Endocrinol Metab.
2023 Dec;38(6):770-781. 10.3803/EnM.2023.1726.
Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2549270
- DOI: http://doi.org/10.3803/EnM.2023.1726
Abstract
- Background
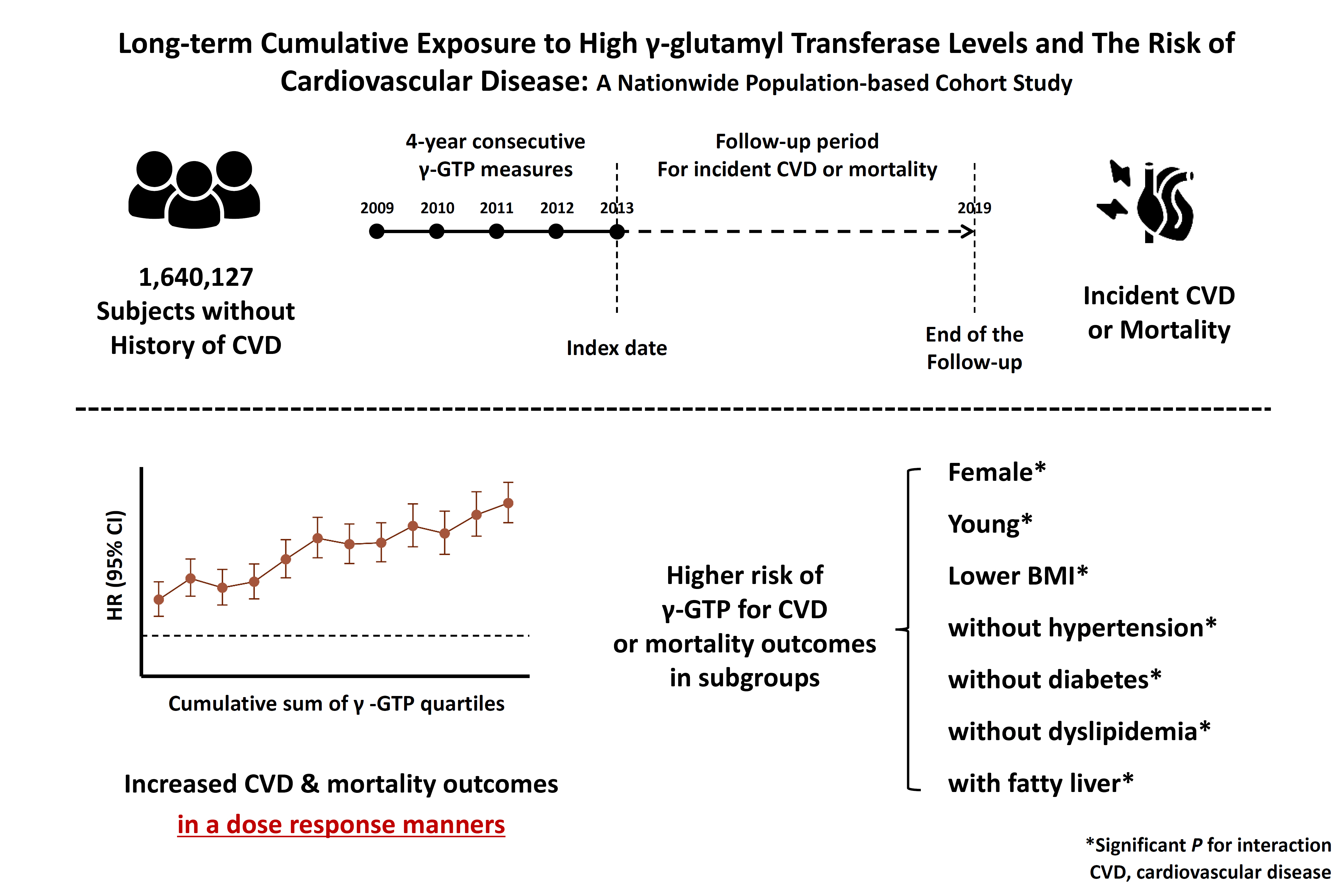
Elevated γ-glutamyl transferase (γ-GTP) levels are associated with metabolic syndrome. We investigated the association of cumulative exposure to high γ-GTP with the risk of cardiovascular disease (CVD) in a large-scale population.
Methods
Using nationally representative data from the Korean National Health Insurance system, 1,640,127 people with 4 years of consecutive γ-GTP measurements from 2009 to 2012 were included and followed up until the end of 2019. For each year of the study period, participants were grouped by the number of exposures to the highest γ-GTP quartile (0–4), and the sum of quartiles (0–12) was defined as cumulative γ-GTP exposure. The hazard ratio for CVD was evaluated using the Cox proportional hazards model.
Results
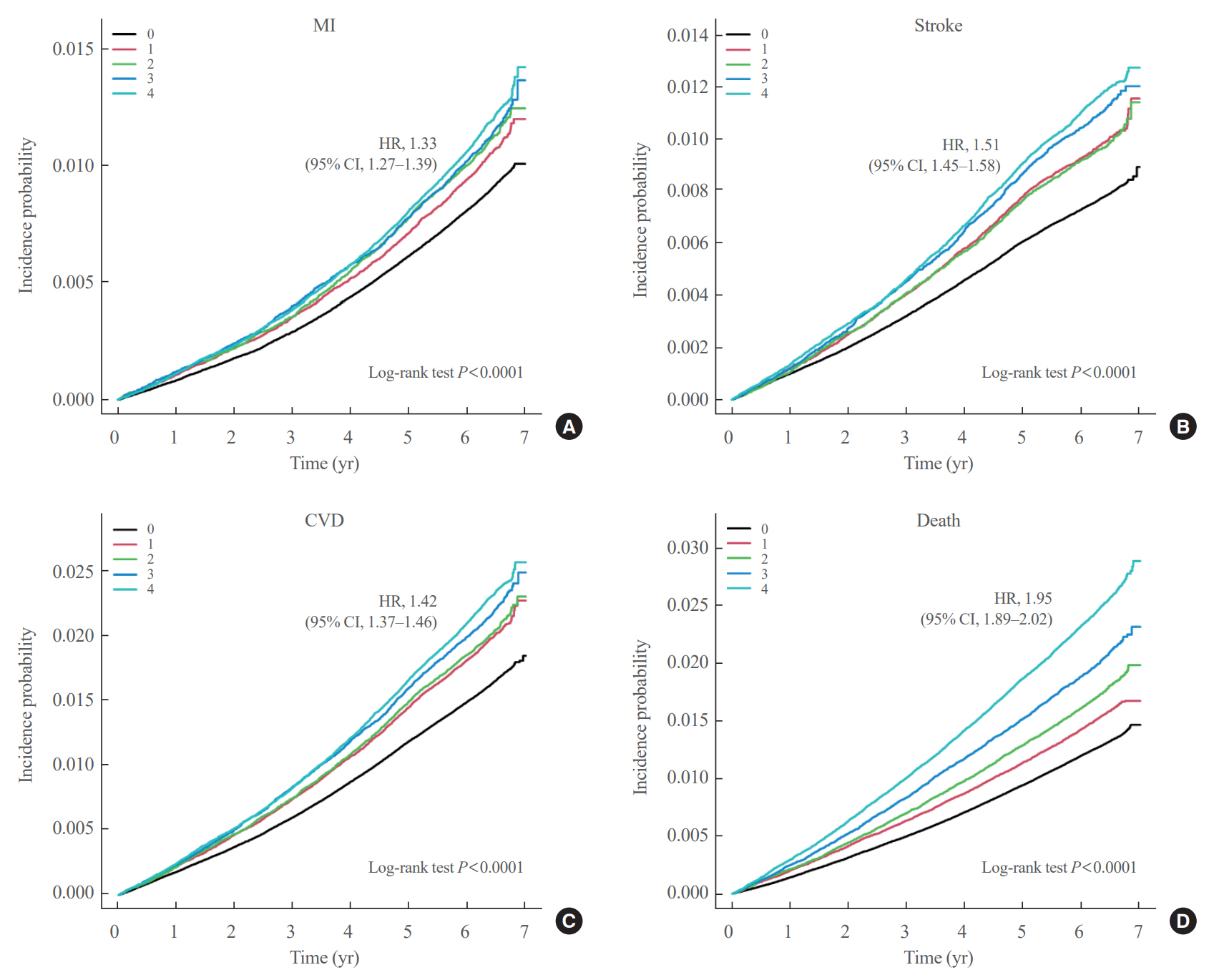
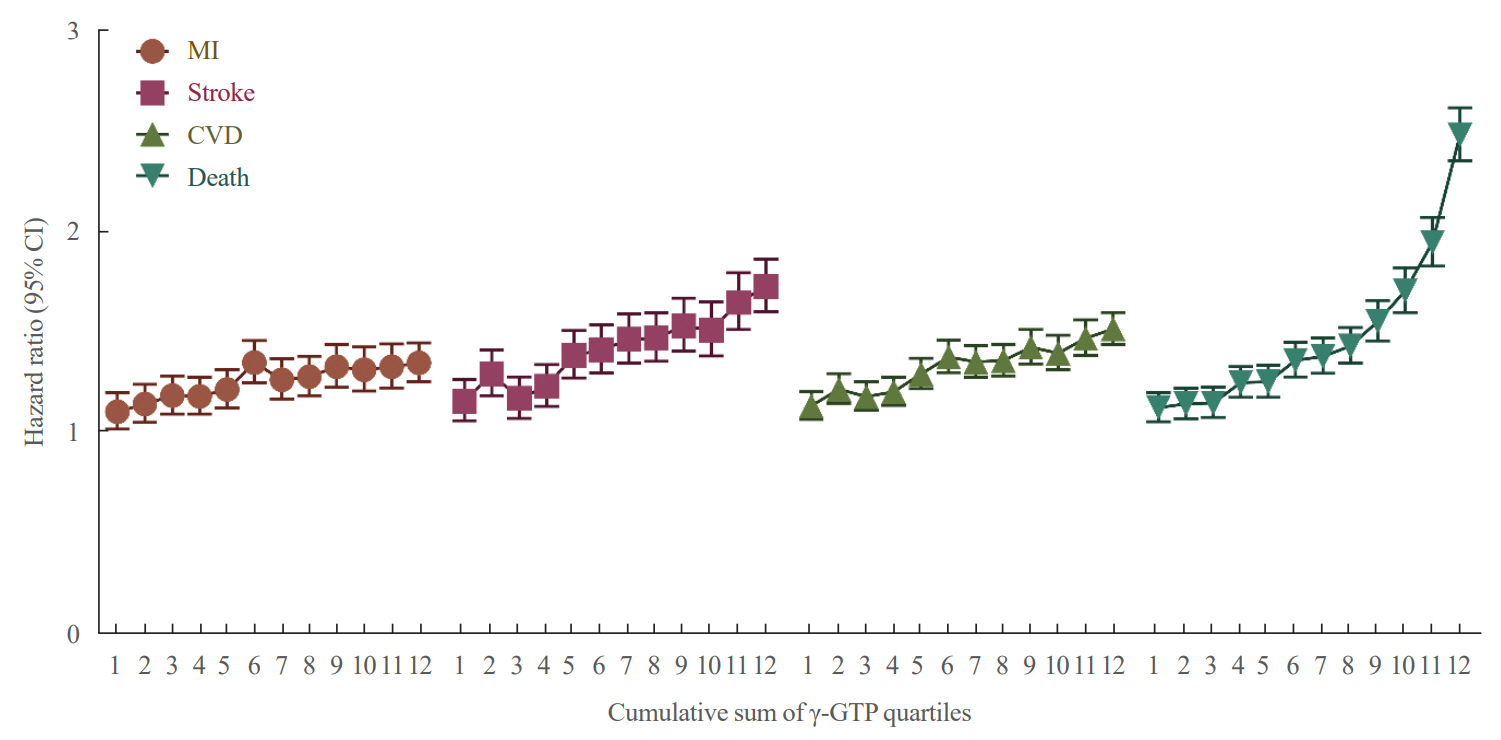
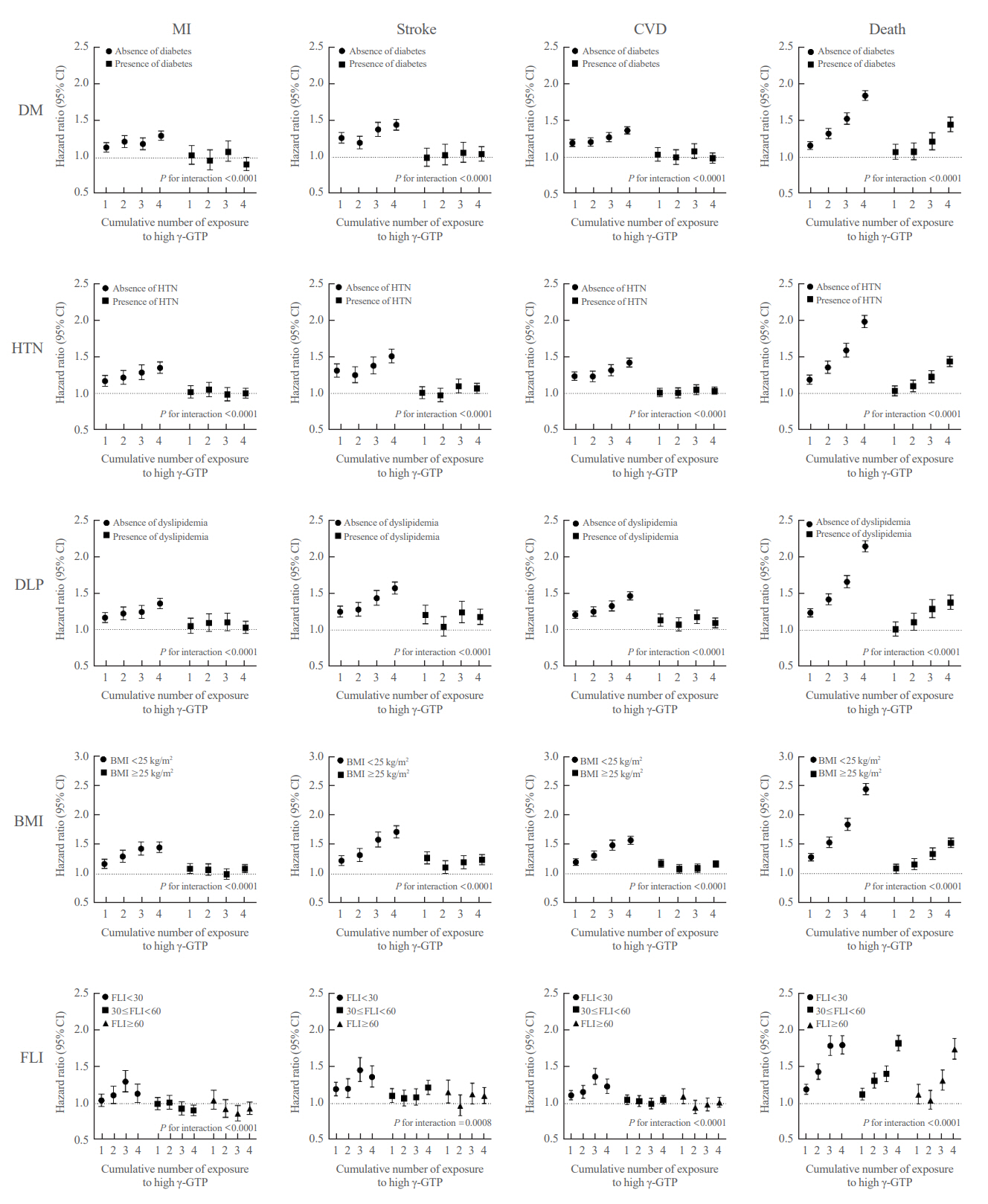
During the 6.4 years of follow-up, there were 15,980 cases (0.97%) of myocardial infarction (MI), 14,563 (0.89%) of stroke, 29,717 (1.81%) of CVD, and 25,916 (1.58%) of death. Persistent exposure to high γ-GTP levels was associated with higher risks of MI, stroke, CVD, and death than those without such exposure. The risks of MI, stroke, CVD, and mortality increased in a dose-dependent manner according to total cumulative γ-GTP (all P for trend <0.0001). Subjects younger than 65 years, with a body mass index <25 kg/m2, and without hypertension or fatty liver showed a stronger relationship between cumulative γ-GTP and the incidence of MI, CVD, and death.
Conclusion
Cumulative γ-GTP elevation is associated with CVD. γ-GTP could be more widely used as an early marker of CVD risk, especially in individuals without traditional CVD risk factors.
Figure
Reference
-
1. Han E, Song SO, Kim HS, Son KJ, Jee SH, Cha BS, et al. Improvement in age at mortality and changes in causes of death in the population with diabetes: an analysis of data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018. Endocrinol Metab (Seoul). 2022; 37:466–74.
Article2. World Health Organization. Cardiovascular diseases (CVD) [Internet]. Geneva: WHO;2021. [cited 2023 Sep 12]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).3. Lee HH, Cho SM, Lee H, Baek J, Bae JH, Chung WJ, et al. Korea heart disease fact sheet 2020: analysis of nationwide data. Korean Circ J. 2021; 51:495–503.
Article4. Francula-Zaninovic S, Nola IA. Management of measurable variable cardiovascular disease’ risk factors. Curr Cardiol Rev. 2018; 14:153–63.
Article5. Cohn JN, Hoke L, Whitwam W, Sommers PA, Taylor AL, Duprez D, et al. Screening for early detection of cardiovascular disease in asymptomatic individuals. Am Heart J. 2003; 146:679–85.
Article6. Baek HS, Park JY, Yu J, Lee J, Yang Y, Ha J, et al. Characteristics of glycemic control and long-term complications in patients with young-onset type 2 diabetes. Endocrinol Metab (Seoul). 2022; 37:641–51.
Article7. Neuman MG, Malnick S, Chertin L. Gamma glutamyl transferase: an underestimated marker for cardiovascular disease and the metabolic syndrome. J Pharm Pharm Sci. 2020; 23:65–74.
Article8. Kazemi-Shirazi L, Endler G, Winkler S, Schickbauer T, Wagner O, Marsik C. Gamma glutamyltransferase and long-term survival: is it just the liver? Clin Chem. 2007; 53:940–6.
Article9. Koenig G, Seneff S. Gamma-glutamyltransferase: a predictive biomarker of cellular antioxidant inadequacy and disease risk. Dis Markers. 2015; 2015:818570.
Article10. Park JY, Han K, Kim HS, Cho JH, Yoon KH, Kim MK, et al. Cumulative exposure to high γ-glutamyl transferase level and risk of diabetes: a nationwide population-based study. Endocrinol Metab (Seoul). 2022; 37:272–80.
Article11. Bharani V, Ramesh V, Rao RN, Tewari S. Evaluation of gamma glutamyl transferase as a marker of cardiovascular risk, in 200 angiographically proven coronary artery disease patients. Indian Heart J. 2017; 69:325–7.
Article12. Sarikaya S, Aydin G, Yucel H, Kaya H, Yildirimli K, Basaran A, et al. Usefulness of admission gamma-glutamyltransferase level for predicting new-onset heart failure in patients with acute coronary syndrome with left ventricular systolic dysfunction. Turk Kardiyol Dern Ars. 2014; 42:236–44.
Article13. Sheikh M, Tajdini M, Shafiee A, Sotoudeh Anvari M, Jalali A, Poorhosseini H, et al. Association of serum gamma-glutamyltransferase and premature coronary artery disease. Neth Heart J. 2017; 25:439–45.
Article14. Yang P, Wu P, Liu X, Feng J, Zheng S, Wang Y, et al. Association between γ-glutamyltransferase level and cardiovascular or all-cause mortality in patients with coronary artery disease: a systematic review and meta-analysis. Angiology. 2019; 70:844–52.
Article15. Long Y, Zeng F, Shi J, Tian H, Chen T. Gamma-glutamyltransferase predicts increased risk of mortality: a systematic review and meta-analysis of prospective observational studies. Free Radic Res. 2014; 48:716–28.
Article16. Kim MK, Han K, Lee SH. Current trends of big data research using the Korean National Health Information Database. Diabetes Metab J. 2022; 46:552–63.
Article17. Cho SW, Kim JH, Choi HS, Ahn HY, Kim MK, Rhee EJ. Big data research in the field of endocrine diseases using the Korean National Health Information Database. Endocrinol Metab (Seoul). 2023; 38:10–24.
Article18. Nam GE, Kim YH, Han K, Jung JH, Rhee EJ, Lee WY, et al. Obesity fact sheet in Korea, 2020: prevalence of obesity by obesity class from 2009 to 2018. J Obes Metab Syndr. 2021; 30:141–8.
Article19. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145:247–54.
Article20. Han B, Lee GB, Yim SY, Cho KH, Shin KE, Kim JH, et al. Non-alcoholic fatty liver disease defined by fatty liver index and incidence of heart failure in the Korean population: a nationwide cohort study. Diagnostics (Basel). 2022; 12:663.
Article21. Ceriotti F, Henny J, Queralto J, Ziyu S, Ozarda Y, Chen B, et al. Common reference intervals for aspartate aminotransferase (AST), alanine aminotransferase (ALT) and γ-glutamyl transferase (GGT) in serum: results from an IFCC multicenter study. Clin Chem Lab Med. 2010; 48:1593–601.
Article22. Li S, Wang A, Tian X, Zuo Y, Meng X, Zhang Y. Elevated gamma-glutamyl transferase levels are associated with stroke recurrence after acute ischemic stroke or transient ischemic attack. CNS Neurosci Ther. 2022; 28:1637–47.
Article23. Fedak KM, Bernal A, Capshaw ZA, Gross S. Applying the Bradford Hill criteria in the 21st century: how data integration has changed causal inference in molecular epidemiology. Emerg Themes Epidemiol. 2015; 12:14.
Article24. Ndrepepa G, Colleran R, Kastrati A. Gamma-glutamyl transferase and the risk of atherosclerosis and coronary heart disease. Clin Chim Acta. 2018; 476:130–8.
Article25. Kunutsor SK, Bakker SJ, Kootstra-Ros JE, Gansevoort RT, Dullaart RP. Circulating gamma glutamyltransferase and prediction of cardiovascular disease. Atherosclerosis. 2015; 238:356–64.
Article26. Dominici S, Paolicchi A, Corti A, Maellaro E, Pompella A. Prooxidant reactions promoted by soluble and cell-bound gamma-glutamyltransferase activity. Methods Enzymol. 2005; 401:484–501.27. Silveira Rossi JL, Barbalho SM, Reverete de Araujo R, Bechara MD, Sloan KP, Sloan LA. Metabolic syndrome and cardiovascular diseases: going beyond traditional risk factors. Diabetes Metab Res Rev. 2022; 38:e3502.
Article28. Yang W, Kim CK, Kim DY, Jeong HG, Lee SH. Gamma-glutamyl transferase predicts future stroke: a Korean nationwide study. Ann Neurol. 2018; 83:375–86.
Article29. Bijnens EM, Derom C, Thiery E, Martens DS, Loos RJ, Weyers S, et al. Serum gamma-glutamyl transferase, a marker of alcohol intake, is associated with telomere length and cardiometabolic risk in young adulthood. Sci Rep. 2021; 11:12407.
Article30. Hong NS, Kim JG, Lee YM, Kim HW, Kam S, Kim KY, et al. Different associations between obesity and impaired fasting glucose depending on serum gamma-glutamyltransferase levels within normal range: a cross-sectional study. BMC Endocr Disord. 2014; 14:57.
Article31. Whitfield JB. Gamma glutamyl transferase. Crit Rev Clin Lab Sci. 2001; 38:263–355.
Article32. Yi SW, Lee SH, Hwang HJ, Yi JJ. Gamma-glutamyltransferase and cardiovascular mortality in Korean adults: a cohort study. Atherosclerosis. 2017; 265:102–9.
Article33. Cho EJ, Jeong SM, Chung GE, Yoo JJ, Cho Y, Lee KN, et al. Gamma-glutamyl transferase and risk of all-cause and disease-specific mortality: a nationwide cohort study. Sci Rep. 2023; 13:1751.
Article34. Zhang XW, Li M, Hou WS, Li K, Zhou JR, Tang ZY. Association between gamma-glutamyltransferase level and risk of stroke: a systematic review and meta-analysis of prospective studies. J Stroke Cerebrovasc Dis. 2015; 24:2816–23.
Article35. Kim HS, Kim DJ, Yoon KH. Medical big data is not yet available: why we need realism rather than exaggeration. Endocrinol Metab (Seoul). 2019; 34:349–54.
Article36. Kim HS, Kim JH. Proceed with caution when using real world data and real world evidence. J Korean Med Sci. 2019; 34:e28.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cumulative Exposure to High γ-Glutamyl Transferase Level and Risk of Diabetes: A Nationwide Population-Based Study
- Asian Cohort Studies on Cardiovascular Risk Factors in Childhood
- The Cumulative Effect of Antipsychotic Usage on Mortality in Schizophrenia: A Nationwide Population-based Cohort Study in Korea
- The Triglyceride-Glucose Index Can Predict Long-Term Major Adverse Cardiovascular Events in Turkish Patients With High Cardiovascular Risk
- Cumulative Exposure to Metabolic Syndrome Components and the Risk of Dementia: A Nationwide Population-Based Study