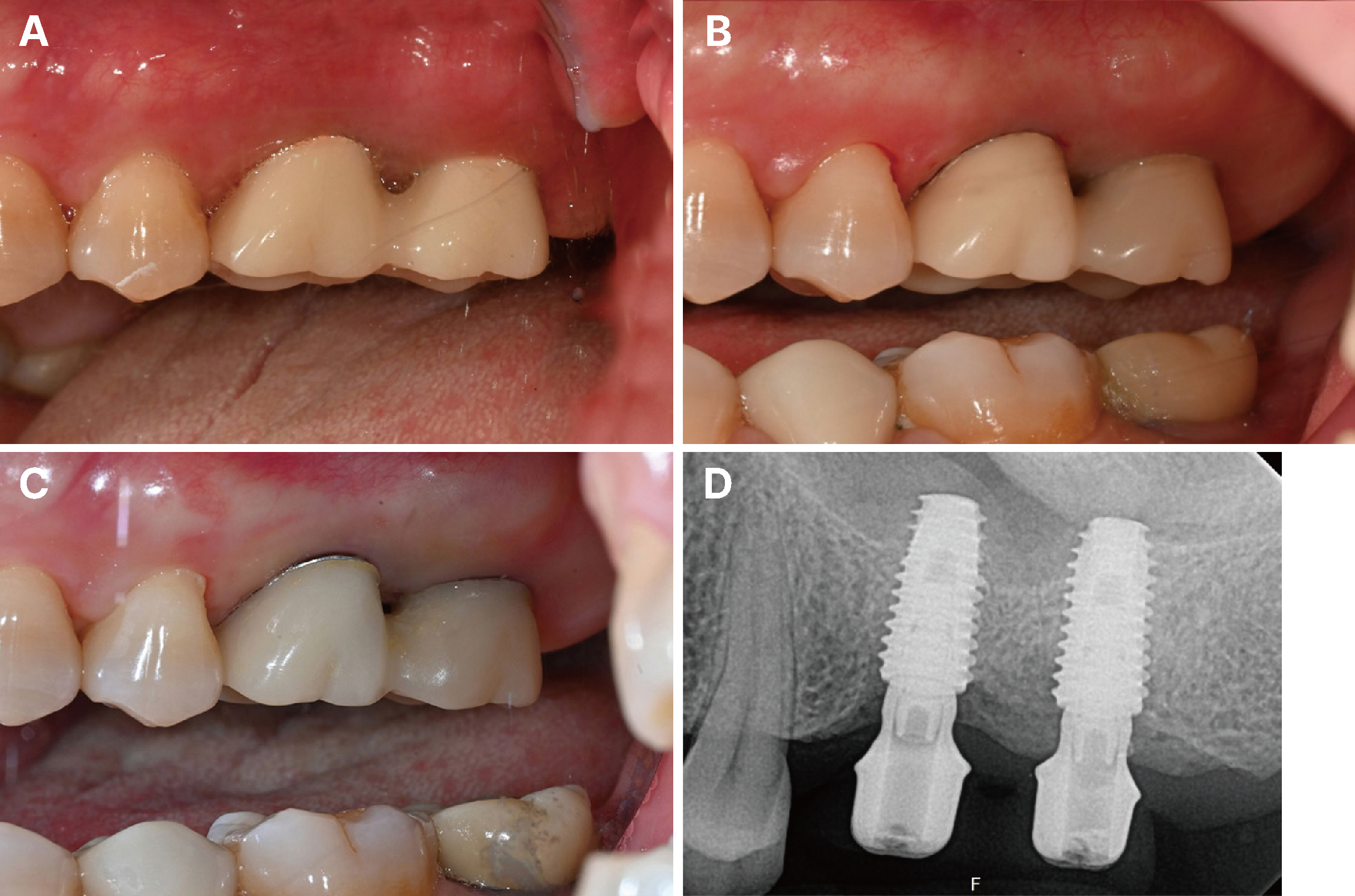
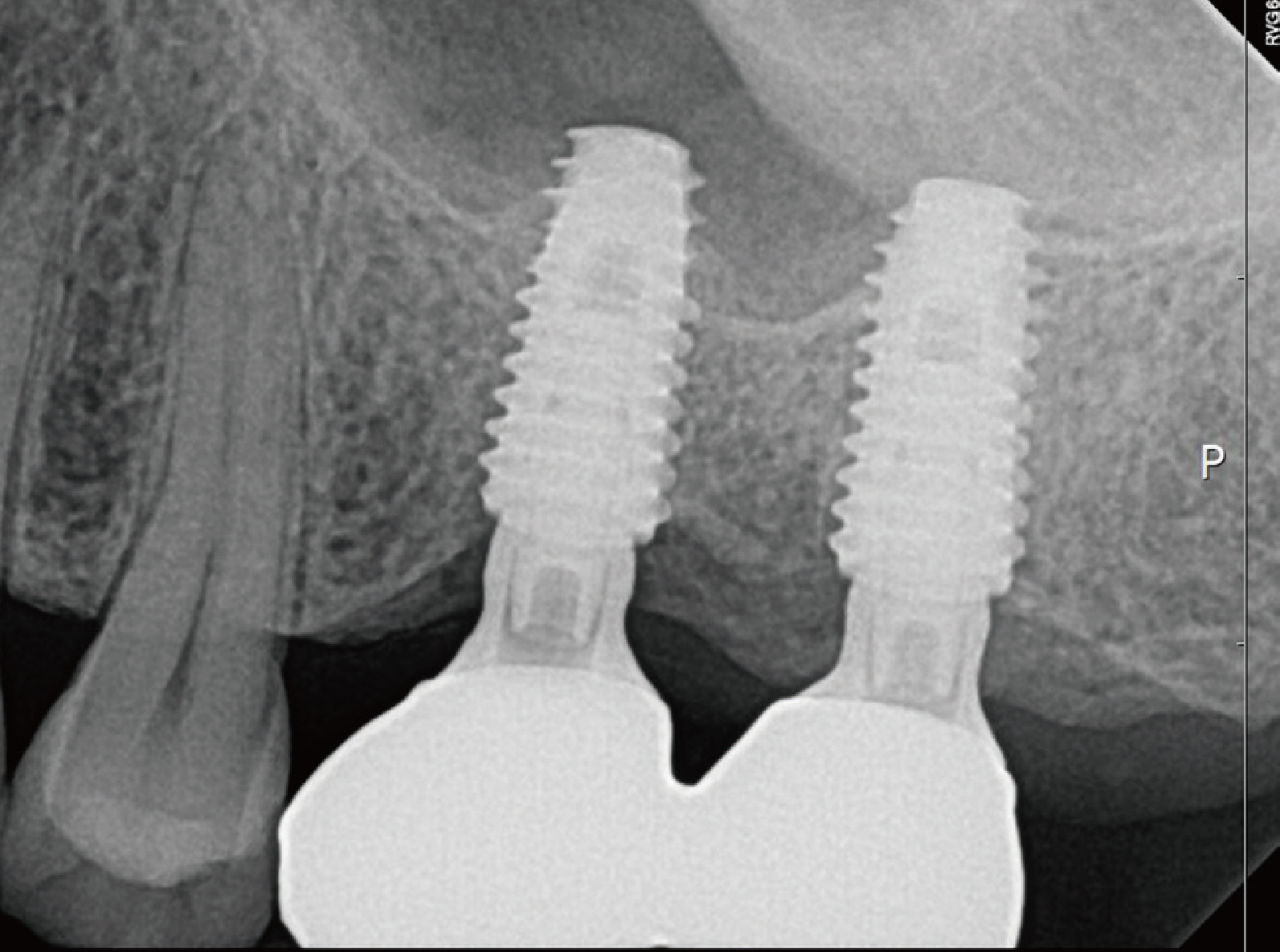
Improvement of peri-implant complications through customized prosthesis restoration allowing soft tissue space: a case report
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Chonnam National University, Gwangju, Republic of Korea
- KMID: 2550435
- DOI: http://doi.org/10.14368/jdras.2023.39.4.260
Abstract
- The concept of ‘Implant Supracrestal Complex (ISC)’ was introduced as a way to determine the impact of implant prosthetic design form on both short-term clinical outcomes and the long-term prognosis of bone and soft tissues around the implant. Implant-prosthesis-abutment complex design forms, such as implant-abutment design, junction, and location, can have important implications for the stable and healthy long-term maintenance of the tissues around the implant. In this case, a customized concave abutment and a prosthesis with an emergence angle of about 30 degrees were restored to a patient suffering from chronic soft tissue inflammation and pain after restoration of an implant prosthesis. It was confirmed that the new prosthesis improved complications by allowing sufficient bone and soft tissue space, achieved appropriate soft tissue sealing, and maintained the longterm stability of the implant.
Figure
Reference
-
References
1. Barootchi S, Wang HL. 2021; Peri-implant diseases: Current understanding and management. Int J Oral Implantol (Berl). 14:263–82. PMID: 34415128.2. Schwarz F, Alcoforado G, Guerrero A, Jönsson D, Klinge B, Lang N, Mattheos N, Mertens B, Pitta J, Ramanauskaite A, Sayardoust S, Sanz-Martin I, Stavropoulos A, Heitz-Mayfield L. 2021; Peri-implantitis: Summary and consensus statements of group 3. The 6th EAO Consensus Conference 2021. Clin Oral Implants Res. 32 Suppl 21:245–53. DOI: 10.1111/clr.13827. PMID: 34642987.3. Albrektsson T, Isidor F. Lang NP, Karring T, editors. 1994. Consensus Report of Session IV. Proceedings of the 1st European Workshop on Periodontology. Quintessence;Berlin: p. 365–369.4. Costa FO, Takenaka-Martinez S, Cota LO, Ferreira SD, Silva GL, Costa JE. 2012; Peri-implant disease in subjects with and without preventive maintenance: a 5-year follow-up. J Clin Periodontol. 39:173–81. DOI: 10.1111/j.1600-051X.2011.01819.x. PMID: 22111654.5. Mattheos N, Janda M, Acharya A, Pekarski S, Larsson C. 2021; Impact of design elements of the implant supracrestal complex (ISC) on the risk of peri-implant mucositis and peri-implantitis: A critical review. Clin Oral Implants Res. 32 Suppl 21:181–202. DOI: 10.1111/clr.13823. PMID: 34642979.6. Koutouzis T, Adeinat B, Ali A. 2019; The influence of abutment macro-design on clinical and radiographic peri-implant tissue changes for guided, placed, and restored implants: A 1-year randomized controlled trial. Clin Oral Implants Res. 30:882–91. DOI: 10.1111/clr.13493. PMID: 31180160.7. Pérez-Sayans M, Castelo-Baz P, Penarrocha-Oltra D, Seijas-Naya F, Conde-Amboage M, Somoza-Martín JM. 2022; Impact of abutment geometry on early implant marginal bone loss. A double-blind, randomized, 6-month clinical trial. Clin Oral Implants Res. 33:1038–48. DOI: 10.1111/clr.13985. PMID: 35869615. PMCID: PMC9796139.8. Yi Y, Koo KT, Schwarz F, Ben Amara H, Heo SJ. 2020; Association of prosthetic features and peri-implantitis: A cross-sectional study. J Clin Periodontol. 47:392–403. DOI: 10.1111/jcpe.13251. PMID: 31912511.9. Majzoub J, Chen Z, Saleh I, Askar H, Wang HL. 2021; Influence of restorative design on the progression of peri-implant bone loss: A retrospective study. J Periodontol. 92:536–46. DOI: 10.1002/JPER.20-0327. PMID: 32902855.10. Katafuchi M, Weinstein BF, Leroux BG, Chen YW, Daubert DM. 2018; Restoration contour is a risk indicator for peri-implantitis: A cross-sectional radiographic analysis. J Clin Periodontol. 45:225–32. DOI: 10.1111/jcpe.12829. PMID: 28985447.11. Berglundh T, Lindhe J, Marinello C, Ericsson I, Liljenberg B. 1992; Soft tissue reaction to de novo plaque formation on implants and teeth. An experimental study in the dog. Clin Oral Implants Res. 3:1–8. DOI: 10.1034/j.1600-0501.1992.030101.x. PMID: 1420721.12. Pérez-Chaparro PJ, Duarte PM, Shibli JA, Montenegro S, Lacerda Heluy S, Figueiredo LC, Faveri M, Feres M. 2016; The Current Weight of Evidence of the Microbiologic Profile Associated With Peri-Implantitis: A Systematic Review. J Periodontol. 87:1295–304. DOI: 10.1902/jop.2016.160184. PMID: 27420109.13. Salvi GE, Aglietta M, Eick S, Sculean A, Lang NP, Ramseier CA. 2012; Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans. Clin Oral Implants Res. 23:182–90. DOI: 10.1111/j.1600-0501.2011.02220.x. PMID: 21806683.14. Renvert S, Polyzois I. 2015; Risk indicators for peri-implant mucositis: a systematic literature review. J Clin Periodontol. 42 Suppl 16:S172–86. DOI: 10.1111/jcpe.12346.15. Lin GH, Chan HL, Wang HL. 2013; The significance of keratinized mucosa on implant health: a systematic review. J Periodontol. 84:1755–67. DOI: 10.1902/jop.2013.120688. PMID: 23451989.16. Gupta S, Sabharwal R, Nazeer J, Taneja L, Choudhury BK, Sahu S. 2019; Platform switching technique and crestal bone loss around the dental implants: A systematic review. Ann Afr Med. 18:1–6. DOI: 10.4103/aam.aam_15_18. PMID: 30729925. PMCID: PMC6380118.17. Rodríguez X, Navajas A, Vela X, Fortuño A, Jimenez J, Nevins M. 2016; Arrangement of Peri-implant Connective Tissue Fibers Around Platform-Switching Implants with Conical Abutments and Its Relationship to the Underlying Bone: A Human Histologic Study. Int J Periodontics Restorative Dent. 36:533–40. DOI: 10.11607/prd.2580. PMID: 27333011.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aesthetic prosthetic restoration through immediate implant placement and provisional restoration in the maxillary anterior region using a digital guide
- Clinical case of implant restoration using customized healing abutment
- Clinical cases of implant-supported fixed dental prosthesis using modified lingual screw system (T-screw system)
- Maxillary anterior fixed implant prosthesis using customized nonprecious metal casting abutment: a case report
- Maxillary anterior single implant prosthesis